Abstract
Purpose
To retrospectively review the effectiveness and safety of fluoroscopic and US-guided percutaneous transgluteal drainage of postoperative pelvic abscesses.
Materials and Methods
From January 2002 to December 2007, 594 patients underwent surgery at our institution due to rectosigmoid cancer. A retrospective analysis revealed that percutaneous drainage of a postoperative pelvic abscess was performed in 19 out of the 594 patients (3.19%) that underwent surgery (13 male, 6 female; mean age, 57.9 years; age range, 40-82 years). The transgluteal and other methods were used for percutaneous drainage and the success rate, duration of therapy, and complication rate were evaluated.
Results
The transgluteal approach was performed with fluoroscopic and US-guidance in 10 patients (52.6%). A catheter was inserted through a preexisting surgical drain in 5 patients (26.3%). The transabdominal approach was performed under US-guidance in 4 patients (21.0%). Technical success was achieved in all patients. The catheter was removed after a mean of 14 days. In 2 patients, who were treated by the transgluteal apporoach, subsequent surgery was performed due to incomplete resolution of the abscess (10.5%). The mean duration of catheter drainage using the transgluteal approach (16.5 days) was longer than other methods (11.2 days). Furthermore, no procedure-related major complications or mortality was observed in all methods.
Figures and Tables
 | Fig. 1A 40-year-old man with pelvic abscess.A. CT scan through mid pelvis shows cephalic portion of the greater sciatic foramen. superior gluteal vessel (sgvs) and sciatic nerve (scn) coursing through the upper portion of the greater sciatic foramen (gsf). ub = urinary bladder, sgvs = superior gluteal vessels, scn = sciatic nerve, gsf = greater sciatic foramen, prf = piriformis muscle
B. CT scan through the caudal portion of the greater sciatic foramen shows sacrospinous ligament (ssl). Note the internal pudendal vessels (ipvs) and inferior gluteal vessels (igvs) located lateral aspect of the greater sciatic foramen (gsf). There were also noted abscess (a) in presacral area. p = prostate, oi = obturator internus muscle
|
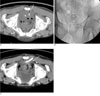 | Fig. 240-year-old man diagnosed and treated for rectal adenocarcinoma developed fever and leukocytosis 10 days after surgery.A. Axial CT image shows a fluid collection with air bubbles at presacral space (*) above anastomosis site. Arrow indicates direction of Chiba needle.
B. 10.2 F pigtail catheter was inserted successfully into the presacral abscess by fluoroscopic and US-guided transgluteal approach.
C. 2 months after, follow up CT shows 10.2 F drainage catheter which traverse the sacrospinous ligament (arrow). Inferior gluteal vessels (arrowhead) are seen more lateral aspect of the catheter. Note the decreased size of the presacral abscess.
|
 | Fig. 359-year-old man diagnosed and treated for rectal neuroendocrine carcinoma developed fever and abdominal pain 6 months after surgeryA. Axial CT image show fluid collection at presacral space (*). Arrow indicates direction of Chiba needle.
B. 18 G Chiba needle was inserted into presacral abscess by fluoroscopic and US-guided transgluteal approach.
C. 10.2 F drainage catheter was inserted successfully.
|
References
1. Welch CE, Malt RA. Abdominal surgery (first of three parts). N Engl J Med. 1983; 308:624–632.
2. Welch CE, Malt RA. Abdominal surgery (second of three parts). N Engl J Med. 1983; 308:685–695.
3. Welch CE, Malt RA. Abdominal surgery (third of three parts). N Engl J Med. 1983; 308:753–760.
4. Varghese JC, O'Neill MJ, Gervais DA, Boland GW, Mueller PR. Transvaginal catheter drainage of tuboovarian abscess using the trocar method: technique and literature review. AJR Am J Roentgenol. 2001; 177:139–144.
