Abstract
Treatment for an enterovaginal fistula should consider the location of an intestinal fistula. Most rectovaginal fistulas develop in the lower third of the vagina and can be treated surgically. Jejunovaginal fistulas can spontaneously close during conservative management. We report the first use of the Amplatzer vascular plug II (AVP II; AGA Medical Corp, Golden Valley, MN, USA) and the use of an N-butyl-2-cyanoacrylate (NBCA; Histoacryl, Braun, Melsungen, Germany)-iodized oil (Lipiodol Ultra-Fluid, Guerbet, Aulnay-sous-Bois, France) mixture for treatment of a patient with a jejunovaginal fistula which failed to close after conservative management. The patient did not have any vaginal discharge one day later after deployment of the AVP II.
An enterovaginal fistula may result from obstetric complications, inflammatory bowel disease, pelvic malignancy, pelvic irradiation, pelvic surgery, or other traumatic causes (1234). Also, it may cause distressing symptoms including vaginal discharge with vaginitis, continual leakage of flatus and feces through the vagina, severe skin excoriation, as well as incontinence and dysparenunia. Treatment for an enterovaginal fistula depends on the location of intestinal fistula. Most rectovaginal fistulas develop at the lower third of the vagina can be treated surgically (5). Jejunovaginal fistulas can be expected to spontaneously close during conservative management.
The use of the Amplatzer vascular plug (AVP; AGA Medical, Golden Valley, MN, USA), a recently available embolic device derived from the Amplatzer septal occluder, has been shown to be safe and effective for the treatment of various cardiopulmonary vascular diseases. We report the first use of the AVP II and the use of an N-butyl-2-cyanoacrylate (NBCA)-lipiodol mixture for treatment of a patient with a jejunovaginal fistula which failed to close following conservative management.
Our case report is of a 44-year-old woman that had undergone a laparoscopic hysterectomy for uterine myoma three months prior. Three days after her surgery, the patient developed worsening abdominal pain. Two weeks later, the patient presented with a foul-smelling vaginal discharge and pelvic heaviness. A CT examination revealed intra-abdominal peritontitis such as the presence of intra-pelvic fluid collection, enhancement of the peritoneum, and engorgement of the mesenteric fat. An enterovaginal fistula was suspected and confirmed by a small bowel series and fistulogram which revealed a jejunovaginal fistula (Fig. 1).
The patient was treated with IV antibiotics, and insertion of drainage tube or gauzes packing the vagina for obliteration of the fistula tract. After prolonged hospitalization (two months), she refused the reoperation for closure of the fistula and was transferred to our institution for possible interventional therapy. We attempted to seal the anastomotic leak with an AVP II and NBCAlipiodol mixture due to her refusal to undergo reoperation and the possibility of AVP removal after technical failure. A 5-Fr catheter (Boston Scientific, Natick, MA, USA) with a 0.035-inch guidewire (GT; Terumo, Tokyo, Japan) was inserted through the vagina and inserted into the jejunum. A fistulogram that was performed through the catheter showed the fistula tract between the jejunum and vagina. The anastomotic leak lesion was treated by placing the AVP II with a diameter of 4 mm (Fig. 2). The all lobe of the AVP II was deployed into the fistula tract without protrusion into the vagina or ileum. A mixture of 1.0-cc lipiodol and 1.0-cc NBCA was injected through the microcatheter with its tip adjacent with the third lobe of the AVP II using a continuous injection technique (Fig. 2). After injection of the NBCA-lipiodol mixture, a fistulogram was performed to confirm the sealing of the jejunovaginal fistula. In addition, the fistulogram did not show abnormal communication between the vagina and jejunum. The patient did not have any vaginal discharge a day after deployment of the AVP II. However, three months later, a contrast-enhanced CT scan showed that the AVP II remained in the jejunovaginal fistula (Fig. 3) and a follow-up fistulogram did not show the tract between jejunum and vagina. The patient did not have any further symptoms.
