Abstract
Glucocorticoids are widely used as potent anti-inflammatory and immunosuppressive drugs to treat a wide range of diseases. However, they are also associated with a number of side effects, including new-onset hyperglycemia in patients without a history of diabetes mellitus (DM) or severely uncontrolled hyperglycemia in patients with known DM. Glucocorticoid-induced diabetes mellitus (GIDM) is a common and potentially harmful problem in clinical practice, affecting almost all medical specialties, but is often difficult to detect in clinical settings. However, scientific evidence is lacking regarding the effects of GIDM, as well as strategies for prevention and treatment. Similarly to nonsteroid-related DM, the principles of early detection and risk factor modification apply. Screening for GIDM should be considered in all patients treated with medium to high doses of glucocorticoids. Challenges in the management of GIDM stem from wide fluctuations in postprandial hyperglycemia and the lack of clearly defined treatment protocols. Together with lifestyle measures, hypoglycemic drugs with insulin-sensitizing effects are indicated. However, insulin therapy is often unavoidable, to the point that insulin can be considered the drug of choice. The treatment of GIDM should take into account the degree and pattern of hyperglycemia, as well as the type, dose, and schedule of glucocorticoid used. Moreover, it is essential to instruct the patient and/or the patient's family about how to perform the necessary adjustments. Prospective studies are needed to answer the remaining questions regarding GIDM.
Glucocorticoids have been shown to be potent anti-inflammatory and immunosuppressive drugs; they started to be used for therapeutic purposes in the mid-20th century, and are currently widely used in the treatment of many diseases [1]. At any point in time, up to 0.9% of the general population may be using cor-ticosteroids, with the highest rate of use (2.5%) seen in individuals 70 to 79 years of age. Moreover, nearly one-quarter of patients may need to use corticosteroids for more than 6 months [2]. Glucocorticoids are extensively used in almost every subspecialty of medicine [3]. Although they are widely prescribed for their anti-inflammatory and immunosuppressive properties, glucocorticoids have a range of common metabolic side effects including hypertension, osteoporosis, and diabetes [2]. Glucocorticoid-induced diabetes mellitus (GIDM) has been recognized as a complication of glucocorticoid use for over 60 years [4]. Glucocorticoids are the drug group most often associated with the onset of hyperglycemia or diabetes mellitus [1]. Glucocorticoids exacerbate hyperglycemia in patients with diabetes mellitus, unmask undiagnosed diabetes mellitus or may precipitate the appearance of GIDM, which is an independent risk factor for other complications associated with the use of these drugs [2]. Furthermore, although it is expected that the blood glucose levels of non-diabetic patients should normalize after discontinuing glucocorticoid use, this does not always happen, and such patients require close monitoring due to the risk of developing diabetes mellitus in the future [5].
The diagnosis and treatment of GIDM are surprisingly undervalued by many health-care professionals, although GIDM results in an increased use of medical care and the development of associated morbidities that affect medical costs and patients' quality of life [2]. Despite the high prevalence of corticosteroid use in clinical practice and the strong association of glucocorticoids with new-onset hyperglycemia, limited information is available regarding the pathophysiology, frequency, and diagnosis of this condition. Similarly, prospective studies assessing the effectiveness of preventive measures taken against this condition and comparing the effectiveness of different treatment schedules are lacking. Therefore, the primary goal of this review article was to highlight the most recent evidence regarding the clinical aspects of GIDM.
The incidence of glucocorticoid-induced hyperglycemia has been reported to be 12% [6]. Other studies of the prevalence of GIDM associated with different diseases have reported varying results [789]. However, the exact prevalence of hyperglycemia secondary to glucocorticoid therapy is not known, making this an unpredictable challenge for general practitioners and endocrinologists alike [5]. Gulliford et al. [10] reported that 2% of incident cases of diabetes were associated with oral glucocorticoids in a primary care population. The prevalence of abnormal glucose metabolism in patients with an organ transplant who undergo glucocorticoid therapy has been reported to be 17% to 32% [11]. GIDM has been reported to have an even greater prevalence among patients treated with glucocorticoids for rheumatoid arthritis [12]. A recent meta-analysis indicated that the rates of glucocorticoid-induced hyperglycemia and diabetes were 32.3% and 18.6%, respectively [13]. The length of time on glucocorticoids, the relative potency of the glucocorticoid and the absolute dose all play a role in the occurrence of GIDM [14]. The odds ratio for presenting with new-onset diabetes after taking glucocorticoids in various studies has been reported to range from 1.36 to 2.31 [10].
