Abstract
Multiple cavernous hemangiomas with fluid-fluid levels were presented in a 40-year-old male patient. These hemangiomas showed nonspecific radiologic features on ultrasound and computed tomography, but gadolinium-enhanced magnetic resonance imaging (MRI) with subtraction revealed fluid-fluid levels with unique and different enhancement of the inferior and superior layer. This is the first case report of cavernous hemangiomas with fluid-fluid levels, containing radiologic features of dynamic MRI with subtraction.
The radiologic features of hemangiomas are well established. The diagnostic features on contrast enhanced computed tomography (CT) or magnetic resonance imaging (MRI) include peripheral globular and gradual centripetal enhancement. In most cases, hemangiomas do not require a pathological examination. However, some hemangiomas show atypical radiologic features, such as poor gradual enhancement on sclerosing or hyalinized hemangioma and a fluid-fluid level within a hemangioma (1). The radiologic diagnosis of hemangioma with a fluid-fluid level remains problematic because the typical enhancement pattern of hemangioma is not found on CT and a fluid-fluid level can be reported in various hepatic lesions from malignant to benign tumors (23). Recently, the gadolinium-enhanced dynamic MRI with subtraction has been introduced as a highly sensitive method in the depiction of a vascular pattern and subtle enhancement of focal hepatic lesions (45). To the best of our knowledge, there has been no report about the imaging feature of dynamic MRI with subtraction in a hemangioma with a fluid-fluid level. Herein, multiple cavernous hemangiomas with fluid-fluid levels in a patient are presented.
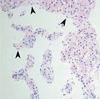
A 40-year-old man was referred for hepatic nodules detected on a routine health checkup. The man had no specific medical history or laboratory findings. Ultrasound (US) revealed three well-defined echogenic nodules in the right lobe of his liver (Fig. 1A). Their diameters were less than 2 cm (range; 0.9-2 cm). On multiphase enhanced CT, these nodules showed nonspecific subtle enhancement in three phases and subtle single layered attenuation difference between the inferior and superior layer. The inferior layer of all nodules showed higher attenuation than that of the superior layer (Fig. 1B). On heavily T2-weighted MRI (TR/TE, 1200/462), the superior layer showed bright signal intensity (SI), similar to cerebrospinal-fluid, whereas the inferior layer showed slightly higher SI than that of adjacent normal liver parenchyma (Fig. 2A). Another heavily T2-wighted MRI was performed in the prone position, and the SI of these nodules was presented vice versa (Fig. 2B). These findings suggested fluid-fluid level in all nodules. T1-weighted gadoxetate-enhanced dynamic MRI were obtained immediately, 1 min, 3 min, 5 min, 10 min, 15 min, and 20 min after contrast injection with a patient's breath-holding in a reproducible manner. Nodules showed low SI compared with the adjacent normal liver parenchyma as well as no perceptible nodule enhancement without subtraction. After subtraction, which maximizes the qualitative recognition of enhancement, the inferior layer showed centripetal globular enhancement at 1 min after injection and gradually increasing enhancement until the 15 min delayed image. The superior layer did not reveal enhancement on 1 min delayed image. However, subtle enhancement was seen in the superior layer on 3 min image and progressive enhancement persisted until 15 min (Figs. 2C-F). Percutaneous needle biopsy was performed in the largest nodule. The histopathologic examination showed a typical cavernous hemangioma composed of dilated vascular spaces lined by a single layer of endothelial cells with intervening fibrous stroma (Fig. 3).
The cavernous hemangioma is the most common benign tumor of the liver. It is composed of dilated vascular spaces lined by a single layer of endothelial cells and separated by connective tissue stroma (67). A definite diagnosis could be made by demonstrating the typical US, CT, and MRI findings (1). The fluid-fluid level has been described in variable types of focal hepatic lesions such as complicated cysts, abscesses, chronic hematomas, biliary cystadenomas, tumors with liquefactive necrosis or hemorrhage, and necrotic metastases (23). The fluid-fluid level within a hepatic hemangioma has been rarely reported (238910). All reported cases with a fluid-fluid level in hemangiomas were easily depicted on CT and MRI (238910). US usually did not identify fluid-fluid levels because of background echogenicity, but fluid-fluid levels were demonstrated on US in one case reported by Ghai et al. (9). In our case, fluid-fluid levels were not seen on US, suspected on CT, and were clearly depicted on MRI. The formation of fluid-fluid level in hemangioma has been explained by a sedimentation effect (238910). Slow blood flow or stagnant blood in a large intercommunicating vascular pool baffled by incomplete septation results in the sedimentation of blood cells within the serum, thereby forming a fluid-fluid layer within the hemangioma (9). The superior layer consists of serum and the inferior layer consists of sedimentary blood cells (238910). This theory well explains the unique SI of a hemangioma with a fluid-fluid level on MRI.
In reported cases, only one demonstrated the shift of a fluid-fluid level in a hemangioma according to a change in position of the patient (9). In our case, prone-positioned, heavily T2-weighted MR showed the shift of a fluid-fluid level in all three hemangiomas. There was a case of hemangioma which did not show the shift of a fluid-fluid level and the author's explanation was that the images were obtained immediately after change of patient's position and did not yet reveal the fluid-fluid level (2). We think that a change of the fluid-fluid interface in hemangiomas might be limited by numerous incomplete septations and may also be affected by blood viscosity the time interval of the position change.
