Abstract
Purpose
To evaluate the relationship between MR/epidurographic findings and the clinical outcome after a fluoroscopy-guided transforaminal epidural steroid injection (TFESI) in patients with cervical radicular pain.
Materials and Methods
Forty-five patients who had taken a cervical TFESI in our department were included in this study. We retrospectively reviewed MR and epidurographic findings to see if there was a relationship between these methods and the amount of pain relief, by way of a multiple regression analysis.
Results
On MR imaging, there was significant relationship between the amount of pain relief and location of herniated intervertebral disc (HIVD, central: 54.4%, lateral recess: 69.4%, foraminal: 59%; p = 0.048). There was no significant difference regarding the other MR findings. On epidurographic findings, there was significant difference in the amount of pain relief with the extent of the contrast (epidural and epineural space, 65.3%; epineural space only, 64.2%; p = 0.03) and location of the needle tip (in the foramen, 59.4%; outside the foramen, 68.4%; p = 0.002).
Conclusion
The results indicate that TFESI could be more useful in patients with cervical HIVD in lateral recess rather than another location. Contrast spread into epidural reflux appears to be a favorable injection pattern. Needle tip location is recommended outside the foramen rather than in the foramen.
Cervical transforaminal epidural steroid injections (TFESIs) play an important role in the conservative treatment of the symptoms of neck pain with a radicular component secondary to cervical herniated intervertebral disc (HIVD) or spinal stenosis (123). Although some investigators have reported no serious complications resulting from the use of cervical TFESIs, recent reports emphasize the risks of this procedure, including a high incidence of intravascular penetration (4) and serious brain and spinal cord injury (567). Therefore, it is important to consider the risks and benefits of TFESI.
MR imaging of the cervical spine combined with plain radiography represents the reference-standard examination for the work-up of patients with cervical radicular pain (89). Moreover, recent reports have attempted to evaluate whether MR imaging findings of the spine can predict the effectiveness of pain relief following epidural injections and assist in appropriate patient selection (101112).
Fluoroscopic needle placement and epidurographs with contrast can also provide visual confirmation of accurate needle placement and the distribution and extent of drug delivery during the procedure (131415). However the detailed techniques are not standardized and various epidurographic findings are observed during the procedure. The purposes of the present study were to evaluate which MR findings are indicators that a patient will likely benefit from cervical TFESI, and to suggest suitable epidurographic findings and needle position while performing the procedure.
Institutional review board approval and written informed consent were obtained for this study. Between January 2004 and August 2006, 51 consecutive patients (31 males and 20 females: mean age, 38 years; age range, 33-66 years) were treated at our department by cervical transforaminal epidural steroid injection (TFESI) for unilateral cervical radicular pain. All of 51 patients underwent cervical spine MR imaging before the injection (interval range, 1 day to 2 months). The indication for TFESI was unilateral cervical radicular pain without significant motor/sensory deficit. The level of the injection site was decided by consensus between an orthopedic surgeon and a musculoskeletal radiologist after considering the patient's history as well as the results of physical examinations, plain radiographs, MR imaging findings, and electrodiagnostic studies. In the case of bilateral cervical radicular pain, interlaminar ESIs were performed instead of TFESIs. Exclusion criteria were as follows: 1) clinically or MR documented myelopathy, 2) progressive neurological deficits, 3) recent epidural steroid injections, and 4) an allergic reaction to local anesthetics/contrast/corticosteroids or a blood coagulation disorder.
Forty-five of 51 patients (26 males and 19 females: mean age, 26 years; age range, 33-66 years) underwent a short-term follow-up within 1 month after the injection (mean interval, 18 days = 2.6 weeks; range, 7-28 days). Follow-ups for the remaining 5 of 51 patients were lost. All patients were requested to state their visual analogue scale (VAS) ranging from 1 to 10 at every visit before and after injection: the pain relief according to VAS after injection was calculated as a percentage (%) compared with that before injection.
All cervical TFESIs were performed as outpatient procedures by a musculoskeletal radiologist with experience in spinal interventions since March 2000. All procedures were performed in a sterile manner and under fluoroscopic guidance. Patients were placed in the supine position on the fluoroscopy table with the head turned to the asymptomatic side. The C-arm was rotated to an ipsilateral oblique angle with respect to the suspected foramen. Lidocaine (1%) was used for cutaneous and needle tract anesthesia. A 22-gauge spinal needle was aimed at a superior articular process to avoid the vertebral artery, before being introduced along the posterior border of the neural foramen. The C-arm was rotated to the anterior-posterior (AP) angle to confirm the depth of the needle. Epidurography was obtained by injecting 1-2 mL of Omnipaque 300 contrast material (OHEXOL, 300 mg of iodine per milliliter; Amersham Health, Princeton, NJ, USA). At least two AP epidurographs were obtained. After confirming contrast filling in the periradicular space in the absence of vascular filling, 0.5 mL of triamcinolone acetonide suspension (Triamcinolone 40 mg; Dongkwang, Seoul, Korea) was injected as a long-acting steroid after slowly injecting 0.3 mL of 0.2% ropivacaine (Naropin 0.2%; AstraZeneca, Westborough, MA, USA).