Treatment method for an enterovaginal fistula should depend on the location of the instestinal fistula (i.e., rectovaginal fistula or ileo- or jejuno-vaginal fistula). Most rectovaginal fistulas develop at the lower third of the vagina and can easily be treated surgically. Several surgical procedures have been described for the treatment of fistulas, but none has been universally accepted as the procedure of choice. Among them include fecal diversion, primary repairs, endorectal advancement flap, transposition flaps, and various muscle flaps (567). Radiation-induced rectovaginal fistulas are characteristically high in position and show communication from the posterior fornix of the vagina to the middle third of the rectum (1). This type of fistula can rarely be treated surgically because of the difficult surgical approach and high recurrence rate. In particular, surgical treatment in patients with underlying Crohn's disease and previous radiation are associated with poor prognosis (5).
Treatment method for a jejunovaginal fistula depends on the degree of output, electrolyte balance, and nutrition. A low-output type (less than 500 cc of drainage per day), resulting in mild electrolyte disturbances could be managed conservatively leading to spontaneous resolution (4). However, a high-output type fistula and ensuing electrolyte imbalance could require surgical repair. In our case, although the fistula was of the low-output type without electrolyte imbalances, spontaneous closure of fistula was not achieved over two months. Therefore, alternative treatment such as surgical repair or an occlusion device was considered for closure of enterovaginal fistula.
Lee et al. (8) reported that new device fit for occlusion of the rectovaginal fistula was developed and consisted of a disk portion, an anchoring portion, and a connecting shaft. All devices were placed successfully, and all fistulas were completely occluded after placement of the device. However, we was used the AVP II for closure of a jejunovaginal fistula. The AVP is a woven nitinol wire cylinder that can be delivered through the guiding catheter or sheath. The AVP can be repositioned and can be redeployed multiple times prior to release, ensuring correct device positioning. The AVP II is a redesigned version of the original AVP with important modifications, which include a finer, more densely woven nitinol frame and a multi-segmented design.
We report our first experience with the AVP II for occlusion of a jejunovaginal fistula. The AVP II can be deployed in the fistula tract through a transvaginal approach. Following deployment of the AVP II at the fistula tract, the NBCA-lipiodol mixture was injected for complete obliteration of the densely woven nitinol frame. We thought that injection of the NBCA mixture into the AVP II would provide a compact barrier in the fistula, which would rapidly seal the jejunovaginal fistula. In our case, the NBCA-lipiodol mixture remained in the AVP II during the follow-up period and the time to occlusion of the jejunovaginal fistula was almost one day, in comparison with the long hospitalization of the patient.
We believe that the method described in this case report allows for a quick closure of a jejunovaginal fistula for which conservative management had failed. Prospective and preferably multicenter studies are needed to refine this technique further and to validate its clinical utility.
Figures and Tables
Fig. 1
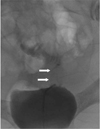
Fistulogram through a transvaginal approach shows the tract of the jejunovaginal fistula (arrows).
References
1. Andreani SM, Dang HH, Grondona P, Khan AZ, Edwards DP. Rectovaginal fistula in Crohn’s disease. Dis Colon Rectum. 2007; 50:2215–2222.
2. Taylor PM, Johnson RJ, Eddleston B, Hunter RD. Radiological changes in the gastrointestinal and genitourinary tract following radiotherapy for carcinoma of the cervix. Clin Radiol. 1990; 41:165–169.
3. Thorvinger B, Horvath G, Samuelsson L. CT demonstration of fistulas in patients with gynecologic neoplasms. Acta Radiol. 1990; 31:357–360.
4. Haddad BR, Usta IM, Khalil A, Mufarrij I. Spontaneous closure of enterovaginal fistula caused by a neglected foreign body. Acta Obstet Gynecol Scand. 1994; 72:598–600.
5. Zmora O, Tulchinsky H, Gur E, Goldman G, Klausner JM, Rabau M. Gracilis muscle transposition for fistulas between the rectum and urethra or vagina. Dis Colon Rectum. 2006; 49:1316–1321.
6. Boronow RC. Repair of the radiation-induced vaginal fistula utilizing the Martius technique. World J Surg. 1986; 10:237–248.
7. Zacharin RF. Grafting as a principle in the surgical management of vesicovaginal and rectovaginal fistulae. Aust N Z J Obstet Gynaecol. 1980; 20:10–17.
8. Lee BH, Choe DH, Lee JH, Kim KH, Hwang DY, Park SY, et al. Device for occlusion of rectovaginal fistula: clinical trials. Radiology. 1997; 203:65–69.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download