Abstract
Breast cancer is one of the most common malignancies in women and the main leading cause of cancer death. Breast cancer frequently metastasizes to the bones, lungs, and liver; however, gastrointestinal involvement is rare. The most frequent sites of the GI tract involved are the stomach and the small intestine, while colonic metastasis is extremely rare with the presentation being nonspecific. Early diagnosis is important for proper treatment. We present a case of metastatic breast cancer to the small and large bowel.
Breast cancer is one of the most common malignancies in women and the main cause of cancer-related deaths (1). Breast cancer usually metastasizes to the lymph nodes, lung, bone, liver or brain. However, metastases to the gastrointestinal (GI) tract are rare. The most frequent sites of the GI tract involved are the stomach and the small intestine, while a colonic metastases is extremely rare (23). Because of its rarity and its nonspecific clinical presentation, a colonic metastasis may be easily mistaken for a double primary colonic carcinoma in patients with history of breast cancer.
Nevertheless, early recognition of this metastatic disease is important because the treatment for these two diseases could vary greatly. We herein report the case of a patient with breast cancer metastases to the colon and small bowel along with a review of literature.
A 70-year-old woman had been diagnosed with locally advanced breast cancer in her left breast in 2007 (Fig. 1). After six cycles of neoadjuvant chemotherapy (cyclophosphamide, methotrexate, and 5-fluorouracil), she had underwent a left modified radical mastectomy and ipsilateral axillary lymph node dissection. A histopathological examination revealed a 3.5 cm sized invasive ductal carcinoma (IDC) of nuclear grade 3, histologic grade III, and metastatic carcinoma in 10 out of 28 lymph nodes with perinodal soft tissue extension. Immunohistochemistry for estrogen and progesterone receptors showed negative staining for both receptors. There was no evidence of distant metastases at the time of surgery. Consequently, the breast cancer was consistent with stage IIIA. After the operation, she received one cycle of radiotherapy at 3,600 cGy dose and a 10th adjuvant cycle of oral chemotherapy (Capecitabine) for 7 months.
Although, there was neither evidence of recurrence, nor metastatic lesions during the two follow-up examinations (six monthly ultrasound, mammography, and biochemical investigations) over the course of two years after surgery. However, a hemoglobin drop of 3 g/L (10.7 to 7.7) was noted in the last follow-up study. An esophagogastroduodenoscopy (EGD) and colonoscopy was recommended for the further study.
The patient underwent an EGD and colonoscopy, which revealed an ulcerofungating mass occupying 30% of circumference of the bowel within the distal transverse colon (Fig. 2). A biopsy was performed, in addition to pathological examination including special immunohistochemical stains, confirmed the diagnosis of a metastatic breast cancer to the transverse colon; pathologic findings were similar to those of the prior breast cancer specimen. Abdominal CT and FDG-PET/CT (Figs. 3A-D) for staging workup revealed an additional 3 × 2.5 cm-sized enhancing mass in the distal ileum causing the intussusception. However, following a small bowel series, there was no evidence of a small bowel mass or lead point. The patient underwent left hemicolectomy and segmental resection of the small bowel with the tentative diagnosis of two concomitant metastatic lesions in the small and large intestine.
A histological examination of the surgical specimens confirmed the diagnosis of metastatic breast cancer in the colon and small intestine (Figs. 4A, B). The postoperative course was uneventful and adjuvant chemotherapy (taxol) was performed.
Although common locations of metastases from breast cancer are the bones, lungs, liver, pleura, adrenals and the central nervous system, GI metastases of breast cancer are rare and usually associated with disseminated disease (4). The stomach is the more frequently involved GI organ, while colonic and rectal metastases are extremely rare (23). Asch et al. (5) reported GI tract metastasis secondary to breast cancer in 1968, which was the largest case series in the medical literature. The sites of involvement of the GI tract included the esophagus (25%), stomach (25%), small intestine (28%), colon (19%), and rectum (4%). There was no mention of the primary histological subtype in this series.
In our case, the histological subtype of metastatic breast cancer was IDC. However, infiltrating lobular carcinoma was found to metastasize more frequently to the GI tract, peritoneum and retroperitoneum than the IDC (6). Taal and colleagues retrospectively identified 17 patients with metastatic breast cancer to the colon or rectum over a 15-year-period. Fifteen of these patients (88%) had lobular carcinoma and only one (6%) had IDC. Therefore, lobular carcinoma represents the most common subtype of breast cancer metastasizing to the colon and rectum (37), although it is not the most common type of primary breast malignancy, accounting for less than 10% (2). The reasons for this have not been clarified.
