Abstract
Real-time cine MRI studies using the steady-state free precession (SSFP) technique are very useful for evaluating cardiac and septal motion. During diastole, the septum acts as a compliant membrane between the two ventricles, and its position and geometry respond to even small alterations in the trans-septal pressure gradients. Abnormal septal motion can be caused by an overload of the right ventricle, delayed ventricular filling and abnormal conduction. In this study, we illustrate, based on our experiences, the causes of abnormal septal motion such as corrective surgery for tetralogy of Fallot, an atrial septal defect, pulmonary thromboembolism, mitral stenosis, constrictive pericarditis and left bundle branch block. In addition, we discuss the significance of paradoxical septal motion in the context of cardiac MR imaging.
The septum normally shows a characteristic right convexity that is determined by a left-to-right positive transseptal pressure gradient, and this shape is maintained during the cardiac cycle (12). Changes in the position and geometry of the ventricular septum occur when there is an acute or chronic imbalance between the left and right ventricular loading conditions, such as a postoperative state of tetralogy of Fallot, an atrial septal defect, pulmonary thromboembolism, mitral stenosis, constrictive pericarditis or left bundle branch block (234). The phenomenon that alters the function of one ventricular function by changes in the filling of the other ventricle is called interventricular dependence or ventricular coupling (4). Delayed left ventricular filling leads to an abnormal trans-septal pressure gradient and this accentuates early diastolic septal movement, which gradually returns rightward when the left ventricular filling continues. Further, the anterior movement of the ventricular septum in systole can be detected during the cardiac cycle after coronary artery bypass grafting, although the cause of this is unclear (5). Doppler echocardiography is currently the first choice of image modalities for assessing septal motion. The advent of magnetic resonance imaging (MRI) with stronger and faster gradient systems has recently enabled evaluating the septal motion and the real-time dynamic contraction of the heart chambers, and this potentially gives cardiac MRI the same ability as that of echocardiography for evaluating septal motion and the real-time dynamic contraction of the heart chambers (6). The purpose of this study was to demonstrate the various MR images of paradoxical septal motion and to correlate these findings with the clinical appearances and pathophysiologic findings.
We recruited the patients who showed paradoxical septal motion on cardiac MRI and we retrospectively reviewed their medical records. All the MR images were acquired with the patients in the supine position and using a 1.5-T MRI system (Intera CV release 10; Philips Medical Systems, Best, Netherlands) with a flexible body array coil. The two or three four-chamber views and the two-chamber views, as well as the contiguous short-axis CINE images of the entire heart, were acquired with steady-state free precession (SSFP) (3 msec/1.5 msec, flip angle: 60°). For the short axis images, 8 mm slices were acquired at 9-12 base-to-apex short-axis locations during repeated breath holds (2~3 sec/slice). The ECG triggered sequence was used with various repetition times (TRs). The typical parameters were a repetition time of 3 to 4 ms, an echo time of 1 to 2 ms, a flip angle of 50° to 60°, a field of view of 270 × 270 mm and a matrix of 256 × 256.
Under normal conditions, the septum has a right convexity and this configuration is maintained during the cardiac cycle. This ventricular shape is caused by ventricular coupling or interventricular dependence, which is altered by the pressure changes during ventricle filling. Ventricular coupling is normally significantly influenced by the respiration. The intrathoracic pressure increases during expiration, and this increases the pulmonary venous return and left ventricular filling, and it diminishes the systemic venous return and right ventricular filling, whereas the opposite occurs during inspiration (Fig. 1).
Paradoxical septal motion or distortion of the interventricular septum has been reported in situations of right ventricular (RV) pressure and volume overload (7). In the presence of increased systolic pressure in the RV, the interventricular septum flattens and sometimes it even bows leftward into the left ventricle (LV). The flattening and bowing of the septum were quantitatively expressed as curvature and the obtained results suggested that septum curvature could be used as a marker of systolic RV hypertension. Changes in the position of the ventricular septum occur when there is an acute or chronic imbalance between the left and right ventricular loading conditions, which is called "altered ventricular coupling". Further, ventricular coupling is significantly influenced by the respiration. In particular, assessments of the impact of respiration on ventricular coupling are crucial for differentiating the patients with constrictive pericarditis from those with restrictive cardiomyopathy (RCM) (4).
