Abstract
A sinus of Valsalva aneurysm is relatively rare and usually involves a single sinus. We describe here the multidetector computed tomography features of a case of an unruptured sinus of Valsalva aneurysms that affected the left and noncoronary sinuses in a 51-year-old woman.
A sinus of Valsalva aneurysm (SVA) is a relatively rare cardiac anomaly (1). SVA most commonly originates in the right coronary sinus of Valsalva (75-90%), the noncoronary sinus (10-25%), and rarely, in the left sinus (12). Unruptured SVA usually remains asymptomatic, but it can sometimes cause cardiac arrhythmia, myocardial ischemia, or systemic embolic events (123).
Multidetector computed tomography (MDCT) is a useful modality for examining the anatomy of the heart, but there have been few radiologic reports of sinus of Valsalva aneurysms diagnosed by MDCT. We report here a case of an unruptured left- and non-coronary sinus of Valsalva aneurysms detected by MDCT.
A 51-year-old woman presented with chest discomfort for four days and was taking medication to control her high blood pressure. She denied any history of previous surgery or other cardiac diseases.
An electrocardiography (ECG) performed on admission revealed atrial fibrillation. Her blood biochemistry findings were unremarkable. The chest radiograph showed cardiomegaly and right pleural effusion. A transthoracic echocardiography (TTE) showed the dilatation of the non-coronary sinus and left coronary sinus (Fig. 1), and the left atrium (LA) was compressed by the dilated left coronary sinus. TTE also revealed a moderate to severe degree of aortic regurgitation, a mild to moderate degree of tricuspid regurgitation and a mild degree of mitral regurgitation.
Chest CT examinations were performed with a 64 channel MDCT (Aquilion, Toshiba, Tokyo, Japan). The chest CT scans were obtained from the level of the thoracic inlet to the level of the diaphragm. The images were obtained with a 2 mm slice thickness in the craniocaudal direction for the axial scan, and the coronal and sagittal images were reconstructed automatically on the console. The contrast enhanced images were routinely obtained 40 seconds after the initiating the injection of contrast medium (a total of 130 mL) at a rate of 3-4 mL/s. In addition to traditional images, multiplanar reconstructions (MPR) and 3-dimensional volume-rendering images were made by an image processing workstation (Rapidia; Infinitt, Seoul, Korea) to clearly depict the coronary sinuses. On the MPR images (Fig. 2), a 4.7 × 4.3 cm sized left coronary sinus of Valsalva aneurysm (LC-SVA) without thrombosis and a 3.0 × 3.4 cm sized non-coronary sinus of Valsalva aneurysm (NC-SVA) were observed. The left main coronary artery (LM) was compressed by the LC-SVA (Fig. 3) and about 50% stenosis was suggested.
A cardiopulmonary bypass with moderate systemic hypothermia and cold blood cardioplegia was performed. The operative findings confirmed the huge aneurysms of the left coronary sinus and the non-coronary sinus of Valsalva. The leaflets of the aortic valve and ascending aorta were morphologically normal. An aortic valve sparing procedure with a 24 mm Vaxcutek graft was attempted, but failed. As a result, a Bentall operation was performed.
The most common cause of SVA is due to a congenital problem. SVA accounts for 0.1-3.5% of congenital heart disease and 0.14% of all open heart surgical procedures (12). The incidence of SVA appears to be higher in countries of the Far East and the male-female ratio is 4:1 (24). The aneurysm is thought to arise from the incomplete fusion of the distal bulbar septum that divides the aorta and pulmonary artery and attaches to the annulus fibrosus of the aortic valve. As a result, the right coronary or noncoronary sinus of Valsalva is usually affected. Because the left sinus of Valsalva does not arise from the bulbar septum, a left sinus of Valsalva aneurysm is rare and it is commonly acquired rather than being congenital (2). Aneurysms affecting both sinuses of Valsalva are extremely rare. We found only three such cases in the English medical literature (567).
SVAs usually remain asymptomatic unless rupture occurs. The incidence of unruptured SVAs has been reported to be 20%, based on previous reports of necropsy and cardiac surgical findings (1). Unruptured SVAs sometimes cause symptoms by mechanical obstruction. Expanding SVAs can obstruct the ventricular outflow tract and compress the coronary arteries or conducting system, and this can induce an acute ischemic attack, complete heart block, or arrhythmia. Furthermore, systemic embolic events may come about from thrombus formation within a SVA (1). Because of its location, distortion or deformation of the pulmonary or aortic valve leaflets can occur and this can cause aortic regurgitation or pulmonary insufficiency. Congenital SVAs are often associated with a ventricular septal defect (23).
