Abstract
Recent introduction of image-guided percutaneous methods to treat unresectable bone tumors including metastases that do not respond to conventional radiotherapy or chemotherapy has proven to be effective. Here we present three successfully treated cases of metastatic bone lesions: two cases of malignant bone metastases in the lumbar spine and one in the sacral bone, using combined percutaneous radiofrequency ablation and percutaneous vertebroplasty/cementoplasty. A brief review of literature is also included.
Metastatic bone lesions are frequently found in cancer patients. Unfortunately, conventional treatments including radiotherapy as the treatment of choice, fail to alleviate pain in 20-30% of patients (1). Recently, percutaneous image-guided treatments were introduced for the treatment of benign and malignant bone tumors (1). The synergistic and additive effects of combined radiofrequency ablation (RFA) and percutaneous vertebroplasty (PVP)/cementoplasty have only been published in a few reports. We present 3 patients with metastatic bone lesions experiencing intractable pain treated with percutaneous RFA and PVP/cementoplasty with encouraging results.
A 59-year-old man diagnosed with hepatocelluar carcinoma (HCC) and treated by multiple transarterial chemoembolizations (TACE) developed lower back pain in December 2005. An osteolytic lesion in the L3 vertebral body which was not present on the initial computed tomography (CT) scan was detected. Magnetic resonance (MR) scan of the lumbar spine showed a 2.7 cm sized enhancing mass lesion involving the right L3 body showing T1 low and T2 high signal intensity (Figs. 1A-C). Cortical breakage of the adjacent lower endplate was combined. On February 2006, combined percutaneous radiofrequency ablation (RFA) and PVP was performed under local anesthesia. Intramuscular pethidine (Pethidine HCL 25 mg; Jeil Pharm, Daegu, Korea) and local lidocaine (Lidocaine HCL 400 mg; Huons Co. Ltd., Gyeonggi-do, Korea) was administered and the patient was placed in the prone position on a 64 channel multi-detector row CT table (Brilliance CT64; Philips Medical Systems, Cleveland, OH, USA). Before the ablation, we performed a coaxial needle biopsy with an 11-gauge disposable vertebroplasty needle (1-"J" Bone Marrow Needle; Angiotech - Manan Medical Products, Wheeling, IL, USA) and a 15-gauge/15 cm disposable biopsy needle (OSTYCUT; Angiomed GmbH & Co., Karlsruhe, Germany), via a right transpedicular approach. After removal of the biopsy needle, we inserted a 17-gauge/20 cm single cool-tip RF needle (Radionics, Burlington, MA, USA) with a 3 cm active electrode via the 11 gage vertebroplasty needle cannula, targeting the center of the L3 lesion (Fig. 1D). The energy of the electrode was controlled with a generator (Radionics) in the impedance-controlled mode with internal electrode cooling. The deployed energy, starting from 50 W, was increased manually by 10 W every 60 seconds up to 100 W, until tissue-impedance increased and further current flow was prevented (roll-off). The total ablation time was 10 minutes. Immediately after the RFA procedure was completed, the patient was transferred to a biplane angiosystem (Axiom Artis; Siemens, München, Germany). After further advancement of the pre-existing 11 gage vertebroplasty needle into the center of the lesion, 3 cc of polymethylmetacrylate (EXOLENT SPINE; Elmdown Ltd., London, UK) was injected via the vertebroplasty needle. Immediate follow-up radiographs and CT scan revealed homogeneous distribution of cement in the ablated metastatic lesion without leakage (Figs. 1E, F). Serial follow-up abdominal CT scans taken 3, 6, and 9 months after treatment showed constant cement-filled necrotic lesion in the right L3 body without evidence of local aggravation of the metastasis. Pain reduction was achieved and the patient reported an increase in spine stability. The treatment site remained stable without complication for 46 months.
A 49-year-old man was diagnosed with HCC on March 2006, and was treated with 5 sessions of TACEs until February 2007. A small osteolytic lesion in the 4th lumbar vertebral body was detected on the CT scan taken in June 2007. When compared with the previous CT taken 4 months earlier, the lesion appeared to have increased in size. MR scans of the spine revealed a 2 cm sized T2 high, T1 low signal diffusely enhancing lesion involving the right L4 body (Figs. 2A, B). Abnormal uptake at the lesion was detected on the whole body bone scan. The patient complained of lower back pain (visual analog scale (VAS) 9) and under the diagnosis of solitary spinal metastasis, combined percutaneous RFA and PVP was performed using similar procedures described in case 1. A 17-gauge/15 cm single cool-tip RF needle (Radionics) with a 2 cm active electrode was used for the percutaneous RFA procedure for a total of 6 minutes. Technical success was achieved in terms of complete ablation of the targeted tumor volume and cement filling of the targeted lesion (Figs. 2C, D). A total of 4 cc of polymethylmetacrylate was injected. Surrounding normal bone marrow was also filled with the injected cement, and minimal intradiscal cement leakage occurred into the L4/5 intervertebral disc (Fig. 2D). The follow-up CT scans acquired 3, 6, and 9 months after the procedure showed no evidence of further tumor progression. The patient experienced pain relief soon after undergoing the procedure (VAS 2). In fact, the metastatic lesion in the lumbar spine remained stable until the patient expired from complications of hepatic failure 1 year later.