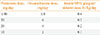
It is unlikely that the development of hyperglycemia is related only to the existence of an underlying disease, because abnormalities in glucose metabolism have also been observed in experimental studies with healthy subjects. The incidence of hyperglycemia (defined as blood glucose >200 mg/dL) in hospitalized patients without a known history of diabetes who are treated with corticosteroids is over 50% [7]. Not all patients who use glucocorticoids develop GIDM, suggesting that GIDM occurs only in vulnerable populations. A number of predictors of the onset of GIDM have been identified [12915]. These predictors include the dose and duration of glucocorticoid treatment, age, weight, previous glucose intolerance, reduced sensitivity to insulin or impaired insulin secretion stimulated by glucose, a family history of diabetes, or race, as shown in Table 1. Gender does not seem to be a predictor and, conversely, early withdrawal from corticosteroids is a protective factor [12915]. Various glucocorticoids differ in their pharmacological properties and duration of action, and can be administered in different schedules depending on the therapeutic indication. These drugs may cause hyperglycemia when administered at supraphysiological doses by any route (topical, oral, inhaled, intramuscular, intravenous, or intra-articular) [10].
The effects of glucocorticoids on glucose homeostasis are complex and not completely understood. Their negative effects are believed to be caused by a variety of factors, including increased insulin resistance, increased glucose intolerance, reduced β-cell mass from β-cell dysfunction, and increased hepatic insulin resistance leading to impaired suppression of hepatic glucose production [1617]. The metabolic effects of glucocorticoids on glucose metabolism are seen at numerous stages in the insulin-signaling cascade [5]. Prednisolone administration for 7 days in healthy volunteers led to a 50% reduction in insulin sensitivity, as assessed using the insulin clamp methodology [18]. The effect of glucocorticoids on glucose metabolism likely results from the impairment of multiple pathways, including β-cell dysfunction (sensitivity to glucose and ability to release insulin) and insulin resistance in other tissues [3]. Glucocorticoids reduce peripheral glucose uptake at the level of the muscle and adipose tissue [1920]. Skeletal muscle is primarily responsible for the insulin-mediated capture of postprandial glucose and corticosteroids can induce insulin resistance by interfering directly with various components of the insulin signaling cascade [1921]. Chronic glucocorticoid overexposure alters body composition, including the expansion of adipose tissue depots in the trunk, and impairs metabolism and insulin action, resulting in hyperglycemia and dyslipidemia [16]. The ability of glucocorticoids to induce adipose tissue lipolysis depends on their concentration, duration of exposure, and the specific adipose tissue depot [16]. The liver plays a major role in the control of glucose metabolism, maintaining fasting euglycemia. Corticosteroids increase endogenous glucose production directly by activating numerous genes involved in the hepatic metabolism of carbohy-drates, leading to increased gluconeogenesis [1922]. Glucocorticoids also inhibit the production and secretion of insulin from pancreatic β-cells [2324]. The abilities of glucocorticoids to induce hyperglycemia depend on their dose and the duration of exposure [1625]. In addition to insulin resistance, inflammatory disease states themselves may induce β-cell dysfunction through indirect mechanisms [11]. The mechanisms of glucocorticoid-induced hyperglycemia are summarized in Table 2.