Clinically, the diagnosis of unruptured sinus of Valsalva aneurysms may be difficult because most cases are asymptomatic (8). TTE with Doppler ultrasonography is highly useful for diagnosing sinus of Valsalva aneurysms. TTE shows the wall of the SVAs or a thrombus within the SVAs, as well as show valve movement or cardiac wall motion for evaluating the cardiac function. Yet obesity and accompanying pulmonary diseases can limit the use of TTE. Transesophageal echocardiography offers the potential for a more accurate characterization of an aneurysm, but this procedure is moderately invasive (24).
In the past, CT could not show the shape of the sinus of Valsalva or the cardiac valves because of rapid cardiac movement (29). Because of the great advances in CT technology, MDCT has recently provided images of the cross-sectional anatomy of the heart with excellent spatial and temporal resolution (4). MDCT is useful for delineating a sinus of Valsalva aneurysm and its rupture, especially in patients whose echocardiography examination is suboptimal (2). MDCT can accurately assess the aneurysm size, the sinus of origin, and aortic valve involvement (9).
In our case, MDCT accurately showed the unruptured left and noncoronary sinus of Valsalva aneurysms and the patient was successfully treated by surgical correction. MDCT can provide superior anatomic orientation between the sinus of Valsalva aneurysm and the surrounding structures (8). This case demonstrates the usefulness of MDCT for the diagnosis of unruptured aneurysms of both the left coronary and non-coronary sinuses of Valsalva.
Figures and Tables
Fig. 1
A transthoracic echocardiography shows the dilatation of the left coronary (LC) and non-coronary (NC) sinuses. The left atrium (LA) is compressed by the dilated left coronary sinus.
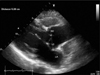
Fig. 2
64 slice-MDCT scans of a 51-year-old woman presenting with chest discomfort for four days.
A, B. Two axial images show the unruptured left coronary sinus of Valsalva aneurysm (A, arrow) and the noncoronary sinus of Valsalva aneurysm (B, arrow head).
C. The MPR image shows the dilation of the left coronary (LC) and noncoronary (NC) sinus of Valsalva and the normal right coronary sinus (RC).

References
1. Kim KH, Yang TH, Han YC, Cho HJ, Um SJ, Seol SH, et al. Huge aneurysm of the sinus of valsalva compressing the left atrium. J Cardiovasc Ultrasound. 2008; 16:140–142.
2. White CS, Plotnick GD. Case 33: sinus of valsalva aneurysm. Radiology. 2001; 219:82–85.
3. Thankachen R, Gnanamuthu R, Doshi H, Shukla V, Korula RJ. Unruptured aneurysm of the sinus of valsalva presenting with right ventricular outflow obstruction. Tex Heart Inst J. 2003; 30:152–154.
4. Kantarci M, Doganay S, Gundogdu F, Unlu Y. A case with noncoronary sinus of valsalva aneurysm: multidetector computed tomography findings. Heart Surg Forum. 2008; 11:E372–E374.
5. Tami LF, Turi ZG, Arbulu A. Sinus of valsalva aneurysms involving both coronary ostia. Cathet Cardiovasc Diagn. 1993; 29:304–308.
6. Zannis K, Tzvetkov B, Deux JF, Kirsch EW. Unruptured congenital aneurisms of the right and left sinuses of valsalva. Eur Heart J. 2007; 28:1565.
7. Vijayalakshmi IB, Devananda NS, Chitra N. A patient with aneurysms of both aortic coronary sinuses of valsalva obstructing both ventricular outflow tracts. Cardiol Young. 2009; 19:537–539.
8. Ho Hwang S, Kim TH, Kim SJ, Kwon HM, Yu KJ. Multidetectorrow computed tomography of a valsalva sinus aneurysm in a patient with behcet disease. J Thorac Imaging. 2006; 21:300–302.
9. Matteucci ML, Rescigno G, Capestro F, Torracca L. Syncope triggered by a giant unruptured sinus of valsalva aneurysm. Interact Cardiovasc Thorac Surg. 2009; 9:1047–1048.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download