Abstract
Bronchogenic cysts are developmental anomalies of the primitive foregut. They are usually located in the mediastinum along the trachobronchial tree, but they can be found at unusual locations, including the abdominal cavity. We experienced a case of a pathologically confirmed bronchogenic cyst that was located in the subphrenic space. We present here the CT findings of this unusual case and we review the relevant literature.
Bronchogenic cysts are rare congenital anomalies that are most frequently located in the mediastinum along the trachebronchial tree (1). However, they may arise in many other locations, and intrapulmonary, intrapericardial, abdominal and retroperitoneal locations have been reported (12). A subphrenic location of bronchogenic cysts is extremely rare and only about 60 such cases have been reported in the English medical literature. We report here on a case of a subphrenic brochogenic cyst and we review the relevant literature.
A 43-year-old man underwent a medical check-up and the computed tomography (CT) showed a left subphrenic mass. He was referred to our hospital for further evaluation. The patient had no specific symptoms related to the subphrenic mass. The physical examination showed unremarkable features, and the results of the laboratory examination were normal.
The contrast-enhanced computed tomography (CT) scans showed a well-defined round solid mass about 2.7 × 2.6 × 2.1 cm in size and it was located in the left subphrenic space. This mass had homogeneous attenuation of 63 Hounsfield units (HU) and this was higher than the attenuation of the skeletal muscle on the unenhanced CT scan. After injection of contrast material, there was no enhancement. Any distinct enhancing component or septi were not showed on the enhanced CT scan and no signs of infliltrative change were noted in the surrounding fat (Figs. 1A-C).
From these CT findings, we suspected an epidermoid cyst, lymphangioma, non-pancreatic pseudocyst, cystic neurogenic tumor and lymphadenopathy for the possible differential diagnosis.
Surgical exploration was performed even though the clinical manifestations and CT findings indicated that this was probably a benign mass. On the operative findings, the mass had a soft and cystic nature and it was located in the subphrenic space. The cystic mass contained a whitish viscid material. Histologic examination revealed that the cystic mass was a unilocular cyst, and the inner wall of cyst was lined by ciliated pseudostratified columnar epithelium (Fig. 1D). The pathological report confirmed this was a bronchogenic cyst.
A bronchogenic cyst is a unilocular cystic mass of non-functioning pulmonary tissue and this mass is composed of smooth muscle, cartilage and glands, and it is lined with ciliated columnar epithelium (2). Embryologically, it is thought to be a result of an abnormal budding of the tracheobronchial analogue of the primitive foregut in early development (3). When an attachment to the primitive foregut persists, the cyst is associated with the trachobronchial tree or esophagus. However, complete separation can give rise to unusual locations (4). The thoracic and abdominal cavities, which are linked by the pericardioperitoneal canal in an early embryonic stage, are divided by fusion of the future components of the diaphragm at the end of the sixth week of intrauterine life (5). Although the exact mechanism of subphrenic bronchogenic cyst is unclear, it has been suggested that a subphrenic bronchogenic cyst is formed when abnormal buds of the tracheobronchial tree are pinched off by these membranes and these buds migrate into the abdominal cavity (6). In most cases, like their counterparts in the throacic cavity, they are diagnosed incidentally without symptoms unless they are become secondarily infected, perforated or large enough to compress the adjacent organs (1)
On CT examination, bronchogenic cysts are typically rounded, well-circumscribed, hypoattenuating cysts (near water density: 0-20 HU) without enhancement. However, they often appear as a highly attenuated mass on CT (30-100 HU), as in the present case, because of the elevated levels of calcium and anthracotic pigment or the high protein content of the cystic fluid (789). On MR imaging, the cyst shows from intermediate to high signal intensity on T1-weighted images. This intermediate to high signal intensity may be related to the presence of a high content of protein, methemoglobin, mucus or debris (10)
In our case, the tumor's unusual subphrenic location and hyperattenuating internal contents led to confusion when making the radiologic diagnosis. Even though a subphrenic location and high attenuation are unusual, bronchogenic cyst should be included in the differential diagnosis of a subphrenic round homogeneous mass.
Figures and Tables
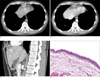 | Fig. 1Subphrenic bronchogenic cyst in a 43-year-old man.The unenhanced CT scan (A), the enhanced CT scan (B) and the coronal reformatted CT images (C) reveal a well-defined homogeneous hyperattenuating mass without contrast enhancement (arrow). The mass is located exactly under the diaphragm.
Microscopic examination (D) shows that the cystic chamber is lined by pseudostratified tall columnar ciliated epithelium (H & E, ×200).
|
References
1. Haddon MJ, Bowen A. Bronchopulmonary and neuroenteric forms of foregut anomalies: imaging for diagnosis and management. Radiol Clin North Am. 1991; 29:241–254.
2. Foerster HM, Sengupta EE, Montag AG, Kaplan EL. Retroperitoneal bronchogenic cyst presenting as an adrenal mass. Arch Pathol Lab Med. 1991; 115:1057–1059.
3. Kim YC, Goo JM, Han JK, Lee KH, Lee HS, Im JG. Subphrenic bronchogenic cyst mimicking a juxtaphrenic solid lesion. Abdom Imaging. 2003; 28:354–356.
4. Kural YB, Ergun S, Buyukbabani N, Durmusouglu R, Onsun N. Cutaneous bronchogenic cysts. Int J Dermatol. 1998; 37:137–140.
5. Moore KL. Body cavities, primitive mesenteries, and diaphragm. the developing human. 3rd ed. Philadelphia: WB Saunders;1982. 31:p. 167–170.
6. Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985; 408:93–98.
7. Nakata H, Sato Y, Nakayama T, Yoshimatsu H, Kobayashi T. Bronchogenic cyst with high CT numbers: analysis of contents. J Comput Assist Tomogr. 1986; 10:360.
8. Mendelson DS, Rose JS, Efremidis SC, Kirschner PA, Cohen BA. Bronchogenic cysts with high CT numbers. AJR Am J Roentgenol. 1983; 140:463–465.
9. Yernault JC, Kuhn G, Dumotier P, Rocmans P, Ketelbant P, DeVuyst P. "Solid" mediastinal bronchogenic cyst: mineralogic analysis. AJR Am J Roentgenol. 1986; 146:73–74.
10. Nakata H, Egashira K, Watanabe H, Nakamura K, Onitsuka H, Murayama S, et al. MRI of bronchogenic cysts. J Comput Assist Tomogr. 1993; 17:267–270.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download