Abstract
Ectopic thyroid tissue in the lateral neck is an uncommon congenital anomaly, and the occurrence of primary follicular carcinoma in this ectopic thyroid tissue is very rare. We report here on such a case of follicular carcinoma arising in ectopic thyroid tissue of the left lateral neck without any evidence of primary carcinoma in the original thyroid gland.
Embryologically, the thyroid gland is derived from a large median endodermal anlage and two lateral anlages (1). Commonly, the median anlage fails to descend, resulting in a lingual thyroid gland. In rare cases, failure of the lateral anlage to fuse with the median anlage produces a lateral ectopic thyroid gland (2).
There are a number of case reports of papillary thyroid carcinomas in ectopic thyroid tissue, but there are only a few cases of primary follicular carcinoma in an ectopic thyroid gland (34). We report here on the ultrasonography (US), computed tomography (CT) and magnetic resonance image (MRI) findings of a primary follicular carcinoma arising from ectopic thyroid tissue in the lateral neck. To the best of our knowledge, this is the first such case report with the findings of these three imaging modalities.
A 39-year-old man presented with a left lateral neck mass that he had had for two years. Physical examination revealed a 3 cm non-tender mass in the left lateral neck. There was no underlying disease and the laboratory test results were within the normal limits.
The CT scan demonstrated a 4.2×3.0×5.4 cm sized, well-defined, spindle-shaped mass located postero-inferior to the left submandibular gland (Fig. 1). The mass showed slightly hypodense attenuation on the precontrast CT scan, and strong and inhomogeneous enhancement on the postcontrast scan. The left carotid artery and internal jugular vein were displaced laterally by the mass. No definite lymph node enlargement was noted. On the consecutive MRI (Fig. 2), the mass showed intermediate signal intensity on the T1-weighted image and high signal intensity on the T2-weighted image, with strong enhancement after gadolinium injection. Because of the location and morphology of the mass, it was suspected of being a neurogenic tumor or a lymph node-related disorder. Ultrasound (US) revealed the inhomogeneous iso- and hypo-echogenecity of the mass and no focal lesions in the thyroid gland (Fig. 3). The mass was targeted for US-guided fine needle aspiration cytology and it was strongly suspected to be a follicular neoplasia or a follicular variant of papillary carcinoma.
A well-defined encapsulated mass was excised from the left level II neck space under general anesthesia. Histopathologic examination revealed a 5.5×4×3 cm-sized minimally invasive follicular carcinoma with focal capsular invasion (Fig. 4). There was no evidence of lymphoid cells or lymphovascular invasion. The patient had an uneventful postoperative recovery and he was discharged on the third day after surgery.
The thyroid develops embryologically from a median anlage and a pair of lateral anlages. The median anlage arises from the pharyngeal floor, whereas the lateral anlages originate from the fourth and fifth branchial pouches (ultimobranchial bodies). In 1955, Springer (5) proposed that the lateral thyroid arises from evaginations and gemmations dilated from the lateral lobes of the thyroid primordia. These lateral "sprouts" of the thyroid may become detached and be left behind, and they constitute the thyroid tissue in the region of the upper neck and in the neighborhood of the angle of the jaw.
Primary thyroid carcinomas arising from ectopic thyroid tissue are uncommon; they have been reported to arise from thyroid tissue in thyroglossal duct cysts, lateral aberrant thyroid tissue, lingual thyroid and mediastinal and struma ovarii. Most tumors of ectopic thyroid tissue have been reported to be papillary carcinomas, mixed follicular and papillary carcinomas or Hurthle cell tumors (3). Follicular carcinomas in ectopic thyroid tissue have also been occasionally reported (6), but primary follicular carcinomas arising from ectopic thyroid tissue of the lateral neck have very rarely been reported (34).
The ultrasound features of follicular thyroid carcinomas are reported to include well-defined and/or haloed, hypoechoic, predominantly solid and homogeneous masses containing intranodular flow with multiple, chaotically arranged vascular poles and with or without significant perinodular vessels (7). In our patient, the mass showed well-defined inhomogeneous iso- and hypo-echogenicity with intranodal vascularity. The CT and MRI findings of follicular carcinomas are relatively nonspecific and they are generally less helpful for the initial evaluation and differential diagnosis (8). On the CT image of our patient, the mass presented as a well-circumscribed, slightly hypodense or isodense mass with strong enhancement. On MRI, the mass showed isointensity on the T1-weighted images and hyperintensity on the T2-weighted images. It also showed prominent enhancement on the gadolinium-enhanced T1-weighted images.
As our patient did not undergo total thyroidectomy, microscopic evaluation of the original thyroid gland was not possible. However, the follicular carcinoma was regarded to have originated from the ectopic thyroid tissue in the lateral neck rather than being a metastatic lymphadenopathy because the original thyroid gland appeared normal on all the US, CT and MR imaging modalities over the two year history of the palpable neck mass. An excised specimen of the lateral neck mass revealed no evidence of lymphoid cells, and the patient has been free of any signs or symptoms of a thyroidal lesion for 15 months since the surgery.
This mass lesion in the lateral neck could have been misdiagnosed as a neurogenic tumor or lymph node-related lesion, and particularly lymph node metastasis from an occult thyroid cancer; hence, careful evaluation of the native original thyroid is very important. We report here on a case of follicular thyroid carcinoma arising from ectopic thyroid tissue in the lateral neck without evidence of abnormality in the native original thyroid gland, with US, CT and MRI findings.
Figures and Tables
Fig. 1
CT findings on the lateral neck mass in a 39-year-old man.
A. The axial pre-enhanced CT image shows a 4.2×3.0×5.4 cm-sized welldefined, isodense mass (arrow) in the left posterior submandibular space.
B. The axial postcontrast CT image shows the strong and inhomogenous enhancement of the mass (arrow). The left submandibular gland is displaced anteriorly by the mass.
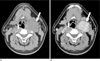
Fig. 2
MRI findings on the lateral neck mass.
A, B. The mass (arrow) shows well-defined, homogenous isointensity on the T1-weighted MR image (A) and mild hyperintensity on the T2-weighted MR image (B).
C, D. The axial and coronal fat-saturated gadolinium-enhanced T1-weighted MR images show inhomogeneous enhancement of the mass (arrow). The external and internal carotid arteries are displaced laterally due to the mass (arrowhead in D).

