Abstract
Lymphoepithelial carcinoma is a rare category of malignant neoplasm that consists of undifferentiated malignant epithelial cells admixed with lymphocytes. Lymphoepithelial carcinoma predominantly occurs in the upper aero-digestive tract and only few cases of metastasis in the posterior cervical space have currently been reported. We report here on a case of lymphoepithelial carcinoma in the posterior cervical space.
Lymphoepithelial carcinoma is an unusual squamous cell neoplasm that is characterized by undifferentiated malignant epithelial cells together with an infiltrate of mature lymphocytes. Lymphoepithelial carcinoma most frequently occurs in the nasopharynx and it has occasionally been documented in diverse sites outside the nasopharynx such as the salivary glands, larynx, thymus, etc (123).
Yet primary lymphoepithelial carcinoma has never been reported in the posterior cervical space in the medical literature, whereas several cases of metastasis of lymphoepithelial carcinoma have been reported (4). We report here on an unusual case of lymphoepithelial carcinoma in the posterior cervical space and we present the MR findings of this tumor and the correlative histopathologic features.
A 38-year-old woman had a 5-month history of a palpable mass in the left neck. She had been healthy prior to this finding and she had no history of disease. The physical examination performed by a physician revealed a painless soft mass in the left neck.
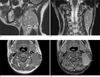
MRI examination was performed on a 1.5T MR unit (Signa Excite, GE Healthcare, Milwaukee, Wisconsin, U.S.A.). The MR image of the neck revealed a 4.3 × 2.6 × 4.7 cm, oval, single mass with a somewhat lobulated margin in the left posterior cervical space. The mass was characterized as showing intermediate signal intensity (SI) relative to the surrounding muscle on the spin-echo T1-weighted MR image (T1WI) and slightly higher SI than the surrounding muscle on the fast spin-echo T2-weighted MR image (T2WI) (Figs. 1A-C). Multiple microtubular cystic clefts were demonstrated in the mass on T2WI (Fig. 1B). The gadolinium-enhanced axial fat suppressed T1-weighted spin-echo MR image showed slightly heterogeneous enhancement of the mass without central necrosis or an enhancing capsule (Fig. 1D). There was no significant peri-tumoral soft tissue infiltration. Several small lymph nodes were found around the mass, but they were too small to characterize. The scanned pharyngeal mucosal space and salivary glands did not show any significant abnormality.
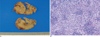
Surgical excision revealed a well-defined grayish tan soft tissue mass with a lobulated contour in the posterior cervical space. Pathologic examination demonstrated islands of undifferentiated carcinoma cells mixed with lymphocytes and plasma cells, and this was all consistent with lymphoepithelial carcinoma (Figs. 2A, B)
We suspected this tumor to be metastasis of lymphoepithelial carcinoma because primary lymphoepithelial carcinoma in the posterior cervical space has never been reported in the current medical literature. An endoscopic survey of the upper aero-digestive tract and whole body PET-CT were performed for evaluating the primary origin of this tumor, but these modalities did not reveal any evidence of a primary tumor.
The patient underwent post-operative radiation therapy on the operation site and adjuvant chemotherapy for possible hidden primary tumor three times, respectively. The patient has been under continuous follow-up at our hospital, and any primary tumor or other metastatic lesions have not developed for approximately 6 months.
Lymphoepithelial carcinoma can be divided into two large groups and these are nasopharyngeal and non-nasopharyngeal lymphoepithelial carcinoma. According to the World Health Organization classification, nasopharyngeal lymphoepithelial carcinoma is the undifferentiated subtype of non-keratinizing nasopharyngeal carcinoma. Non-nasopharyngeal lymphoepithelial carcinoma has been described at diverse sites such as the sinonasal tract, nasolacrimal duct, oral cavity, oropharynx, salivary glands, thymus, hypopharynx, esophagus, stomach, larynx, trachea, lung, uterine cervix, urinary bladder and skin (23).
Lymphoepithelial carcinoma of a squamous cell origin is histopathologically difficult to develop in the posterior cervical space because the main contents of this space are lymph nodes, nerves and fat, and there are no soft tissues associated with squamous cells in the posterior cervical space. As a result, lymphoepithelial carcinoma encountered in the posterior cervical space can be generally considered as a metastatic carcinoma (56).
The primary foci of cervical metastatic carcinoma are mostly in the head and neck regions, and the majority of the primary cancers are found by subsequent imaging studies. But they cannot be detected when they are limited to the submucosa of pharyngeal mucosal space, and cervical nodal metastases can only be detected when they reach a certain visible size. The incidence of cervical metastatic carcinoma of an unknown origin is estimated to be between 3 and 11% of the cases of head and neck carcinoma. Thus, endoscopy of the upper aero-digestive tract should be performed in order to detect the primary tumor in such patients. If possible, blind systemic pharyngeal biopsies should also be performed, and CT/MRI or PET-CT should follow (4).