There are several reasons why glucocorticoid-induced hyperglycemia is important in clinical practice. First, it is quite common, and the problems of hyperglycemia itself, which are often severe, may cause hospitalization, prolonged hospital stays, or repeated emergency room visits. Second, glucocorticoids increase the risk of infection due to persistent hyperglycemia, which has a deleterious effect on patients' prognoses. Moreover, the control of transient hyperglycemia in similar situations during hospitalization has been associated with decreased mortality and complication rates [262728]. Most inpatients given glucocorticoids at a dose at least equivalent to 40 mg/day for more than 2 days develop hyperglycemia [11]. It is well known that glucocorticoid therapy may provoke new-onset type 2 diabetes mellitus (T2DM) and invariably worsens hyperglycemia in patients with preexisting diabetes mellitus [10]. Glucocorticoids are a well-known cause of hyperosmolar hyperglycemic nonketotic syndrome [28], which requires admission to the hospital for aggressive hydration and insulin therapy. The tendency for high-risk patients to develop new-onset hyperglycemia is often not anticipated, and outpatients with new-onset GIDM frequently require hospitalization for intravenous hydration and initiation of insulin therapy. In addition, hyperglycemia in hospitalized patients (with or without diabetes) has been associated with poor outcomes regardless of the underlying cause [17]. Inpatient hyperglycemia is known to be associated an increased length of stay and a greater incidence of infections [27]. In addition, sustained glucocorticoid treatment increases the potential for future cardiovascular disease through multiple pathways [11]. Glucocorticoids are administered using different schedules, doses, and methods, and it is possible that the mode of administration (e.g., inhaled, injected, or topical) and dosing regimen may affect the development of hyperglycemia [2]. Knowledge of these hyperglycemia patterns is essential to establish the most appropriate strategy for diagnosis and therapy.
GIDM is defined as an abnormal increase in blood glucose associated with the use of glucocorticoids in a patient with or without a prior history of diabetes mellitus. The diagnosis of GIDM, as well as other types of diabetes, is set according to the criteria established by expert committees [29]. The current criteria for diagnosing diabetes are an 8-hour fasting blood glucose level ≥7.0 mmol/L (126 mg/dL), a 2-hour post-75 g oral glucose tolerance test (OGTT) ≥11.1 mmol/L (200 mg/dL), a hemoglobin A1c (HbA1c) percentage ≥6.5%, or in patients with symptoms of hyperglycemia, a random plasma glucose reading ≥11.1 mmol/L (200 mg/dL) [29].
It is generally thought that glucocorticoids result mainly in an increase in postprandial blood glucose levels [30]. The use of a continuous blood glucose monitor in chronic obstructive pulmonary disease patients treated with prednisolone demonstrated that hyperglycemia predominantly occurred in the afternoon and evening, indicating that this would be the most appropriate time to screen for GIDM as well as the preferable time to implement specific treatments [31]. In patients treated with most glucocorticoids, measuring fasting blood glucose can underestimate glucocorticoid-induced hyperglycemia and diabetes, particularly in intermediate-acting treatments that are administered in single morning doses. However, given the pathophysiology and pattern of glucocorticoid-induced hyperglycemia, it can be inferred that the established criteria [29] provide a low diagnostic sensitivity in most patients with GIDM. For most glucocorticoids, measuring fasting blood glucose can underestimate glucocorticoid-induced hyperglycemia and diabetes, especially in cases of intermediate-acting glucocorticoid treatment with single morning doses [11]. On the contrary, postprandial glycemia after lunch offers the greatest diagnostic sensitivity. Preprandial glycemia at dinner offers less sensitivity, but is easier to standardize [11]. Blood glucose monitoring should be considered for non-diabetic patients who are at high risk of developing GIDM as shown in Table 1 [5]. In addition, an OGTT should also be performed as early as to detect diabetes in those deemed to be at risk [32]. However, the OGTT does not seem suitable for the diagnosis of GIDM because, apart from the difficulties associated with its implementation, it is performed in fasting patients and may underestimate the increase in glucose levels that occurs predominantly in the evening [2]. HbA1c may be a suitable method for diagnosis in patients treated with corticosteroids for >2 months, but it is not useful for patients whose treatment has been initiated more recently. Recently, Japanese scientists developed a detection algorithm for GIDM and suggested that monitoring changes in HbA1c levels is important for detecting GIDM [33]. In patients where HbA1c levels could be unreliable, such as those with hemoglobinopathies, renal failure, or anemia/recent blood transfusion, fructosamine measurements would be a better alternative [5]. In order to appreciate the magnitude of GIDM, one needs to consider that glucocorticoids cause predominantly postprandial hyperglycemia and therefore, using impaired fasting glucose as the sole diagnostic criterion, may underestimate the true incidence of GIDM. Therefore, the most useful criterion for the diagnosis of GIDM in most patients is a glucose level >200 mg/dL at any time of the day [2].