Fig. 3
US findings of the lateral neck mass.
A. The gray-scale US shows a circumscribed inhomogeneous mass (arrow) in the left posterior submandibular space.
B. The color Doppler scan shows some internal vascularity of the mass (arrow).
C. No abnormal lesion is found in the native original thyroid on US.

Fig. 4
Histopathologic findings on the excised mass.
A. The photograph of the gross specimen (arrow) shows it is ovoid in shape with a smooth external surface and solid cut surface, and it measures 5.0×3.5 cm.
B. Photomicrograph of the specimen shows that the tumor is composed of thyroid tissue (arrow) with small, abortive follicles. The tumor has invaded the vessels (arrowhead) in the outermost portion of the capsule.

References
1. Mansberger AR Jr, Wei JP. Surgical embryology and anatomy of the thyroid and parathyroid glands. Surg Clin North Am. 1993; 73:727–746.
2. Basaria S, Westra WH, Cooper DS. Ectopic lingual thyroid masquerading as thyroid cancer metastases. J Clin Endocrinol Metab. 2001; 86:392–395.
3. Subramony C, Baliga M, Lemos LB. Follicular carcinoma arising in ectopic thyroid tissue: case report with fine-needle aspiration findings. Diagn Cytopathol. 1997; 16:39–41.
4. Tucci G, Rulli F. Follicular carcinoma in ectopic thyroid gland. A case report. G Chir. 1999; 20:97–99.
5. Springer KC. Lingual thyroid: two cases in siblings diagnosed and treated with radioactive iodine. AMA Arch Otolaryngol. 1955; 61:386–393.
6. Potdar GG, Desai PB. Carcinoma of the lingual thyroid. Laryngoscope. 1971; 81:427–429.
7. Wong KT, Ahuja AT. Ultrasound of thyroid cancer. Cancer Imaging. 2005; 5:157–166.
8. Angelos P. Current approaches to the treatment of well-differentiated thyroid cancer. Oncology (Williston Park). 2002; 16:309–331.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download