Cervical spine MR images were performed at our institution for all 45 patients using 1.0 T (Impact Expert; Siemens Medical Solutions, Erlangen, Germany) or 3.0 T (Intera Achieva 3T; Philips Medical Systems, Best, Netherlands) MR units. All MR images were retrospectively reviewed in consensus by two radiologists using a picture archiving and communication system (PACS) working station (Marosis M-view 4.0; Marotech, Seoul, Korea). The reviewers were informed of the patients' symptoms and the level of cervical TFESI. The MR findings were assessed at the level of the TFESI with regard to the causes, degree, and sites of nerve root compression, presence or absence of herniated intervertebral disc (HIVD), location of HIVD, and the presence or absence of foraminal/canal stenosis. The causes of nerve root compression were classified as HIVD, foraminal stenosis, or mixed. The degree of nerve root compression was classified as 1 (abutment), 2 (displacement), or 3 (entrapment) for intra-spinal canal lesions, and classified as 1 (foraminal encroachment < 1/3 foraminal diameter), 2 (1/3-1/2), or 3 (> 1/2) for a foraminal lesion. The sites of nerve root compression were classified as lateral recess or foraminal. Location of HIVD was classified as central, lateral recess, or foraminal. Foraminal stenosis was diagnosed when the findings of uncovertebral joint hypertrophy and encroachment of the neural foramen and spinal canal stenosis were diagnosed when the sagittal diameter of the cervical canal was 10 mm or less.
All epidurographic findings were retrospectively reviewed by the radiologist who had performed the TFESIs. The extent of contrast spread was classified based on the visualization of the contrast in the epidural space (both epidural and epineural spaces), or only in the epineural space (epineural space only) (Fig. 1). The location of the needle tip was evaluated, either in the foramen or outside the foramen on a frontal radiography.
A multiple regression analysis with a control for age, sex, and follow-up periods was performed to determine factors of MRI or epidurographic findings contributing to significant pain relief. Data were analyzed by using the SAS system for Windows 9.12 (SAS, Cary, SC, USA). A Pearson's correlation was used to evaluate the relationship among the variables.
Mean pain relief after cervical TFESI was 65% on VAS at short term follow-up (mean interval, 2.6 weeks; range, 7 - 28 days). Thirty-seven of 45 patients (82.2%) showed pain relief greater than 50% after cervical TFESIs at the same follow-up periods. Left-side injections were performed in 29 of 45 patients and right-side injections were performed in 16 patients. The most frequently injected level was C5-6 (23 patients): The C6-7 level was injected in 17 patients, while the C4-5 level was injected in 5 patients. There were no reported side effects of neurologic deficit, vertigo, seizure like motion, dural puncture, bleeding or infection.
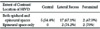
An MR analysis revealed a significant relationship between the degree of pain relief and the location of HIVD (central, 54.4 %; lateral recess, 69.4%; foraminal, 59%; p = 0.048) (Fig. 2). None of the other MR parameters were significantly associated with pain relief (Table 1).
An epidurography analysis revealed significant relationships between the degree of pain relief and extent of contrast (both epidural and epineural spaces, 65.3%; epineural space only, 64.2 %; p = 0.03) (Fig. 3) as well as the location of the needle tip (in the foramen, 59.4%; outside the foramen, 68.4 %; p = 0.002) (Table 2, Fig. 4). However, a Pearson's correlation test revealed a significant relationship between the location of HIVD and the extent of contrast, but there was no correlation between the location of HIVD and the location of the needle tip (Table 3). We also evaluated the relationship between the location of HIVD and extent of the contrast (Table 4), which revealed the tendency of the contrast medium to be confined to the epineural space in the foraminal locating disc herniation. However, the degree of pain relief was not affected by the extent of the contrast.
Two routes are commonly used for cervical epidural steroid injections: interlaminar and transforaminal injections. Although appropriate indications for both techniques are not standardized, interlaminar techniques are usually preferred in patients with bilateral radicular pain, while transforaminal techniques are preferred in patients with unilateral or foraminal disease. The transforaminal technique has a theoretical advantage in that it delivers the drug directly around the nerve root. However, following recent reports of the risks of TFESI (567), it is becoming increasingly necessary to conduct studies to assess which patients will most benefit from TFESI, regardless of the risk.