A 67-year-old man was diagnosed with renal cell carcinoma in February 2008. Soon after receiving radical nephroureterectomy, the patient complained of lower back pain and metastatic lesions were uncovered in C7, T12, and the left sacrum. In spite of the subsequent repetitive radiotherapies issued, an adequate amount of pain reduction nor tumor size was achieved in the left sacral lesion (Figs. 3A, B). On April 2009, percutaneous RFA was performed targeting a 4 cm sized sacral metastatic mass using a 17-gauge/15 cm cool-tip RF needle (Radionics) with a 3 cm active electrode for 330 seconds at maximum power under the impedence controlled mode. Afterwards, cementoplasty using a 11-guage vertebroplasty needle was performed, delivering 8 cc of polymethylmetacrylate (EXOLENT SPINE; Elmdown Ltd.) under CT-fluoroscopy guidance (Brilliance CT64; Philips Medical Systems) (Figs. 3C-E). Instant relief of lower back pain was observed. Moreover, despite the fact that progression of multiple metastatic bone lesions were noted on the follow-up spine MR taken 8 months after the procedure, the left sacral lesion previously treated by combined RFA and cementoplasty showed no evidence of tumor progression.
Skeletal metastases commonly occur in patients with cancer, occurring most often in breast, prostate, or lung cancer and are usually located in the spine, pelvis, femur, skull, or other long bones where hematopoietic bone marrow proportions are high. The presence of metastatic bone lesions implies that the patients are in an advanced stage of cancer and frequently, palliative care including pain reduction and improvement of the patient's quality of life is the primary goal of treatment.
Conventional treatments include surgical resection, chemotherapy, radiation therapy, and analgesics. Although radiation therapy remains as the main standard therapy for cancer patients with bone metastasis, 20-30% of the patients do not achieve pain relief when treated by this method. Furthermore, many patients who do achieve pain relief after radiation therapy will experience a return of pain of the same or higher degree within a few months (1). Skeletal metastases are also at risk for impending fracture and consequently, stabilization for these lesions is also required.
Since its first introduction for treatment of spinal tumors by Dupuy et al. (2) on 2000, RFA has received much interest as an effective, minimally invasive alternative option for the treatment of bone metastasis. The multicenter study of Goetz et al. (3) found that 95% of patients had significant pain relief after RF ablation of bone metastases. PVP and cementoplasty are also indicated in bone metastasis: providing pain reduction, stabilization and strengthening of the affected bone (4). PVP is now a popular procedure with its well-known effects of cellular toxicity and internal stabilization (1). Combined RFA and PVP/cementoplasty for spinal osseous metastasis was first reported in 2002 (5), where subsequent delayed vertebroplasty was performed 3-7 days after RFA. Since then, several clinical trials combining RFA and PVP/cementoplasty have been reported (46789). Although only a few reports exist, all of them reported a one hundred percent rate of technical success, as well as significant (80-100%) and immediate pain relief. The mean duration of pain relief was 7.3 months in one study (6). By combining these two methods, complementary effects in treating metastatic bone lesions can be expected from the tumor necrosis effect of RFA, stabilization effect of PVP/cementoplasty, and additive pain relief effects from both methods (4689).
In all three cases, our patients were experiencing moderate to significant amounts of pain associated with the metastatic bone lesions despite receiving various treatments including radiation therapy. We successfully treated these lesions using combined percutaneous RFA and PVP/cementoplasty in one treatment session without any major complications. Two of the cases with solitary spinal metastasis showed almost curative effect for as long as 4 years until our latest follow-up in the 1st case, and for 1 year for the 2nd case, and the last case with sacral metastasis showed suitable palliative effect. For the 3rd case, we used CT-fluoroscopy guidance for cementoplasty because of the complex anatomy of the sacrum and also that CT-fluoroscopy would be a safer approach in introducing the RF needle. Although still less preferred than conventional fluoroscopic guidance due to greater radiation exposure and limited flexibility of work space, the authors believe that recent advancements in CT-fluoroscopy equipment could widen the use of CT-fluoroscopy in treating osseous metastasis with RFA, not only reducing the discomfort of transferring the patient from the CT unit to the fluoroscopy suite, but also providing more accurate anatomical detail. Unfortunately, the biopsy results performed in the first and second cases were inconclusive. But in both cases, radiographic evidence such as a newly appeared lesion which showed progressive growth in size and characteristic contrast enhancement, were substantial enough to assure the diagnosis of osseous metastasis.
