Abstract
Osteoblastoma-like osteosarcoma is a rare, low-grade variant of osteosarcoma that may resemble osteoblastoma clinically, radiographically and histologically. We report a case of osteoblastoma-like osteosarcoma in the right proximal tibia in a 17-year-old woman. Plain radiography revealed an irregular osteolytic lesion in the metaepiphysis of the right proximal tibia and transverse fracture line of the metaphysic through an osteolytic lesion. MRI showed well-defined mass confined to the medullary space with cortical disruption and pathologic fracture. The MR signals were low on T1-weighted image and intermediate on T2-weighted image.
Osteoblastoma-like osteosarcoma is a rare, low-grade variant of osteosarcoma that may resemble osteoblastoma clinically, radiographically, and histologically and has been estimated to represent approximately 1% of osteosarcomas (1). Recently, reported involvements contain distal tibia, distal femur, proximal fibula and cuboid (1234). To our knowledge, there has been no documented radiologic report concerning proximal tibial involvement. Radiologists might be faced with the dilemma of diagnosis whether it is giant cell tumor or other tumor, especially for patients of a young age. We report a case of MR imaging of osteoblastoma-like osteosarcoma of the proximal tibia, which was pathologically confirmed.
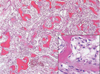
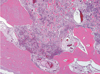
A 17-year-old woman presented to our hospital with persistent right knee pain for several months. The symptoms developed 4 months ago after she fell as a result of slipping. A physical examination revealed tenderness around the anteromedial aspect of the right knee. The limitation of the right knee motion range was not noted. In the laboratory, alkaline phosphatase was increased to 890 IU/L. Four years before, she had presented to our hospital with a valgus injury to her right knee joint after slipping. Mild osteopenic change was observed on plain radiography, but was otherwise unremarkable. MRI of the right knee reveals no discrete tumor lesion in the tibia, except for a focal medial collateral ligament tear at the femoral attachment site. The lesion could be suc cessfully treated without surgery. One year before, she returned to our hospital again with right knee pain. A plain radiography revealed focal disruption of the cortex at the proximal tibia and a slightly aggravated osteopenic lesion (Fig. 1). The radiologist and physician suspected the possibility of the tumor and recommended that she undergo an MRI for further evaluation; however, the patient refused. Several months later, a plain radiography revealed an irregular osteolytic lesion in the metaepiphysis of the right proximal tibia and transverse fracture line of the metaphysic through an osteolytic lesion. The border between the lesion and the adjacent medullary space was blurred and sclerotic band was not noted (Fig. 2). MRI showed a well-defined mass confined to the medullary space without significant cortical disruption except for a pathologic fracture. The MR signals were low on T1-weighted image and intermediate on T2-weighted image (Fig. 3). The lesion extended into the proximal end of the tibial epiphysis but definite cystic change was not noted. Significant periosteal reaction and soft tissue changes were not combined. The differential diagnosis, based on the MRI, included a giant cell tumor. Within several days, a wide incision biopsy was performed and osteoblastoma was diagnosed. The surgeon decided upon surgical intervention because the pathologic fracture was combined and he did not have confidence in the biopsy result. The en-bloc resection of the lesion and allogeneic bone graft was performed. The bone specimen consisted of a portion of the proximal tibia which measured 13 cm in length and the resection margin of bony shaft which was grossly free of tumor (Fig. 4). Microscopically, the tumor was composed of woven bone, trabeculae lined by plump osteoblastic tumor cells, and a stroma rich in vessels (Fig. 5). The tumor tissue permeated the periphery of the host bony trabeculae (Fig. 6).
