Abstract
The congenital absence of the submandibular gland is very uncommon, and might occur in association with other developmental abnormalities. Unilateral aplasia is reported more infrequently because it is usually asymptomatic, whereas the bilateral form often presents as xerostomia, dysphagia, and frequent dental caries because of decreased salivary flow. Submandibular gland aplasia with a concurrent thyroglossal duct cyst (TGDC) has not been reported. We report a case of unilateral submandibular aplasia that might be associated with a TGDC.
Unilateral absence of the submandibular glands (SMG aplasia) is rare, with only a few reported cases. A thyroglossal duct cyst (TGDC) with unilateral SMG aplasia is very rare, especially when there is a correlation between the TGDC and an ectopic SMG.
We report a case of unilateral SMG aplasia with TGDC. This case is unique because there TGDC might have developed as an ectopic SMG with the unilateral SMG aplasia in the same side.
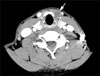
A 48-year-old man with an anterior neck mass, diagnosed as a thyroglossal duct cyst (TGDC), was referred to our hospital. His chief complaint was mild postprandial swelling of the cystic mass. Clinical examination of the oral cavity, oropharynx, and larynx was normal and no other mass was palpated in the neck. The mass in the anterior neck was soft on palpation and moved on swallowing. There was a palpable submandibular gland (SMG) on the right, but no palpable gland on the left on bimanual examination. No abnormalities were seen on the mouth floor, although slight swelling was observed in the left sublingual gland region, as compared to the right. No salivary flow was seen from the left Wharton's duct orifice in the mouth floor. Enhanced neck computed tomography (CT) demonstrated a 1.5 × 1.5 cm cystic mass in the left neck, below the hyoid bone and anterior to the thyroid cartilage (Fig. 1). The results of the clinical exam and CT of the neck were compatible with a TGDC. The TGDC was located on the superior part of the thyroid cartilage and there was no sign of adhesion to the thyroid cartilage or hyoid bone.
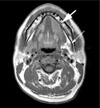
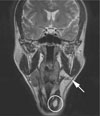
On subsequent magnetic resonance imaging (MRI), the left submandibular gland was absent and there was ipsilateral sublingual gland hypertrophy. The left submandibular space was replaced with fatty tissue (Fig. 2). In addition, left SMG aplasia and TGDC were seen, with fluid enhancement in the TGDC (Fig. 3). We recommended surgical excision of the TGDC to evaluate the relationship to the SMG aplasia, but the patient refused any further study, including fine needle aspiration biopsy (FNAB) to diagnose salivary fluid or tissue, or surgical removal.
Development of the submandibular salivary glands is first visible as a thickening of the epithelium next to the tongue around the prebud stage. The main duct of the salivary gland is visible as a slight dimple on the oral surface, where lumen formation has already begun. The parotid, submandibular, and sublingual glands appear during the 4th, 6th, and 9th weeks of gestation, respectively. The aplasia of the SMG is likely to be due to arrest in organogenesis.
In our patient, no accompanying anomalies were seen other than mild postprandial swelling of a TGDC. He also had ipsilateral compensatory sublingual hypertrophy, which is seen in many cases of unilateral SMG aplasia. He complained only of dryness of the mouth, but had no difficulty chewing or swallowing or increased incidence of dental caries, which are thought to be due to the reduction in the protective effect of saliva within the oral cavity.
Salivary gland aplasia may be associated with first branchial arch defects in Treacher-Collins syndrome (mandibulofacial dysostosis) or orbital abnormalities like lacrimal hypoplasia, canalicular atresia, and absence of the lacrimal puncta (1). Anomalies of the submandibular glands and ducts can appear as ranula and epidermal/dermal inclusion cysts (2). Congenital dilation of the submandibular duct can appear as a mucocele, ranula, dermoid and epidermoid cyst, TGDC, or branchial cleft cyst (BCC) (3). In all these cases, no submandibular tissue is detected in the cystic lesions. That is, SMG duct dilation is seen only as cystic lesions and the dilation is located closer to the submandibular area than the common location of a TGDC or other cystic lesions.
Based on these clues, there was little possibility of a relationship between the SMG and TGDC, especially without being able to conduct other examinations, including a biopsy. No cases of unilateral SMG aplasia with a TGDC have been reported.
There are two possible mechanisms for postprandial TGDC swelling in unilateral SMG aplasia. First, salivary flow from the normal SMG may enter the foramen cecum and pass into the TGDC, resulting in TGDC swelling after a meal. Second, postprandial saliva-producing stimulation might occur in the TGDC, resulting in TGDC swelling if it contains ectopic SMG tissue. Therefore, we still suspected a relationship between the TGDC and ectopic SMG, although it is possible that a TGDC might be found incidentally in a case of SMG aplasia. The clue suggesting that the TGDC in our case was an ectopic SMG was the postprandial swelling, we think that the possibility of a TGDC arising from an ectopic SMG is small. Although we did not perform surgery to identify the TGDC as an ectopic SMG, we cannot exclude the possibility of a close relationship between the TGDC and an ectopic SMG. Moreover, if a patient with ipsilateral SMG aplasia complained of post-prandial swelling of a concurrent TGDC, we would suspect that the TGDC might have arisen as an ectopic SMG with an abnormal path of Wharton's duct or duct obstruction.
If a patient is seen complaining of postprandial TGDC swelling, further radiological evaluation, such as CT or MRI, with a biopsy or surgery, are necessary to identify any ectopic SMG.
Figures and Tables
Fig. 1
The thyroglossal duct cyst (TGDC) is seen as a well-defined cystic mass (arrow) below the hyoid bone on enhanced CT (axial view). The TGDC is located above the left thyroid gland lobe and superior thyroid cartilage. There is no adhesion between the TGDC and surrounding structure.
References
1. Srinivasan A, Moyer JS, Mukherji SK. Unilateral submandibular gland aplasia associated with ipsilateral sublingual gland hypertrophy. AJNR Am J Neuroradiol. 2006; 27(10):2214–2216.
2. Pal K, Abdulla AM. Congenital imperforate submandibular duct in a newborn. Indian J Pediatr. 2007; 74(7):687–688.
3. Addante RR. Congenital cystic dilatation of the submandibular duct. Oral Surg Oral Med Oral Pathol. 1984; 58(6):656–658.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download