The present study identified a significant relationship between the location of the HIVD on MR images and the degree of pain relief after a TFESI. This result suggests that a TFESI can be more useful in patients with HIVD in the lateral recess rather than other HIVD locations or stenosis patients. In addition, nerve root compromise at the lateral recess showed greater pain relief compared to the foraminal level in the present study, even though the result was not statistically significant. In a similar study, Strobel et al. had reported that patients with foraminal disc herniation and foraminal nerve root compromise showed the greatest pain amount of relief immediately after a CT-guided cervical nerve root block (10). These results are not do not agree with those of the present study. We assume that this discrepancy was caused by the time difference after the injection. Because immediate pain relief is caused in most cases by the accompanying local anesthetics, a foraminal lesion is more likely to benefit immediately after transforaminal drug delivery, compared to a lateral recess or other intraspinal lesion; however, the effect of the local anesthetics decreases over time, and that of the steroid begins to act on the lesion. In the present study, we retrospectively reviewed the clinical outcome at short-term follow-up (mean, 2.6 weeks). Although these follow-up periods also do not represent long-term results, we consider that the outcomes of this period are crucial in deciding whether conservative treatment including repeat injections, should be maintained or not (16).
We also evaluated the relationship between the epidurographic findings and clinical outcome. Although all procedures were technically successful and 37 of 45 patients (82.2%) showed a successful outcome (pain relief greater than 50%) after a cervical TFESI at their short-term follow-up periods (mean, 2.6 weeks), contrast filling around the nerve with epidural reflux showed greater pain relief than epineural contrast filling alone in the present study. However, Pearson's correlation test revealed a significant relationship for extent of contrast, location of HIVD, and foraminal stenosis. In other words, in the cases with the foraminal stenosis or foraminal locating HIVD, there was a tendency for contrast filling to be limited in the epineural space only, rather than epidural reflux. Therefore, even though we could not say to what extent of contrast is the main predictive variable for the clinical outcome after cervical transforaminal ESI, but we could be sure that contrast spread in both the epidural and epineural spaces appears to be a favorable injection pattern while performing the procedure. In addition, the needle tip location outside the foramen showed greater pain relief rather than needle tip location in the foramen. This result was not significantly affected by other MR variables and could give us methodological grounds for depth of the needle location. The periradicular foraminal space is small and contains some fibrotic tissue. In particular, the superficial layer of the posterior longitudinal ligament is connected to the periradicular sheath anchoring the pedicle (17). When the needle tip is located in the small periradicular foraminal space, the contrast could initially collect on one side of the periradicular space without spreading to the other side around the nerve root. In addition, Ma et al. reported that the rate of complications associated with deep needle position on the frontal view was slightly higher than for a superficial needle position (18). In those circumstances, we can assert that the intentional introduction of the needle tip into the neural foramen has no clinical benefit and cannot be necessary.
The present study had several limitations. First, the follow-up periods of the patients after TFESI were not uniform and short because of the retrospective nature of this study. This is a major limitation of our study; however, the range was not wide (1-4 weeks), and most of the patients (43 of 45 patients) were followed-up within 2-3 weeks. To overcome this limitation, we treated the data statistically treated it by multiple regression analysis which can control the various follow-up periods. Second, multiple-level lesions were not considered; therefore the possibility of injection at the wrong level could not be excluded. Third, the amount of contrast material used in obtaining epidurographs was small, and lateral and oblique views were not routinely obtained; however, 2 cc of contrast or less is usually enough to confirm needle placement and drug delivery. We did not use a large amount of contrast during the procedure. Fourth, large population studies would be needed, because of small number of subjects in this study.
In conclusion, cervical TFESI can be useful in patients with cervical radicular pain. Among them, patients with MR revealed HIVD in the lateral recess gained the most significant benefit at the short-term follow-up after injection in the present study. Contrast spread in both the epidural and epineural spaces appears to be a favorable injection pattern while performing the procedure. In addition, it is recommended that the needle tip be located outside the foramen rather than in the foramen.
Figures and Tables
Fig. 1
Anterior-posterior (AP) projection epidurographs for the extent of contrast spread.
A. Visualization of the contrast both in the epidural and epineural spaces.
B. Contrast filling only in the epineural space.

Fig. 2
MRI and epidurography of a 39-year-old female patient with left posterior shoulder and arm pain.
A, B. T2-weighted sagittal (A) and T1-weighted axial (B) MR images show lateral recess HIVD (arrows) with grade III nerve root compression. The site of nerve root compression is at the lateral recess level.
