Abstract
Purpose
To evaluate the occurrence of superficial femoral artery stent fractures, the risk factors of stent fracture, and the relationship between fractures and clinical findings.
Materials and Methods
Of the 38 patients who underwent treatment with Protégé GPS stenting due to arterial occlusions on the superficial femoral artery, 17 also underwent a clinical analysis. Forty-three stents were inserted in the 17 superficial femoral arteries, ranging between 15 and 50 cm in length, with a mean treated length of 26.4 cm (15-50 cm). A fracture was evaluated by taking a PA and lateral simple radiography, as well as a follow-up evaluation accompanied with a CT angiography, DSA, and a color Doppler sonography. The examination involved the assessment of the difference between bone fractures due to length, placement, and frequency.
Results
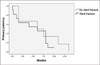
Fractures occurred in 13 of 43 stents (30.2%). A total of 10 (71.4%) occurred in the upper third, compared to 4 (28.6%) in the lower third of the superficial femoral artery. In addition, 10 stents (71.4%) had a single strut fracture, whereas 4 (28.6%) had multiple strut fractures. A stent fracture occurred more frequently when the stents and lesions were longer (p=0.021, 0.012) and the stents were inserted near the joint. However, there was no significant relationship between stent numbers and the fractures (p=0.126). When the stents were inserted along the popliteal artery, a stent fracture occurred more frequently in the lower third of the artery. The stent fractures did not significantly influence the patency rate of the stented artery (p=0.44)
Conclusion
Protégé GPS stents in the superficial femoral artery revealed a considerable number of fractures and the fracture frequency showed a significant relationship with the length of stents and lesions. The closer stent insertion was to the joints, the more frequently fractures occurred. There were no evident significant relationships between the presence of stent fractures and the patency of the stented arteries.
Figures and Tables
Fig. 2
64-year-old man with right leg claudication.
A. Type I single fracture (arrow) occur at overlapping zone in the proximal superficial femoral artery 5 months after impantation.
B. Note the reocclusion of the superficial femoral artery.

Fig. 3
A, B. 72-year-old man with type I and II stent fractures (arrows) with total occlusion of SFA at 16 months after placement of four stents in the SFA and the popliteal artery.
C, D. After balloon angioplasty (arrows) following thrombolysis with infusion of UK 240,000 U, SFA is recanalized with residual stenosis.

References
1. Chung SK, Kim JK, Yoon W, Kim J, Park JG, Kang HG, et al. Metallic stent implantation in patients with iliac artery occlusion: long term patency rate and factors related recurrence. J Korean Radiol Soc. 2003; 49:173–179.
2. Lugmayr HF, Holzer H, Kastner M, Riedelsberger H, Auterith A. Treatment of complex arteriosclerotic lesions with nitinol stents in the superficial femoral and popliteal arteries: a midterm follow-up. Radiology. 2002; 222:37–43.
3. Jahnke T, Voshage G, Muller-Hulsbeck S, Grimm J, Heller M, Brossmann J. Endovascular placement of self-expanding nitinol coil stents for the treatment of femoropopliteal obstructive disease. J Vasc Interv Radiol. 2002; 13:257–266.
4. Vogel TR, Shindelman LE, Nackman GB, Graham AM. Efficacious use of nitinol stents in the femoral and popliteal arteries. J Vasc Surg. 2003; 38:1178–1184.
5. Ruef J, Hofmann M, Haase J. Endovascular interventions in iliac and infrainguinal occlusive artery disease. J Interv Cardiol. 2004; 17:427–435.
6. Dorrucci V. Treatment of superficial femoral artery occlusive disease. J Cardiovasc Surg. 2004; 45:193–201.
7. Allie DE, Hebert CJ, Walker CM. Nitinol stent fracture in the SFA. Endovasc Today. 2004; (7):22–34.
8. Schlager O, Dick P, Sabeti S, Amighi J, Mlekusch W, Minar E, et al. Long-segment SFA stenting-the dark sides: in-stent restenosis, clinical deterioration, and stent fractures. J Endovasc Ther. 2005; 12:676–684.
9. Duda SH, Pusich B, Richter G, Landwehr P, Oliva VL, Tielbeek A, et al. Sirolimus-eluting stents for the treatment of obstructive superficial femoral artery disease: six-month results. Circulation. 2002; 106:1505–1509.
10. Kim SK, Yang HS, Han JH, Chang NK, Yim NY, Yoon W, et al. Endovascular stent placement for the treatment of superficial femoral artery stenoses and occlusions. J Korean Radiol Soc. 2008; 58:365–373.
11. Scheinert D, Scheinert S, Sax J, Piorkowski C, Braunlich S, Ulrich M, et al. Prevalence and clinical impact of stent fractures after femoropopliteal stenting. J Am Coll Cardiol. 2005; 45:312–315.
12. Ansel GM. Are stent fractures significant? Endovasc Today. 2006; (11):45–52.
13. Ansel GM. Clinical significance of stent fractures. Endovasc Today. 2006; (5):37–40.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download