Tetralogy of Fallot (TOF) is the most common congenital cyanotic heart disease in non-infants (8). Long-term follow-up studies have reported that following TOF repair, these patients may suffer from altered right and left ventricular dysfunction (8). This LV dysfunction may be partially related to paradoxical interventricular septal motion. For the patients with LV asynchrony after repair of their TOF repair, the progressive mechanical interaction between an enlarged failing RV and the LV that's mediated through paradoxical septal motion is a possible explanation for the LV asynchrony. The right ventricular volume overload in patients following corrective surgery for TOF is not the only cause of the paradoxical septal movements, and other factors such as the duration of preoperative hypoxia, the presence of myocardial fibrosis and the surgical repair techniques should not be ignored (9). The paradoxical septal motion in asymptomatic postoperative patients following TOF repair and who are without significant right ventricular volume overload is related to electrical delay and the reduced septal systolic function, and the latter is mainly secondary to the diminished regional septal systolic function and paradoxical septal motion (Fig. 2).
The paradoxical septal motion in patients with atrial septal defect (ASD) occurs due to right ventricular volume overload (10). In these patients, the degree of septal paradoxical motion is significantly related to the degree of volume overload. Paradoxical motion of the ventricular septum is usually observed by M-mode echocardiography at the level of the papillary muscles of the left ventricle, and this paradoxical septal motion is frequently seen in patients with ASD and who have more than moderate volume overload of the right ventricle (Fig. 3). It is well known that the upper part of the ventricular septum moves toward the anterior chest wall during systole, while the lower part of the ventricular septum moves toward the posterior wall. A pivot point is a hinge point for the wall motion of the ventricular septum during systole, and presumably also in diastole, and this hinge joint is believed to be located at the upper one third of the ventricular septum. Several causes for paradoxical ventricular septum motion have been proposed, yet the exact mechanism remains unclear.
Impaired left ventricular filling due to right ventricular pressure overload in patients with primary pulmonary hypertension has been described (11). Flattening of the interventricular septum is a certain sign of pulmonary hypertension, and negative curvature is only observed at systolic pressures higher than 67 mm Hg (12). Echocardiography can also be used to evaluate the septal curvature and to estimate the RV pressure or the pulmonary pressure. While the relative simplicity and low costs of echocardiography are certainly important arguments in its favor, its reliability is questionable. On the other hand, MRI can achieve high accuracy and reproducibility (Fig. 4).
Patients with mitral stenosis often have abnormal leftward motion of the ventricular septum during early diastole, which has been termed paradoxical diastolic septal motion, although it actually reflects an exaggeration of the normal slight posterior septal movement during this phase of the cardiac cycle. Some patients with mitral stenosis and atrial fibrillation show marked variability during diastolic filling. With continued filling of the left ventricle, the normal (left ventricle > right ventricle) trans-septal gradient is reestablished and the septum moves progressively rightward. Leftward motion is initiated at a time when the trans-septal gradient, although decreasing, is still substantially positive (left ventricle > right ventricle). The marked degree of early diastolic leftward motion that is characteristic of patients with mitral stenosis reflects an abnormal trans-septal gradient, which often is the reverse of the normal gradient (Fig. 5). Thompson et al. (13) demonstrated a tight linear correlation between the septal position and the transseptal gradient both at end-diastole and end-systole. Ryan et al. (14) used an eccentricity index to quantitate the degree of septal flattening and they showed that end-diastolic septal flattening occurs in patients with right ventricular volume-overload, and that those patients with right ventricular systolic pressures greater than 45 mm Hg (pressure overload) also had septal flattening at end-systole. Depending on the degree of leftward septal displacement, the septal motion during subsequent systole may be reduced leftward, flattened or reversed (paradoxic septal motion).
The main characteristic of constrictive pericarditis (CP) is a thickened, fibrotic and/or calcified pericardium that constricts the heart and impairs cardiac filling. One of the main manifestations of CP is increased ventricular interdependence, a phenomenon whereby the function of one ventricle is altered by changes in the filling of the other ventricle (3). Because the pericardial sac has a fixed volume in patients with CP, the position of the ventricular septum during diastole depends on the filling characteristics of both ventricles. This phenomenon of pathologic ventricular coupling, or increased ventricular dependence, is a major direct cause of pericardial inflexibility. Accordingly, the filling pressures are increased, and during early diastole, the rate of filling is rapid and the rate of change of the ventricular pressure is particularly rapid. This rapid change in ventricular pressure can lead to abrupt changes in the septal position with septal flattening or eventually septal inversion (paradoxical motion) (3). Furthermore, this ventricular septal shift is influenced by respiration. In addition, the ventricular interdependence is increased by the presence of a noncompliant pericardium, which impedes the outward movement of the ventricular free wall during filling. Accordingly, the instantaneous diastolic transseptal gradient changes and this leads to septal reconfiguration and paradoxical motion during filling. This phenomenon is enhanced during inspiration since the decreased intra thoracic pressure in patients with CP is not transmitted to the ventricles because of the thickened fibrotic pericardium (Fig. 6).