C. Epidurography shows smooth contrast spread with contrast filling only in the epineural space. The needle tip is located outside the foramen. The patient achieved about 71% pain reduction, 2 weeks after a left C6 TFESI.

Fig. 3
MRI and epidurography of a 40-year-old female patient with left radiating pain.
A, B. T2-weighted sagittal (A) and gradient echo axial (B) MR images show foraminal HIVD (arrows). The degree of nerve root compression was graded I.
C. Epidurography shows smooth contrast spread with lateral epidural extension (curved arrow). The needle tip is located outside the foramen. The patient achieved about 80% pain reduction, 2 weeks after a left C5 TFESI.

Fig. 4
MRI and epidurography of a 53-year-old male patient with radicular pain on his right side.
A, B. T2-weighted sagittal (A) and gradient echo axial (B) MR images show uncovertebral joint hypertrophy with foraminal stenosis (arrows) and grade III nerve root compression in right C5-6.
C. Epidurography shows contrast spread with epidural extension (arrowheads). The needle tip is located in the foramen and the patient achieved about a 40% reduction in pain, 2 weeks after a right C6 TFESI.

Table 1
Association of MR findings and Pain Relief After a Cervical TFESI

Note.─ TFESI = transforaminal epidural steroid injection, NR = nerve root, HIVD = herniated intervertebral disc, CST = canal stenosis, FST = foraminal stenosis, LR = lateral recess, A = absence, P = presence, No. = number, Pts = patients. * Indicates a statistically significant value (p < 0.05, multiple regression analysis).
References
1. Slipman CW, Lipetz JS, Jackson HB, Rogers DP, Vresilovic EJ. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000; 81:741–746.
2. Bush K, Hiller S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996; 5:319–325.
3. Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004; 100:1595–1600.
4. Furman MB, Giovanniello MT, O'Brien EM. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine. 2003; 28:21–25.
5. Brouwers PJ, Kottnik EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001; 91:397–399.
6. Baker R, Dreyfuss P, MercerS , Bogduk N. Cervical transforaminal injection of corticosteoids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003; 103:211–215.
7. Scanlon GC, Moeller-Bertram T, Romanowsky SM, Wallace MS. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine. 2007; 32:1249–1256.
8. Boutin RD, Steinbach LS, Finnesey K. MR imaging of degenerative diseases in the cervical spine. . 2000; 8:471–490.
9. Brown MN, Schwartz RH, Frank E, Blank NK. Preoperative evaluation of cervical radiculopathy and myelopathy by surface-coil MR imaging. AJR Am J Roentgenol. 1988; 151:1205–1212.
10. Strobel K, Pfirrmann CW, Schmid M, Hoder J, Boos N, Zanetti M. Cervical nerve root blocks: indications and role of MR imaging. Radiology. 2004; 233:87–92.
11. Choi SJ, Song JS, Kim C, Ryu DS, Ahn JH, Jung SM, et al. The use of magnetic resonance imaging to predict the clinical outcome of non-surgical treatment for lumbar intervertebral disc herniation. Korean J Radiol. 2007; 8:156–163.
12. Jeong HS, Lee JW, Kim SH, Myung JS, Kim JH, Kim JH, et al. Effectiveness of transforaminal epidural steroid injection by using a preganglionic approach: a prospective randomized controlled study. Radiology. 2007; 245:584–590.
13. Johnson BA, Schellhas KP, Pollei SR. Epidurography and therapeutic epidural injections: technical considerations and experience with 5334 cases. AJNR Am J Neuroradiol. 1999; 20:697–705.
14. Manchikanti L, Cash KA, Pampati V, McManus CD, Damron KS. Evaluation of fluoroscopically guided caudal epidural injections. Pain Physician. 2004; 7:81–92.
15. Botwin KP, Natalicchio J, Hanna A. Fluoroscopic guided lumbar interlaminar epidural injections: a prospective evaluation of epidurography contrast patterns and anatomincal review of the epidural space. Pain Physician. 2004; 7:77–80.
16. Boswell MV, Shah RV, Everett CR, Sehgal N, McKenzie Brown AM, Abdi S, et al. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005; 8:1–47.
17. Kubo Y, Waga S, Kojima T, Matsubara T, Kuga Y, Nakagawa Y. Microsurgical anatomy of the lower cervical spine and cord. Neurosurgery. 1994; 34:895–902.
18. Ma DJ, Gilula LA, Riew KD. Complications of fluoroscopically guided extraforaminal cervical nerve blocks. An analysis of 1036 injections. J Bone Joint Surg Am. 2005; 87:1025–1030.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download