Abstract
Intrathoracic mesothelial cysts are congenital developmental cysts usually located in the anterior cardiophrenic angle region (so called, pericardial cysts). We report two rare cases of an intrathoracic paraspinal mesothelial cyst which was purely cystic and had no perceptible cyst wall on CT or MRI with histopathologic findings.
The differential diagnosis of paraspinal masses usually include neurogenic tumors and neoplastic lymphadenopathy. Cystic lesions including neurenteric cysts, lateral thoracic meningoceles, and mesothelial cysts rarely develop in the paraspinal region. Intrathoracic mesothelial cysts are fluid-filled and lined with mesothelial cells and are typically located in the anterior cardiophrenic angle (so called, pericardial cysts). However, they can occur in unusual locations such as the paratracheal region, anterior mediastinum, or paravertebral region (1234). We report two rare cases of intrathoracic paraspinal mesothelial cysts that were incidentally detected on CT and MR images.
A 51-year-old woman presented with right shoulder pain radiating to the right upper extremities for 2 months. She had a history of a cervical spinal operation for treatment of posterior longitudinal ligament ossification 3 years prior.
Magnetic resonance imaging of the cervical spine, performed under the impression of cervical radiculopathy, incidentally revealed a well-circumscribed, 1.2 × 0.8 × 1.4 cm sized, spindle-shaped mass abutting the right anterolateral side of the T3 vertebra (Figs. 1A, B). The mass was seen as homogeneous with low signal intensity on T1-weighted images and homogeneous with high signal intensity on T2-weighted images. These findings corresponded with a cystic mass, but did not show a discernible cyst wall or solid component. On non-contrast chest CT scans, the attenuation of the mass was homogeneously low (Fig. 1C). On both MR and CT studies, the mass had no continuity with the pericardium, spinal canal, esophagus, or airway, and there was no associated abnormality of the adjacent vertebral bodies (Figs. 1A-C). Moreover, there were no abnormal findings for a physical examination or laboratory tests attributable to the mass.
An exploratory right lateral thoracotomy disclosed a translucent, cystic mass beneath the parietal pleura in the right anterolateral side of the T3 vertebra that had no anatomic continuity with the pericardium, esophagus, or airway. When the parietal pleura overlying the tumor was incised, the mass easily separated from the T3 nerve roots. The tumor was a unilocular, thin-walled cyst with internal clear fluid and microscopically determined to be lined with a layer of flat or cuboidal mesothelial cells which were positive for keratin and negative for the lymphocyte marker (Fig. 1D). No malignant foci were found and these findings were consistent with a mesothelial cyst.
A 44-year-old woman visited the emergency room due to a traffic accident. She complained of nuchal pain and a tingling sensation in two fingers which she had felt four years prior. Evaluation of the patient revealed a fracture of the sternum and ribs, hepatic laceration, and a cardiac contusion. Incidentally, a non-enhanced and enhanced CT of the chest demonstrated a 2.3 × 1.1 × 2.0 cm sized, non-enhancing, spindle-shaped, low-attenuation mass abutting the right lateral side of the T7 vertebra (Figs. 2A, B). The mass had no peripheral enhancement corresponding to a cyst wall, and had no connection with the pericardium, airway, esophagus, or spinal canal. Also, there was no associated abnormality of adjacent vertebral bodies.
As a result, a thoracoscopic resection was performed. Operative and histological findings were the same as those of Case 1 described above, except for the location and size of the mass. The diagnosis was a mesothelial cyst.
Mesothelial cysts are benign developmental anomalies representing 5-10% of mediastinal tumors (2). The cyst is also known as mesothelial inclusion cyst, benign cystic mesothelioma, or coelomic cyst (25). Intrathoracic mesothelial cysts are classically located in the anterior cardiophrenic angle (pericardial cysts), and on rare occasions can be located elsewhere such as the paraspinal region, the anterior mediastinum, or the paratracheal region. In our two cases, mesothelial cysts were located in the paraspinal region, and three such cases have been reported in the previous literature (23). The different locations of these cysts are explained by embryological factors. Fusion of mesenchymal coelomic lacunae gives rise to the pleural and pericardial cavity on one side, the peritoneal cavity on the other, and are also divided by the antero-posterior development of the septum transversum. Incomplete fusion or secondary migration of an isolated lacunae at the level of parietal pleura, mediastinal pleura, or septum transversum can result in mesothelial cyst formation in the chest wall, mediastinum, or diaphragm (2).