Osteoblastoma-like osteosarcoma was first reported by Bertoni et al. in 1984. Seventeen cases of well-differentiated osteosarcomas that resembled osteoblastomas were reported. They reported no gender dominance and the most common site was the tibia (4 lesions, 25%). The clinical symptoms described were nonspecific and in cluded short-term pain (5). Our case showed persistent bone pain mimicking a ligament injury. If not adequately treated, this malignant tumor is capable of local recurrence and metastasis (6). Osteoblastoma-like osteosarcoma is characterized by a longer clinical history and less aggressive radiographic features than conventional osteosarcoma. Some investigators reported benign featured periosteal reaction and cortical disruption (1). The current case showed benign looking osteolytic lesion confined to the medulla and metaepiphyseal location. Joint extension of the lesion was not noted. In the case of the involvement of the proximal tibia, giant cell tumor and osteosarcoma are the most likely diagnosis considered especially in younger individuals. Our initial radiologic diagnosis was a giant cell tumor. An incision biopsy revealed osteoblastoma, but the surgeon and radiologist did not agree on the pathologic result because of somewhat different location and clinical characteristics. Tani et al. (3) reported that the precise diagnosis was made based on the histological findings only after the recurrence. The proliferation of osteoblasts with abundant bone or osteoid formation and vascular spaces between the bony trabeculae are typical histological features of osteoblastoma. Pathological differentiation from osteoblastoma is nearly impossible to make with limited tissue (e.g., needle biopsy), and may be impossible even with adequate tissue (5). Clinical features are not helpful (6). This radiological and pathologic dissociation lead more aggressive surgical intervention. En-bloc resection was performed on the current case. Bertoni et al (5) reported the histological differences in that osteoblastoma shows a low mitotic rate, well defined margins, and non-permeative bone growth. The tumor should also be differentiated from conventional osteosarcoma, which usually has a short clinical presentation, more aggressive radiographic findings, and high-grade histologic features (7). The permeative pattern seen histologically is a diagnostic indication of osteosarcoma (3). Recently Kumar et al. (4) reported high rate of recurrence if adequate surgical margins were not achieved in the two cases of the osteoblastoma-like osteosarcoma in the cuboid.
We report MR findings of a case of osteoblastoma-like osteosarcoma located in the proximal tibia. On the other hand, plain radiography revealed confined osteolytic lesion in the metaepiphysis and no periosteal reaction. MRI showed a well-defined mass confined to the medullary space with a pathologic fracture, low signals on a T1-weighted image, and an intermediate on T2-weighted image. MRI allows exact evaluation of the lesion extent and helps to establish a therapeutic plan.
Figures and Tables
Fig. 1
Initial anteroposterior radiograph reveals an irregular osteolytic lesion in the metaepiohysis of the proximal tibia.
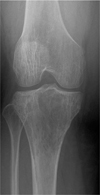
Fig. 3
A, B. Coronal T1 (TR 590, TE 15) and T2 (TR 4011, TE 100)-weighted MR image shows low and intermediate signal intensity lesion confined to the tibia.
C. Fat-suppressed axial T2-weighted image (TR 3200, TE 60) predominatly showing hyperintense lesion with clear circumscription and no prominent periosteal reaction.

Fig. 4
Photograph of the gross specimen shows the tumor, measuring 13 cm in length, in the tibia. The cut surfaces reveal relatively well circumscribed lesion abutting the articular cartilage. Grafted bone cement is present (arrow).

References
1. Abramovici L, Kenan S, Hytiroglou P, Rafii M, Steiner GC. Osteoblastoma-like osteosarcoma of the distal tibia. Skeletal Radiol. 2002; 31:179–182.
2. Bonar SF, McCarthy S, Stalley P, Schatz J, Soper J, Scoyler R, et al. Epiphyseal osteoblastoma-like osteosarcoma. Skeletal Radiol. 2004; 33:46–50.
3. Tani T, Okada K, Shoji K, Hashimoto M, Sageshima M. Osteoblastoma-like osteosarcoma. Skeletal Radiol. 2000; 29:656–659.
4. Kumar NL, Rosenberg AE, Raskin KA. Osteoblastoma-like osteosarcoma of the cuboid: a case report. J Orthop Surg Res. 2010; 5:52.
5. Bertoni F, Unni KK, Mcleod RA, Dahlin DC. Osteosarcoma resembling osteoblastoma. Cancer. 1985; 55:416–426.
6. Bertoni F, Bacchini P, Donati D, Martini A, Picci P, Campanacci M. Osteoblastoma-like osteosarcoma. The Rizzoli Institute experience. Mod Pathol. 1993; 6:707–716.
7. Dorfman HD, Weiss S. Borderline osteoblastic tumors: problems in differential diagnosis of aggressive osteoblastoma and low grade osteosarcoma. Semin Diagn Pathol. 1984; 1:215–234.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download