Abstract
Purpose
To evaluate the effectiveness of an additional transdermal fentanyl patch compared to intravenous analgesics in pain control during the 24-hour period following uterine artery embolization (UAE) for myoma and adenomyosis.
Materials and Methods
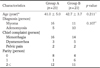
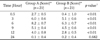
Between September 2009 and August 2010, 42 patients underwent UAE for myoma or adenomyosis. Of these, 21 received an intravenous opioid (pethidine) and a nonsteroidal anti-inflammatory drug (group A), and 21 received an additional transdermal fentanyl patch (group B). Pain perception levels were established verbally on a 0-10 scale during the 24-hour period following UAE. Differences in pain trends, mean dose of intravenous pethidine, and adverse effects were compared between the two groups.
Results
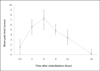
Pain perception was most severe at 6 hours after UAE and the mean pain level of group B at that time was 6.3 ± 0.7, which was significantly lower than that of group A, 8.2 ± 0.7 (p<0.05). The mean dose of intravenous pethidine was 114.3 ± 59.5 mg in group A and 90.5 ± 49.0 mg in group B, while the incidence of nausea was 67% in group A and 77% in group B. In both cases, the differences were not significantly different (p>0.05), and no evidence of respiratory distress was demonstrated.
Figures and Tables
Fig. 1
Successful uterine artery embolization in a 44-year-old patient with symptomatic adenomyosis.
A, B. Sagittal T2-weighted image (A) and fat suppressed gadolinium enhanced T1-weighted image (B) show the enlarged uterus with hyperintense foci in myometrium and intense contrast enhancement, suggestive of adenomyosis.
C. Follow-up sagittal fat suppressed gadolinium enhanced T1-weighted image four months after embolization shows near-complete infarction of adenomyosis in the uterine fundus with decreased volume.

Fig. 3
Difference of mean pain level between two groups by verbal rating scale during 24 hours after uterine artery embolization.
References
1. Ravina JH, Herbreteau D, Ciraru-Vigneron N, Bouret JM, Houdart E, Aymard A, et al. Arterial embolisation to treat uterine myomata. Lancet. 1995; 346:671–672.
2. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow-up. BJOG. 2002; 109:1262–1272.
3. Pron G, Bennett J, Common A, Wall J, Asch M, Sniderman K, et al. The ontario uterine fibroid embolization trial. part 2. uterine fibroid reduction and symptom relief after uterine artery embolization for fibroids. Fertil Steril. 2003; 79:120–127.
4. Spies JB, Bruno J, Czeyda-Pommersheim F, Magee ST, Ascher SA, Jha RC. Long-term outcome of uterine artery embolization of leiomyomata. Obstet Gynecol. 2005; 106:933–939.
5. Kim MD, Kim S, Kim NK, Lee MH, Ahn EH, Kim HJ, et al. Long-term results of uterine artery embolization for symptomatic adenomyosis. AJR Am J Roentgenol. 2007; 188:176–181.
6. Lohle PN, De Vries J, Klazen CA, Boekkooi PF, Vervest HA, Smeets AJ, et al. Uterine artery embolization for symptomatic adenomyosis with or without uterine leiomyomas with the use of calibrated tris-acryl gelatin microspheres: midterm clinical and MR imaging follow-up. J Vasc Interv Radiol. 2007; 18:835–841.
7. Pron G, Mocarski E, Bennett J, Vilos G, Common A, Zaidi M, et al. Tolerance, hospital stay, and recovery after uterine artery embolization for fibroids: the ontario uterine fibroid embolization trial. J Vasc Interv Radiol. 2003; 14:1243–1250.
8. Hehenkamp WJ, Volkers NA, Birnie E, Reekers JA, Ankum WM. Pain and return to daily activities after uterine artery embolization and hysterectomy in the treatment of symptomatic uterine fibroids: results from the randomized EMMY trial. Cardiovasc Intervent Radiol. 2006; 29:179–187.
9. Kim HS, Czuczman GJ, Nicholson WK, Pham LD, Richman JM. Pain levels within 24 hours after UFE: a comparison of morphine and fentanyl patient-controlled analgesia. Cardiovasc Intervent Radiol. 2008; 31:1100–1107.
10. Siskin GP, Bonn J, Worthington-Kirsch RL, Smith SJ, Shlansky-Goldberg R, Machan LS, et al. III. uterine fibroid embolization: Pain management. Tech Vasc Interv Radiol. 2002; 5:35–43.
11. Lampmann LE, Lohle PN, Smeets A, Boekkooi PF, Vervest H, van Oirschot CM, et al. Pain management during uterine artery embolization for symptomatic uterine fibroids. Cardiovasc Intervent Radiol. 2007; 30:809–811.
