Scleroderma is a chronic autoimmune disease that can be systemic or localized to the skin. Linear scleroderma is an uncommon subtype of scleroderma which produces an unilateral, localized band-like linear atrophy of the skin and its underlying structures which in rare cases, causes orbital complications are rarely seen in linear scleroderma. We introduce Orbital CT and MR findings of scleroderma with enophthalmos.
Case Report
Case 1
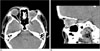
A 44-year-old woman was referred to an ophthalmologist due to a visual disturbance and progressive shrinking of the left eye that has occurred over the last 2 years. Sixteen years prior, the woman had been diagnosed with a localized scleroderma of the face and underwent skin graft surgery due to progressive skin sclerotic thickening of the left eyelid. The patient's exophthalmometry measured 20 mm in the right eye and 12 mm in the left eye. In addition she also diagnosed with a cataract and enophthalmos of the left eye and underwent surgery for the left cataract. An orbital CT was performed for further evaluation and found decrease in the amount of left orbital fat as well as a reduction of the left orbit. Those findings were diagnosed as enophthalmos caused by scleroderma (Fig. 1). A her enhancing soft tissue lesion of the left retrobulbar area showed the possibility of inflammatory tissue associated with scleroderma (Fig. 1). The patient was subsequently followed the ophthalmologic department of our institution.
Case 2
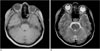
A 46-year-old woman was diagnosed with localized scleroderma at an outside hospital. Her medical history was not recorded for personal reasons. A brain MR verified at the department of neurosurgery at our institution showed a depressed left eyeball, a decreased amount of orbital fat, and a reduction in the size of the left orbit, which was indicative of enophthalmos (Fig. 2). In the left retrobulbar soft tissue, a linear low singal intensity on T1 weighted image was observed, which was probably indicative of inflammatory tissue (Fig. 2A).
Discussion
Scleroderma is a chronic autoimmune disease that can be systemic or localized to the skin. Localized forms of scleroderma are distinguished from systemic sclerosis, not only by the absence of vasospasm, structural vascular damage, and involvement of internal organs, but also by the distribution of the skin lesions (1). The 3 main varieties of localized scleroderma are morphea, linear scleroderma, and coup de saber (1). Linear scleroderma is manifested as a linear streak that crosses dermatomes and is associated with the tracking of fibrosis from the skin to deeper tissues, including muscle and fascia (2). In severe cases, scleroderma causes dramatic growth deformities of bone and supporting tissues in the affected regions (2). En coup de saber ("sword stroke") is a subtype of linear scleroderma that affects the face or scalp and is associated with atrophy of muscle, underlying bone, and in rare cases, brain tissue (2). Parry-Romberg syndrome is a condition of hemifacial atrophy involving skin and tissues below the forehead that can also cause enophthalmos, though it generally has minimal involvement with the superficial cutaneous layers (3).
Linear scleroderma is divided into two histologic stages- the early inflammatory stage and the late sclerotic stage (4). The early inflammatory stage is characterized by coarsened collagen bundles in the reticular dermis with perivascular lymphocytic infiltrates, at which point, the skin appears indurated (4). The hyalinization of collagen bundles, which replace subcutaneous fat and muscle, characterize the late sclerotic phase of scleroderma. The most important feature of this stage is the absence of tissue elasticity (4).
Enophthalmos is a relative posterior displacement of a normal-sized eye in relation to a bony orbital margin. Unilateral enophthalmos is said to be present when there is a difference of more than 2 mm on exophthalmometry between the 2 eyes(3) and has 3 main pathogenic mechanisms (3). The first mechanism is the structural alterations in the bony orbit brought out by maxillary sinus disease, bony defect, and bone disease (3). The second mechanism is orbital fat atrophy (i.e., senile change, periorbital or systemic disease, pressure effect, and radiation) and the third mechanism is the retraction owing to metastasis, restrictive myopathy, and postinflammatory change (3). The main mechanism of enophthalmos among the 3 etiologies mentioned above related to scleroderma is orbital fat atrophy (5). The thickening of the orbital muscles can be secondary effect of orbital fat atrophy and fibrosis (6). Traditionally, scleroderma shows cutaneous atrophy, which can include balding and loss of eye lashes, as has occurred in our patient (3).
Ophthalmic signs in scleroderma except for enophthalmos, may include atrophy, sclerosis, or inflammation of the eyelids, orbit or globe (4). Patients can show various ophthalmic manifestations such as the loss of eyelash, eyelid induration or tightening, periorbital edema, corneal opacities, and thickening, keratoconjunctivitis sicca, fornix shortening, ocular myopathy or palsy, iritis, iris atrophy and heterochromia, and retinal hemorrhages (4).
In conclusion, linear scleroderma is one of the rare causes of enophthalmos. Linear scleroderma often involves skin and tissue below the forehead, resulting in orbital tissue atrophy and enophthalmos.




 ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download