In our case, metastatic lesions were confined to the small and large intestine without disseminated metastasis. Metastases in multiple sites of the GI tract like our case were reported in the literature only as autopsy studies (89). Our case is the first in non-autopsied case. Although the therapeutic management is still controversial, there is general agreement on the need for palliative surgery (10). Especially, when the leading point of the intussusception is suspected as malignancy like in our case, surgical resection of the involved bowel without attempted reduction is required.
Isolated GI metastases without disseminating metastasis to other organs are extremely rare and are less common than benign disease processes or second primaries of the intestinal tract in patients with a history of breast cancer. However, in patients with a history of breast cancer, especially, a histological subtype of lobular carcinoma and a newly identified GI neoplasm, the radiologist should be concerned about the possibility of metastatic breast cancer. In conclusion, a detailed pathological analysis and repetition of endoscopy are necessary for early diagnosis.
Figures and Tables
Fig. 1
A 70-year-old woman with locally advanced cancer in the left breast. US image demonstrates a 3 cm-sized irregular hypoechoic mass at 1 o'clock position.
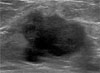
Fig. 2
Colonoscopy shows an ulcerofungating mass at the distal transverse colon with lobulation on the surface.
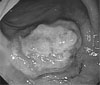
Fig. 3
A 70-year-old woman followed after undergoing a left mastectomy due to locally advanced breast cancer in her left breast.
A. Abdominal CT shows an enhancing mass (arrow) in the distal portion of transverse colon, corresponding to the finding on a colonoscopy.
B. There is another enhancing mass (arrow) in the distal ileum causing the intussusceptions (arrowhead).
C, D. Strong F-18 FDG uptakes are noted for each lesion (SUV 8.9 (C) and 10.4 (D), respectively).

Fig. 4
Histopathologic findings of initial breast cancer and colonic metastasis.
A. Histologic finding of the initial breast mass. Infiltrating ductal carcinoma showing marked nuclear atypia with prominent nucleoli (Original magnification: ×400).
B. Histologic finding of the colon. The tumor is composed of non-cohesive, pleomorphic tumor cells with prominent nucleoli. The immunohistochemical staining of CK7 (+) and CK20 (-) favors the diagnosis of metastatic carcinoma over primary gastrointestinal carcinoma.

References
1. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA: Cancer J Clin. 2008; 58:71–79.
2. Schwarz RE, Klimstra DS, Turnbull AD. Metastatic breast cancer masquerading as gastrointestinal primary. Am J Gastroenterol. 1998; 93:111–114.
3. Taal BG, den Hartog Jager FC, Steinmetz R, Peterse H. The spectrum of gastrointestinal metastases of breast carcinoma: II. The colon and rectum. Gastrointest Endosc. 1992; 38:136–141.
4. Rabau MY, Alon RJ, Werbin N, Yossipov Y. Colonic metastases from lobular carcinoma of the breast. Dis Colon Rectum. 1988; 31:401–402.
5. Asch MJ, Wiedel PD, Habif DV. Gastrointestinal metastases from crcinoma of the breast. Autopsy study and 18 cases requiring operative intervention. Arch Surg. 1968; 96:840–843.
6. Borst MJ, Ingold JA. Metastatic patterns of invasive lobular versus invasive ductal carcinoma of the breast. Surgery. 1993; 114:637–641.
7. Washington K, McDonagh D. Secondary tumors of the gastrointestinal tract: surgical pathologic findings and comparison with autopsy survey. Mod Pathol. 1995; 8:427–433.
8. Cifuentes N, Pickren JW. Metastases from carcinoma of mammary gland: an autopsy study. J Surg Oncol. 1979; 11:193–205.
9. Graham WP 3rd, Goldman L. Gastro-intestinal metastases from carcinoma of the breast. Ann Surg. 1964; 159:477–480.
10. Clavien PA, Laffer U, Torhost J, Harder F. Gastro-intestinal metastases as first clinical manifestation of the dissemination of a breast cancer. Eur J Surg Oncol. 1990; 16:121–126.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download