The abnormal interventricular activation and mechanical asynchrony in patients with LBBB may result in dynamic changes throughout the cardiac cycle in terms of both the pressure differentials and the ventricular volumes (15). These differences in transseptal pressures and volumes may cause septal displacement. The onset of right ventricular contraction occurs before that of the left ventricle in patients with LBBB. As a result, the increased pressure during right ventricular isovolumic systole presumably exceeds the left ventricular end-diastolic pressure and the septum is displaced into the left ventricle. Furthermore, the upstroke of the right ventricular systolic pressure occurs earlier than that of the left ventricle, and the septum is abruptly displaced into the left ventricle because of the reversal of the transseptal pressure gradient (211). Abrupt anterior septal motion occurs at the time of decreasing right ventricular volume with pulmonic ejection. In addition, left ventricular systole begins at this time and this normalizes the transseptal pressure gradient, which moves the septum toward its equilibrium position. Tricuspid valve opening and right ventricular filling occur much earlier than mitral valve opening and left ventricular filling, and the resultant additional right ventricular volume may be responsible for the early diastolic displacement of the septum into the left ventricle. The direction of the systolic septal motion may be influenced by the septal position during diastole. Displacement of the septum in LBBB patients may occur as a result of a relative increase in the right ventricular volume or pressure (the right ventricular contraction during left ventricular end-diastole). The diastolic displacement of the septum in LBBB patients reduces the paradoxic systolic septal motion and it diminishes the septal contribution to the ejection fraction (Fig. 7).
We conclude that an understanding of the imaging findings and the causes of paradoxical septal motion are important in terms of achieving accurate diagnoses and for analyzing the various regional abnormalities of the LV. Furthermore, given the expected advances in MRI technology, we are confident that MRI will play an increasingly important role in assessing the abnormal regional movements of the LV.
Figures and Tables
Fig. 1
The real-time cine-MR images acquired in a midventricular short-axis plane during deep inspiratory and expiratory movements in a normal subject. The ventricular septum shows a convex shape towards the right ventricle at end diastole. The septal position and configuration are not modified by respiratory activity during the cardiac cycle. The horizontal dotted line shows the level of the diaphragm at end-inspiration. DA (DL) means that distance measured from the reference point to the anterior border of the septum (the posterior border of the lateral wall). R: stationary anterior reference point, Ex-ED: expiration-end diastole, Ins-ED: inspiration-end diastole, ES: end systole.

Fig. 2
A 21-year-old man with complete repair of tetralogy of Fallot. The early systolic paradoxical septal motion (convex toward the left ventricle, arrowed) and the sustained paradoxical motion during mid-late systole are shown. DA (DL) means that distance measured from the reference point to the anterior border of the septum (the posterior border of the lateral wall). R: stationary anterior reference point, ED: end diastole, ES: end systole.

Fig. 3
A 35-year-old woman with the sinus venous type ASD. Systolic anterior motion of the ventricular septum parallel to the posterior wall of the left ventricle is evident (arrowed). In addition, enlargement of the right ventricle, which indicates more than a moderate volume overload, is shown. ED: end diastole, ES: end systole (Image courtesy of Kim YJ, Yonsei University Severance Hospital).

Fig. 4
Diastolic flattening of the septal wall in the short-axis view of a 57-year-old man with pulmonary thromboembolism.
A. Massive thromboemboli in the right main pulmonary artery (arrowed) and pericardial effusion.
B. During diastole, marked inward bending of the interventricular septum toward the left ventricle was observed (arrows).
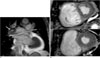
Fig. 5
Early diastolic septal flattening depicted in the short-axis view of a 63-year-old man with mitral stenosis. During early filling, the septum (arrowed) flattened, but it regained a normal appearance at the end of diastolic filling.

