Abstract
Purpose
We evaluated the effectiveness of performing fluoroscopic and ultrasonography guided percutaneous catheter drainage (PCD) through the anterolateral transabdominal approach for treating iliopsoas abscess.
Materials and Methods
From January 2008 to December 2009, fluoroscopic and US-guided PCD through the anterolateral transabdominal approach was performed on sixteen iliopsoas abscesses of fourteen patients (7 males and 7 females; mean age: 63 years; age range: 30-87 years). Six abscesses were on the right side and ten abscesses were on the left side. The location of the abscesses were the psoas muscle (n=7), the iliacus muscle (n=7) and the iliopsoas muscle (n=2). All the procedures were performed under fluoroscopy and US guidance in the angiography room. The clinical findings before and after the procedure, the duration of catheter insertion and the procedure-related complications were evaluated.
Results
15 out of the 16 iliopsoas abscesses were effectively treated. The duration of catheter insertion was 5-27 days (mean: 14.6) days. No patient had significant complications during or after drainage. One patient died of uncontrolled diabetes complications and shock on the 9th day after percutaneous catheter drainage. One recurrence was noted 5 months after removal of the catheter. This patient underwent aspiration and antibiotic treatment for this lesion and the patient improved.
Figures and Tables
Fig. 1
A 74-years-old woman with low abdominal and back pain.
A-C. Axial and coronal CT scan shows both iliopsoas abscesses, right psoas abscess was septated.
D. Percutaneous drainage catheters were inserted in the both iliopsoas abscesses using anterolateral transabdominal approach.
E. Additional catheter was inserted in the right upper septated psoas abscess. Posterior approach was used in this procedure on prone position.

Fig. 2
Schematic drawings of US-guided anterolateral transabdominal approach.
A. Left iliopsoas abscess was overlaid with small bowel.
B. Compression of left lateral abdomen by US probe translocate the overlaid small bowels medially, and then psoas abscess could be punctured by needle.
C, D. On the sagittal views, compression of lower abdomen by US probe could translocate the overlaid bowels to the upper side.

Fig. 3
A 68-years-old man with low back pain.
A, B. Axial and coronal CT scan shows low density abscess in the left iliopsoas muscle and another low density abscess in right gluteus muscle.
C. Ultrasonography on the left lower lateral abdomen shows high echoic abscess in the left iliac muscles.
D. 22G Chiba needle was inserted into left iliopsoas abscess through left lower lateral abdomen.
E. Abscess cavity was partially outlined by contrast materials and guide wire was inserted in the abscess cavity.
F. 10.2F drainage catheter was inserted successfully.

Fig. 4
A 46-years-old man with left flank pain.
A. CT scan shows mild swelling and poorly enhanced left kidney with perirenal fluid collections that suggested acute pyelonephritis.
B. CT scan of psoas muscle level shows low density abscess cavity at left iliopsoas muscle.
C. Fluroscopic image after PCD shows abscess cavity which is partially filled with contrast materials.
D. One month follow up CT scan shows complete resolution of previously noted left iliopsoas abscess.
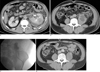
Table 1
Characteristics and Underlying Diseases of the Study Subjects and Cultured Microorganisms

Note.─ DM = diabetes mellitus, ESRD = end stage renal disease, PMHx = past medical history, PI = present illness, OP = operation, APN = acute pyelonephritis, S.aureus = Staphylococcus aureus, MRSA = methicillin-resistant Staphylococcus aureus, K.pneumoniae = Klebsiella pneumoniae, V.streptococcus = Viridance streptococcus, E.coli = Escherichia.coli
References
1. Dinc H, Onder C, Turhan AU, Sari A, Aydin A, Yulug G, et al. Percutaneous drainage of tuberculous and nontuberculous psoas abscesses. Eur J Radiol. 1996; 23:130–134.
2. Muller PR, Ferrucci JT Jr, Wittenberg J, Simeone JF, Butch RJ. Iliopsoas abscess : treatment by CT-guided percutaneous catheter drainage. AJR Am J Roentgenol. 1984; 142:359–362.
3. Gupta S, Suri S, Gulati M, Singh P. Ilio-psoas abscess. Percutaneous drainage under image guidance. Clin Radiol. 1997; 52:704–707.
4. Pombo F, Martin-Egana R, Cela A, Diaz JL, Linares-Mondejar P, Freire M. Percutaneous catheter drainage of tuberculous psoas abscesses. Acta Radiol. 1993; 155:366–368.
5. Cantasdemir M, Kara B, Cebi D, Selcuk ND, Numan F. Computed tomography-guided percutaneous catheter drainage of primary and seconddary iliopsoas abscess. Clin Radiol. 2003; 58:811–815.
6. Gupta S, Nguyen HL, Morello FA Jr., Ahrar K, Wallace MJ, Madoff DC, et al. Various approaches for CT-guided percutaneous biopsy of deep pelvic lesions: anatomic and technical considerations. Radiographics. 2004; 24:175–189.
7. Maher MM, Gervais DA, Kalra MK, Lucey B, Sahani DV, Arellano R, et al. The inaccessible or undrainable abscess: how to drain it. Radiographics. 2004; 24:717–735.
8. Tanomkiat W, Buranapanitkit B. Percutaneous drainage of large tuberculous iliopsoas abscess via a subinguinal approach: a report of two casces. J Orthop Sci. 2004; 9:157–161.
9. Ralls PW, Boswell W, Henderson R, Rogers W, Boger D, Halls J. CT of inflammatory disease of the psoas muscle. AJR Am J Roentgenol. 1980; 134:767–770.
10. Sheikh M, Al-Ali AA, Al-Sumait B, Behbehani A. CT-guided percutaneous drainage of tuberculous and non-tuberculous deep pelvic abscesses. Med Princ Pract. 2000; 9:52–58.
11. Desandre AR, Cottone FJ, Evers ML. Iliopsoas abscess: etiology, diagnosis and treatment. Am Surg. 1995; 61:1087–1091.
12. Gruenwald I, Abrahamson J, Cohen O. Psoas abscess: case report and review of the literature. J Urol. 1992; 147:1624–1626.
13. Ricci MA, Rose FB, Meyer KK. Pyogenic psoas abscess: worldwide variations in etiology. World J Surg. 1986; 10:834–843.
14. Harris LF, Sparks JE. Retroperitoneal abscess: case report and review of the literature. Dig Dis Sci. 1980; 25:392–394.
15. Santaella RO, Fishman EK, Lipsett PA. Primary vs secondary iliopsoas abscess: presentation, microbiology, and treatment. Arch Surg. 1995; 130:1309–1313.
16. 2005. 68:205–210.
17. Lobo DN, Dunn WK, Iftikhar SY, Scholefield JH. Psoas abscess complicating colonic disease: imaging and therapy. Ann R Coll Surg Engl. 1998; 80:405–409.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download