12. Kornick CA, Santiago-Palma J, Moryl N, Payne R, Obbens EA. Benefit-risk assessment of transdermal fentanyl for the treatment of chronic pain. Drug Saf. 2003; 26:951–973.
13. Nelson L, Schwaner R. Transdermal fentanyl: pharmacology and toxicology. J Med Toxicol. 2009; 5:230–241.
14. Minville V, Lubrano V, Bounes V, Pianezza A, Rabinowitz A, Gris C, et al. Postoperative analgesia after total hip arthroplasty: patient-controlled analgesia versus transdermal fentanyl patch. J Clin Anesth. 2008; 20:280–283.
15. Spies JB, Cooper JM, Worthington-Kirsch R, Lipman JC, Mills BB, Benenati JF. Outcome of uterine embolization and hysterectomy for leiomyomas: results of a multicenter study. Am J Obstet Gynecol. 2004; 191:22–31.
16. Goodwin SC, Bradley LD, Lipman JC, Stewart EA, Nosher JL, Sterling KM, et al. Uterine artery embolization versus myomectomy: a multicenter comparative study. Fertil Steril. 2006; 85:14–21.
17. Siskin GP, Shlansky-Goldberg RD, Goodwin SC, Sterling K, Lipman JC, Nosher JL, et al. A prospective multicenter comparative study between myomectomy and uterine artery embolization with polyvinyl alcohol microspheres: long-term clinical outcomes in patients with symptomatic uterine fibroids. J Vasc Interv Radiol. 2006; 17:1287–1295.
18. Bruno J, Sterbis K, Flick P, McCullough M, Cramp M, Murphy-Skrynarz K, et al. Recovery after uterine artery embolization for leiomyomas: a detailed analysis of its duration and severity. J Vasc Interv Radiol. 2004; 15:801–807.
19. Keyoung JA, Levy EB, Roth AR, Gomez-Jorge J, Chang TC, Spies JB. Intraarterial lidocaine for pain control after uterine artery embolization for leiomyomata. J Vasc Interv Radiol. 2001; 12:1065–1069.
20. Pisco JM, Bilhim T, Duarte M, Ferreira A, Santos D, Pires FM, et al. Pelvic pain after uterine artery embolization: a prospective randomized study of polyvinyl alcohol particles mixed with ketoprofen versus bland polyvinyl alcohol particles. J Vasc Interv Radiol. 2008; 19:1537–1542.
21. Ryu RK, Omary RA, Sichlau MJ, Siddiqi A, Chrisman HB, Nemcek AA Jr, et al. Comparison of pain after uterine artery embolization using tris-acryl gelatin microspheres versus polyvinyl alcohol particles. Cardiovasc Intervent Radiol. 2003; 26:375–378.
22. Rasuli P, Jolly EE, Hammond I, French GJ, Preston R, Goulet S, et al. Superior hypogastric nerve block for pain control in outpatient uterine artery embolization. J Vasc Interv Radiol. 2004; 15:1423–1429.
23. Nagao T, Ohwada T, Kitazono M, Ohshima K, Shimizu H, Katayama M. Thoracic epidural analgesia is effective in perioperative pain relief for uterine artery embolization. Masui. 2005; 54:156–159.
24. Ganguli S, Faintuch S, Salazar GM, Rabkin DJ. Postembolization syndrome: changes in white blood cell counts immediately after uterine artery embolization. J Vasc Interv Radiol. 2008; 19:443–445.
25. Sandler AN, Baxter AD, Katz J, Samson B, Friedlander M, Norman P, et al. A double-blind, placebo-controlled trial of transdermal fentanyl after abdominal hysterectomy. analgesic, respiratory, and pharmacokinetic effects. Anesthesiology. 1994; 81:1169–1118.
26. van Bastelaere M, Rolly G, Abdullah NM. Postoperative analgesia and plasma levels after transdermal fentanyl for orthopedic surgery: double-blind comparison with placebo. J Clin Anesth. 1995; 7:26–30.
27. Strupp C, Sudhoff T, Germing U, Hunerliturkoglu A, Schneider P, Niederste-Hollenberg A, et al. Transdermal fentanyl during high-dose chemotherapy and autologous stem cell support. Oncol Rep. 2000; 7:659–661.
28. Mantovani G, Curreli L, Maccio A, Massa E, Massa D, Mulas C, et al. Prevention of nausea and vomiting (N&V) in cancer patients receiving high-dose cisplatin. assessment of the potential antiemetic activity of transdermal fentanyl (TTS-F) compared to standard antiemetic treatment in acute and delayed N&V: first clinical report. Anticancer Res. 1999; 19:3495–3502.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download