Fig. 6
Early diastolic septal flattening depicted in the short-axis view of a 54-year-old woman with constrictive pericarditis. During early filling, the septum (arrowed) flattened, but it regained a normal appearance at the end of diastolic filling. DA (DL) means that distance measured from the reference point to the anterior border of the septum (the posterior border of the lateral wall). R: stationary anterior reference point, ED: end diastole, ES: end systole.

Fig. 7
Pre-ejection of septal motion depicted in the short-axis view of a 63-year-old man with LBBB. Right ventricular contraction in the LBBB patient occurs much earlier (eS) than the left ventricular systole and this is associated with an abrupt displacement of the interventricular septum into the left ventricle. Therefore, the septum in early systole adopts a more inner position compared to that in end systole. eS: early systole, ES: end systole, ED: end diastole

References
1. Lima JA, Guzman PA, Yin FC, Brawley RK, Humphrey L, Traill TA, et al. Septal geometry in the unloaded living human heart. Circulation. 1986; 74:463–468.
2. Weyman AE, Wann S, Feigenbaum H, Dillon JC. Mechanism of abnormal septal motion in patients with right ventricular volume overload: a cross-sectional echocardiographic study. Circulation. 1976; 54:179–186.
3. Giorgi B, Mollet NR, Dymarkowski S, Rademaakers FE, Bogaert J. Clinically suspected constrictive pericarditis: MR imaging assessment of ventricular septal motion and configuration in patients and healthy subjects. Radiology. 2003; 228:417–424.
4. Francone M, Dymarkowski S, Kalantzi M, Bogaert J. Real-time cine MRI of ventricular septal motion: a novel approach to assess ventricular coupling. J Magn Reson Imaging. 2005; 21:305–309.
5. Joshi SB, Salah AK, Mendoza DD, Goldstein SA, Fuisz AR, Lindsay J. Mechanism of paradoxical ventricular septal motion after coronary artery bypass grafting. Am J Cardiol. 2009; 103:212–215.
6. Dong SJ, Crawley AP, MacGregor JH, Petrank YF, Bergman DW, Belenkie I, et al. Regional left ventricular systolic function in relation to the cavity geometry in patients with chronic right ventricular pressure overload: a three-dimensional tagged magnetic resonance imaging study. Circulation. 1995; 91:2359–2370.
7. King ME, Braun H, Goldblatt A, Liberthson R, Weyman AE. Interventricular septal configuration as a predictor of right ventricular systolic hypertension in children: a cross-sectional echocardiographic study. Circulation. 1983; 68:68–75.
8. Vliegen HW, van Straten A, de Roos A, Roest AA, Schoof PH, Zwinderman AH, et al. Magnetic resonance imaging to assess the hemodynamic effects of pulmonary valve replacement in adults late after repair of tetralogy of Fallot. Circulation. 2002; 106:1703–1707.
9. Abd El Rahman MY, Hui W, Dsebissowa F, Schubert S, Gutberlet M, Hetzer R, et al. Quantitative analysis of paradoxical interventricular septal motion following corrective surgery of tetralogy of fallot. Pediatr Cardiol. 2005; 26:379–384.
10. Popio KA, Gorlin R, Teichholz LE, Cohn PF, Bechtel D, Herman MV. Abnormalities of left ventricular function and geometry in adults with an atrial septal defect. Ventriculographic, hemodynamic and echocardiographic studies. Am J Cardiol. 1975; 36:302–330.
11. Marcus JT, Vonk Noordegraaf A, Roeleveld RJ, Postmus PE, Heethaar RM, Van Rossum AC, et al. Impaired left ventricular filling due to right ventricular pressure overload in primary pulmonary hypertension: noninvasive monitoring using MRI. Chest. 2001; 119:1761–1765.
12. Roeleveld RJ, Marcus JT, Faes TJ, Gan TJ, Boonstra A, Postmus PE, et al. Interventricular septal configuration at MR imaging and pulmonary arterial pressure in pulmonary hypertension. Radiology. 2005; 234:710–717.
13. Thompson CR, Kingma I, MacDonald RP, Belenkie I, Tyberg JV, Smith ER. Transseptal pressure gradient and diastolic ventricular septal motion in patients with mitral stenosis. Circulation. 1987; 76:974–980.
14. Ryan T, Petrovic O, Dillon JC, Feigenbaum H, Conley MJ, Armstrong WF. An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol. 1985; 5:918–927.
15. Grines CL, Bashore TM, Boudoulas H, Olson S, Shafer P, Wooley CF. Functional abnormalities in isolated left bundle branch block. Circulation. 1989; 79:845–853.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download