Accurate assessment of the enhancement pattern is crucial to the diagnosis of the hemangioma. However, the determination of the amount of contrast enhancement is not always easy to accomplish for relatively subtle enhancing lesions on dynamic contrast-enhanced CT and even on contrast-enhanced T1 weighted MRI (410). Previous studies have shown that the dynamic subtraction MRI increases the sensitivity and specificity of the hepatic mass by depicting the subtle enhancement and providing information on the enhancement pattern of the hepatic masses (410). Soyer et al. demonstrated enhancement patterns of hemangiomas on subtraction MRI, which were high intensity relative to the hepatic parenchyma on arterial phase and progressive enhancement on the delayed phase (4). The previously reported cases of hemangiomas with fluid-fluid levels showed variable enhancement patterns such as absence of enhancement (2), relatively delayed peripheral nodular enhancement with centripetal progression (810), and early subtle peripheral enhancement with centripetal progression (9). In the present study, subtraction MRI with a 1, 3 and 10 min delay after contrast injection revealed nodular and progressive enhancement of the inferior layer. Subtraction MRI also depicted a subtle enhancement of the superior layer with gradual filling. The enhancement pattern of the two layers was similar, but there was a time gap for the enhancement between the two layers. This enhancement pattern was unique and not reported in previous articles and was not seen in multiphase enhanced CT and even in conventional MRI without subtraction. We postulated that the time gap for the contrast enhancement between the two layers was due to the combination of the sedimentation effect and slow diffusion of contrast into the superior fluid layer from the inferior layer by a widely disseminated intercommunicating vascular channel.
In conclusion, the dynamic MRI with subtraction may play a diagnostic role in hemangiomas with a fluid-fluid level and might be helpful for the differentiation of hemangiomas from other hepatic masses with a fluid-fluid level.
Figures and Tables
Fig. 1
A 40-year-old man with three hepatic hemangiomas with fluid-fluid levels.
A. US shows a well-defined homogeneously hyperechoic nodule in the right lobe of liver. No fluid-fluid levels were demonstrated for all three lesions.
B. Dynamic contrast enhanced CT at portal phase shows well-defined low density nodules with layered attenuation differences, which suggest fluid-fluid levels.

Fig. 2
MRI of the largest hemangioma with a fluid-fluid level.
A. Heavily T2-weighted MR image (TR/TE, 1200/462) obtained in the supine position clearly depicts a fluid-fluid level within the hemangioma.
B. On prone position, the heavily T2-weighted MR image shows the shift of the fluid-fluid level.
C. T1-weighted 3D dynamic MR image without enhancement shows a low signal intensity (SI) nodule with a fluid-fluid level. The superior layer shows lower SI than the inferior layer.
D-F. Subtraction MR images obtained 1, 3, and 10 min after injection of contrast medium shows centripetal globular enhancement of the inferior layer (arrow). The superior layer shows subtle enhancement on the 3 min delayed image (arrowhead in E) and gradual filling on the 10 min (arrowhead in F) delayed image. There is a time gap of enhancement between the two layers.

References
1. Vilgrain V, Boulos L, Vullierme MP, Denys A, Terris B, Menu Y. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics. 2000; 20:379–397.
2. Itai Y, Ohtomo K, Kokubo T, Yamauchi T, Okada Y, Makita K. CT demonstration of fluid-fluid levels in nonenhancing hemangiomas of the liver. J Comput Assist Tomogr. 1987; 11:763–765.
3. Soyer P, Bluemke DA, Fishman EK, Rymer R. Fluid-fluid levels within focal hepatic lesions: imaging appearance and etiology. Abdom Imaging. 1998; 23:161–165.
4. Soyer P, Spelle L, Gouhiri MH, Rondeau Y, Pelage JP, Scherrer A, et al. Gadolinium chelate-enhanced subtraction spoiled gradient-recalled echo MR imaging of hepatic tumors. AJR Am J Roentgenol. 1999; 172:79–82.
5. Ward J, Guthrie JA, Scott DJ, Atchley J, Wilson D, Davies MH, et al. Hepatocellular carcinoma in the cirrhotic liver: double-contrast MR imaging for diagnosis. Radiology. 2000; 216:154–162.
6. Tung GA, Vaccaro JP, Cronan JJ, Rogg JM. Cavernous hemangioma of the liver: pathologic correlation with high-field MR imaging. AJR Am J Roentgenol. 1994; 162:1113–1117.
7. Yamashita Y, Ogata I, Urata J, Takahashi M. Cavernous hemangioma of the liver: pathologic correlation with dynamic CT findings. Radiology. 1997; 203:121–125.
8. Obata S, Matsunaga N, Hayashi K, Ohtsubo M, Morikawa T, Takahara O. Fluid-fluid levels in giant cavernous hemangioma of the liver: CT and MRI demonstration. Abdom Imaging. 1998; 23:600–602.
9. Ghai S, Dill-Macky M, Wilson S, Haider M. Fluid-fluid levels in cavernous hemangiomas of the liver: baffled? AJR Am J Roentgenol. 2005; 184:3 Suppl. S82–S85.
10. Lee J, Lim HK, Jeon YH. Multiple hepatic hemangiomas with fluid-fluid levels. Australas Radiol. 2007; 51:Suppl. B310–B312.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download