5. Gazelle GS, Haaga JR, Stellato TA, Gauderer MW, Plecha DT. Pelvic abscesses: CT-guided transrectal drainage. Radiology. 1991; 181:49–51.
6. Pereira JK, Chait PG, Miller SF. Deep pelvic abscesses in children: transrectal drainage under radiologic guidance. Radiology. 1996; 198:393–396.
7. Whelan MA, Gold RP. Computed tomography of the sacrum: 1. Normal anatomy. AJR Am J Roentgenol. 1982; 139:1183–1190.
8. Whelan MA, Hilal SK, Gold RP, Luken MG, Michelson WJ. Computed tomography of the sacrum: 2. Pathology. AJR Am J Roentgenol. 1982; 139:1191–1195.
9. Wechsler RJ, Schilling JF. CT of the gluteal region. AJR Am J Roentgenol. 1985; 144:185–190.
10. Federle MP, Moss AA, Margolin FR. Role of computed tomography in patients with "Sciatica". J Comput Assist Tomogr. 1980; 4:335–341.
11. Butch RJ, Mueller PR, Ferrucci JT, Wittenberg J, Simeone JF, White EM, et al. Drainage of pelvic abscesses through the greater sciatic foramen. Radiology. 1986; 158:487–491.
12. Harisinghani MG, Gervais DA, Maher MM, Cho CH, Hahn PF, Varghese J, et al. Transgluteal approach for percutaneous drainage of deep pelvic abscesses: 154 cases. Radiology. 2003; 228:701–705.
13. Walser E, Raza S, Hernandez A, Ozkan O, Kathuria M, Akinci D. Sonographically guided transgluteal drainage of pelvic abscesses. AJR Am J Roentgenol. 2003; 181:498–500.
14. Cahill AM, Baskin KM, Kaye RD, Fitz CR, Towbin RB. Transgluteal approach for draining pelvic fluid collections in pediatric patients. Radiology. 2005; 234:893–898.
15. Gervais DA, Hahn PF, O'Neill MJ, Mueller PR. CT-guided transgluteal drainage of deep pelvic abscesses in children: selective use as an alternative to transrectal drainage. AJR Am J Roentgenol. 2000; 175:1393–1396.
16. Gervais DA, Ho CH, O'Neill MJ, Arellano RS, Hahn PF, Mueller PR. Recurrent abdominal and pelvic abscesses: incidence, results of repeated percutaneous drainage, and underlying causes in 956 drainages. AJR Am J Roentgenol. 2004; 182:463–466.
17. Maher MM, Gervais DA, Kalra MK, Lucey B, Sahani DV, Arellano R, et al. The inaccessible or undrainable abscess: how to drain it. Radiographics. 2004; 24:717–735.
18. Gervais DA, Brown SD, Connolly SA, Brec SL, Harisinghani MG, Mueller PR. Percutaneous imaging-guided abdominal and pelvic abscess drainage in children. Radiographics. 2004; 24:737–754.
19. Woo JK, Millward SF. Transgluteal approach for percutaneous drainage of deep pelvic abscesses: how to avoid injury to vital structures. Radiology. 2004; 233:300–301.
20. Harisinghani MG, Gervais DA, Hahn PF, Cho CH, Jhaveri K, Varghese J, et al. CT-guided transgluteal drainage of deep pelvic abscesses: indications, technique, procedure-related complications, and clinical outcome. Radiographics. 2002; 22:1353–1367.
21. Gupta S, Nguyen HL, Morello FA, Ahrar K, Wallace MJ, Madoff DC, et al. Various approaches for CT-guided percutaneous biopsy of deep pelvic lesions: anatomic and technical considerations. Radiographics. 2004; 24:175–189.
22. Ryan JM, Murphy BL, Boland GW, Mueller PR. Use of the transgluteal route for percutaneous abscess drainage in acute diverticulitis to facilitate delayed surgical repair. AJR Am J Roentgenol. 1998; 170:1189–1193.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download