Sometimes, mesothelial cysts may cause symptoms and signs due to the compression of adjacent structures or due to complications such as infection, rupture, or hemorrhage (267). Perrini et al. (3) reported a case of dorsal radiculopathy caused by a paraspinal mesothelial cyst compressing adjacent nerve roots. Although there were similar symptoms in our cases, they do not appear to be caused by mesothelial cysts because they did not match the dermatomes of adjacent spinal nerve roots.
Typical CT findings of a mesothelial cyst consist of a well-circumscribed lesion with a near-water attenuation value (Figs. 1, 2). Sometimes, a mesothelial cyst can be misinterpreted when the density is greater than 30 HU (28). In these cases, the absence of enhancement after contrast injection is helpful for a radiological diagnosis of mesothelial cyst. MRI revealed signals similar to those of water on all imaging sequences and, especially for paraspinal lesions, MRI is essential to rule out a cyst of meningeal or neurogenic origin with a connection to the spinal canal (2).
Neurenteric cysts or lateral thoracic meningoceles may show similar cystic lesions in the paraspinal area, but they are usually associated with vertebral body anomalies or widening of the adjacent neural foramina, respectively, which is contrary to mesothelial cysts without such abnormalities. Esophageal duplication cysts or bronchogenic cysts which are usually located near the esophagus or airway, respectively, may be indistinguishable from mesothelial cysts arising from the same area, but they would be distinguished from mesothelial cysts in the paraspinal area by their main tumor locations.
In summary, a mesothelial cyst is a unilocular cystic tumor without a perceptible cyst wall on CT or MRI. Differential diagnosis for such a cystic lesion in the paraspinal area should include a mesothelial cyst, especially if there is no associated spinal abnormality.
Figures and Tables
Fig. 1
T1- (A) and T2-weighted (B) MRI at the level of the T3 vertebra show a small well-circumscribed cyst (arrows) with signal characteristics similar to water in the right paraspinal area. Note that there is no perceptible cyst wall, vertebral abnormalities, or continuity with the pericardium, esophagus, or airway.
C. Noncontrast thin-section CT at the same level shows a water attenuation mass abutting the right anterolateral side of the vertebra.
D. Photomicroscopic image of the resected specimen shows a layer of flat or cuboidal cells lining the cyst wall (Hematoxylin and Eosin stain; original magnification, ×400). The lining cells were positive for keratin and negative for the lymphocyte marker (not shown), which was consistent with the mesothelial cyst diagnosis.

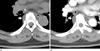
Fig. 2
Noncontrast (A) and contrast-enhanced (B) CT at the level of the T7 vertebra shows a well-demarcated, non-enhancing, water attenuation mass (arrows) just lateral to the vertebral body. The mass had no connection with the pericardium (closed arrowhead), esophagus (open arrowhead), or airway, excluding the diagnosis of pericardial cyst, esophageal duplication cyst, or bronchogenic cyst.
References
1. Jamplis RW, Lillington GA, Mills W Jr. Pleural cysts simulating mediastinal tumors. JAMA. 1963; 185:727–728.
2. Mouroux J, Venissac N, Leo F, Guillot F, Padovani B, Hofman P. Usual and unusual locations of intrathoracic mesothelial cysts. Is endoscopic resection always possible? Eur J Cardiothorac Surg. 2003; 24:684–688.
3. Perrini P, Benedetto N, Buccoliero AM, Di Lorenzo N. Thoracic radiculopathy from a paravertebral mesothelial cyst. Acta Neurochir (Wien). 2006; 148:989–991.
4. Urschel JD, Horan TA. Mediastinoscopic treatment of mediastinal cysts. Chest. 1998; 114:1794.
5. Urbanczyk K, Skotniczny K, Kucinski J, Friediger J. Mesothelial inclusion cysts (so-called benign cystic mesothelioma)--a clinicopathological analysis of six cases. Pol J Pathol. 2005; 56:81–87.
6. Borges AC, Gellert K, Dietel M, Baumann G, Witt C. Acute right-sided heart failure due to hemorrhage into a pericardial cyst. Ann Thorac Surg. 1997; 63:845–847.
7. King JF, Crosby I, Pugh D, Reed W. Rupture of pericardial cyst. Chest. 1971; 60:611–612.
8. Brunner DR, Whitley NO. A pericardial cyst with high CT numbers. AJR Am J Roentgenol. 1984; 142:279–280.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download