It can be concluded that combined RFA and verterbroor cementoplasty provides almost instant pain relief and also bone strengthening in patients with metastatic bone lesions. Further clinical trials to determine its long-term effectiveness should be conducted in the future.
Figures and Tables
Fig. 1
RFA and combined percutaneous vertebroplasty of spinal metastasis in a 59-year-old man with hepatocelluar carcinoma. Sagittal T1 (A), T2 (B), and post-contrast fat suppressed T1 (C) - weighted images of the lumbar spine show a round mass lesion in the L3 body with T1 low, T2 heterogeneous high signal intensity, diffuse and prominent peripheral enhancement, representing a metastatic lesion. Axial CT scan during RFA (D) demonstrates the inserted RFA needle with a 3 cm active tip in the center of the lesion through the 11-gauge vertebroplasty cannula. Bone cement is well packed in the center of the metastatic lesion on the immediate prone AP view (E) and sagittal CT scan (F) after combined vertebroplasty.

Fig. 2
A 49-year-old man with hepatocelluar carcinoma and lumbar metastasis treated with RFA and combined percutaneous vertebroplasty. Axial T2 (A), T1 (B) - MR images show a heterogeneous T2 high, T1 low signal intensity mass with surrounding bone edema in the right side of the L4 body. Axial CT scan during RFA (C) demonstrates an inserted RFA needle with a 2 cm active tip in the center of the lesion. Immediate prone AP radiograph (D) shows injected cement in the lesion and surrounding bone marrow of the L4 body. Small amount of intradiscal cement leakage is seen (arrow).
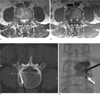
Fig. 3
Metastatic renal cell carcinoma involving the left sacrum in a 67-year-old man. Axial T1- (A), T2- (B) weighted MR images show an inhomogeneous T1 low, T2 high signal mass in left sacral ala with bone expansion. Axial CT scan during RFA (C) shows the needle inserted in the center of the left sacral lesion. Frontal (D) and lateral (E) radiographs taken after RFA and cementoplasty show well confinement of polymethylmetacrylate within the sacral mass lesion.

References
1. Callstrom MR, Charboneau JW, Goetz MP, Rubin J, Atwell TD, Farrell MA, et al. Image-guided ablation of painful metastatic bone tumors: a new and effective approach to a difficult problem. Skeletal Radiol. 2006; 35:1–15.
2. Dupuy DE, Hong R, Oliver B, Goldberg SN. Radiofrequency ablation of spinal tumors: temperature distribution in the spinal canal. AJR Am J Roentgenol. 2000; 175:1263–1266.
3. Goetz MP, Callstrom MR, Charboneau JW, Farrell MA, Maus TP, Welch TJ, et al. Percutaneous image-guided radiofrequency ablation of painful metastases involving bone: a multicenter study. J Clin Oncol. 2004; 22:300–306.
4. Hoffmann RT, Jakobs TF, Trumm C, Weber C, Helmberger TK, Reiser MF. Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease. J Vasc Interv Radiol. 2008; 19:419–425.
5. Gronemeyer DH, Schirp S, Gevargez A. Image-guided radiofrequency ablation of spinal tumors: preliminary experience with an expandable array electrode. Cancer J. 2002; 8:33–39.
6. Toyota N, Naito A, Kakizawa H, Hieda M, Hirai N, Tachikake T, et al. Radiofrequency ablation therapy combined with cementoplasty for painful bone metastases: initial experience. Cardiovasc Intervent Radiol. 2005; 28:578–583.
7. Schaefer O, Lohrmann C, Herling M, Uhrmeister P, Langer M. Combined radiofrequency thermal ablation and percutaneous cementoplasty treatment of a pathologic fracture. J Vasc Interv Radiol. 2002; 13:1047–1050.
8. Nakatsuka A, Yamakado K, Maeda M, Yasuda M, Akeboshi M, Takaki H, et al. Radiofrequency ablation combined with bone cement injection for the treatment of bone malignancies. J Vasc Interv Radiol. 2004; 15:707–712.
9. van der Linden E, Kroft LJ, Dijkstra PD. Treatment of vertebral tumor with posterior wall defect using image-guided radiofrequency ablation combined with vertebroplasty: preliminary results in 12 patients. J Vasc Interv Radiol. 2007; 18:741–747.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download