The MRI features of metastasis of lymphoepithelial carcinoma have not been established because of the rarity of reported cases. Metastasis of typical squamous cell carcinoma manifests as unilateral multiple masses along the nodal chain and this rarely presents as a single mass. This tumor generally shows an intermediate SI on T1WI and a slightly higher signal than the muscle on T2WI. The gadolinium-enhanced MR image frequently shows central necrosis with peripheral irregular enhancement in the tumor, and especially when the size of the mass is greater than 3 cm. But metastatic carcinoma can at times shows variable imaging features according to the type of primary cancer and it can present as a homogeneous enhancing mass without a necrotic portion (7).
In our case, central necrosis was not shown in the mass despite the large size of the mass, and microtubular cystic clefts were also seen. Microtubular cystic clefts are dilated lymphovascular channels that are seen on the gross photograph of a specimen. We considered that these findings can be a kind of diagnostic clue that favors the diagnosis of metastasis of lymphoepithelial carcinoma rather than metastasis of another primary tumor or a solitary tumor such as schwannoma.
The differential diagnosis in this case also can include lymphoma and neurogenic tumors. Lymphoma manifests as a large (> 2 cm) solid mass and it typically presents with lymphadenopathy involving multiple other nodal chains. Lymphoma shows homogeneous intermediate SI on T1WI and high SI on T2WI. Unlike metastasis of squamous cell carcinoma, it shows relatively uniform enhancement and it rarely shows central necrosis or heterogeneous enhancement, except during the posttreatment state (8). Among the neurogenic tumors, schwannoma and solitary neurofibroma occasionally occur on the brachial plexus or cranial nerve 11 in the posterior cervical space. These tumors appear as a welldefined oval or fusiform mass, and they show variable SI from low to high on T1WI and hyperintensity compared to muscle on T2WI. Cystic changes frequently can be seen in the tumor, but necrosis is very rare. Paraganglioma commonly occurs in the carotid body and it very rarely occurs in the posterior cervical space. This tumor can sometimes show a "salt and pepper" appearance on TIWI if it is bigger than 1.5 cm and the tumor shows intense enhancement with internal flow voids on the post contrast image (9).
In summary, we experienced an unusual case of pathologic confirmed lymphoepithelial carcinoma in the posterior cervical space. Although the primary origin of this tumor was not found on following studies, we think that these MR findings such as homogeneous enhancement without central necrosis and intra-tumoral microtubular cystic clefts can be the points for differentiating metastasis of lymphoepithelial carcinoma from metastasis of other primary tumors or solitary tumors.
Figures and Tables
Fig. 1
The MR imaging reveals a well-defined mass with a lobulated contour in the left posterior cervical space.
A, B. On the coronal (A) and sagittal (B) T2-weighted fast spin-echo MR images, the mass shows slightly higher signal intensity than the surrounding muscle and intra-tumoral microtubular cystic clefts (arrows).
C. The axial T1-weighted spin-echo MR image shows an isointense mass (arrows) relative to the surrounding muscle.
D. The gadolinium-enhanced axial fat suppressed T1-weighted spin-echo MR image shows the slightly heterogeneous enhancement of the mass (arrows) without central necrosis or an enhancing capsule.
References
1. Mills SE, Fechner RE. The nose, paranasal sinuses and nasopharynx. Diagnostic surgical pathology. 3nd ed. New York: Lippincott Williams & Wilkins;1999. p. 885–924.
2. Chan JKC, Bray F, McCarron P, Foo W, Lee AWM, Yip T, et al. Tumours of the nasopharynx: Nasopharyngeal carcinoma. In : Bames L, Eveson JW, Reichart P, Sidransky D, editors. Pathology and genetics of head and neck tumours: WHO classification of tumours. Lyon: IARC Press;2005. p. 83–97.
3. Wassef M, Le Charpentier Y, Monteil JP, Le Tien K, Galian A. Undifferentiated carcinoma with lymphoid stroma (undifferentiated carcinoma nasopharyngeal type): optical, electron microscopical and immunofluorescence study. Bull Cancer. 1982; 69:11–21.
4. Haas I, Hoffmann TK, Engers R, Ganzer U. Diagnostic strategies in cervical carcinoma of an unknown primary (CUP). Eur Arch Otorhinolaryngol. 2002; 259:325–333.
5. Parker GD, Harnsberger HR. Radiologic evaluation of the normal and diseased posterior cervical space. AJR Am J Roentgenol. 1991; 157:161–165.
6. Som PM, Curtin HD. Head and Neck Imaging. 4th ed. St Louis, Mo: Mosby-Elsevier Science;2003. p. 1824–1825.
7. Sakai O, Curtin HD, Romo LV, Som PM. Lymph node pathology. Benign proliferative, lymphoma, and metastatic disease. Radiol Clin North Am. 2000; 38:979–999.
8. Weber AL, Montandon C, Robson CD. Neurogenic tumors of the neck. Radiol Clin North Am. 2000; 38:1077–1090.
9. Kaji AV, Mohuchy T, Swartz JD. Imaging of cervical lymphadenopathy. Semin Ultrasound CT MR. 1997; 18:220–249.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download