In patients with pre-existing diabetes or risk factors for GIDM, screening should be performed even when low doses of corticosteroids are indicated [2]. However, no glucose monitoring was performed in 24% of patients receiving high-dose glucocorticoid therapy [7]. Failure to appreciate the frequency of hyperglycemia in patients without diabetes is associated with the time course of corticosteroid action with prednisone or prednisolone given once daily [7]. No consensus exists for the optimal screening frequency. Some authors recommend screening with a once- to twice-weekly 2-hour post-lunch capillary blood glucose test in patients who are not known to be diabetic, but who are at a high risk of GIDM [5]. The American Diabetes Association further recommended that glucose monitoring be conducted in patients without known diabetes who receive therapies with a high risk of hyperglycemia, such as parenteral or enteral nutrition, glucocorticoids, immunosuppressive therapy, or octreotide [26]. The Endocrine Society recommended that all patients have blood glucose levels tested on admission, regardless of whether they have a pre-existing diagnosis of diabetes [27]. This approach is believed to be warranted by the opportunity to diagnose new diabetes and to assess glycemic control early course of hospitalization. Gonzalez-Gonzalez et al. [34] reported that, 50% of the time, GIDM occurred between the 2nd and 4th week. Therefore, continued blood glucose monitoring is advisable before meals and at bedtime in patients who exhibit hyperglycemia, and is definitely recommended for those who require anti diabetic medications.
Efforts to minimize hyperglycemic episodes are beneficial for patients exposed to glucocorticoids. Fluctuations in plasma glucose concentrations have shown an increased risk of cardiovascular mortality [35]. As is the case for diagnosis, no clear evidence exists for the establishment of therapeutic goals in patients with GIDM. From a practical standpoint, we recommend that the treatment of corticosteroid-induced hyperglycemia be considered when the preprandial and postprandial capillary glucose levels are ≥140 and ≥200 mg/dL, respectively. In the case of chronic treatment with glucocorticoids at more or less stable doses, the control goals and the need for drug treatment can be based on the recommended control aims for most patients with diabetes mellitus: preprandial glycemia <130 mg/dL, postprandial glycemia <180 mg/dL, and HbA1c <7% [2627]. Similarly to the recommendations for T2DM, the introduction of therapeutic measures should be progressive and additive. The selection strategy for hypoglycemic drugs should prioritize those with a mechanism of action that fits with the pathophysiology of the process and the patient's hyperglycemic profile. In the posttransplant setting, as more studies will be conducted with these and other agents, it is essential to focus attention to on drug—drug interactions is essential.
At present, no consensus guidelines exist for the optimal management of hyperglycemia secondary to glucocorticoids, although various opinions have been published by international organizations. There is no evidence to confirm which hypoglycemic drugs and treatment regimens are more effective in achieving adequate glycemic control and lowering complication rates in patients with glucocorticoid-induced hyperglycemia [2]. Therefore, the recommendations proposed in the present review are based on the pathophysiology of the process, the mechanism of action of various hypoglycemic drugs, and few clinical studies. First, it is important to evaluate the degree of pre-existing glucose intolerance, the patient's clinical condition, and the degree of hyperglycemia. Second, it is essential to determine the type, dose, and frequency of administration of the corticosteroid compound. Third, it is necessary to recognize the mechanism of action, pharmacokinetics, and pharmacodynamics of various hypoglycemic drugs. The final relevant aspect of addressing the treatment of GIDM is to differentiate between temporary and indefinite treatment with glucocorticoids. All these aspects condition the selection and schedule of hypoglycemic measures, as well as the goals set in terms of glycemic control. Together with, or after, lifestyle measures, hypoglycemic drugs with insulin-sensitizing effects are indicated. Other oral hypoglycemic drugs or insulin therapy can be considered as the second drug of choice [2]. As second drugs of choice, pioglitazone, sulfonylureas, glinides, dipeptidylpeptidase 4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists or insulin therapy can be considered, taking into account their profile of action, tolerance, cost, and risk for hypoglycemia, especially at night [1].
As with all types of diabetes, the initial steps to improve glycemic control incorporate lifestyle modifications, which include exercise and dietary counseling to provide options that may reduce postprandial hyperglycemia [3].
Theoretically, of the entire range of oral agents that can be used to treat glucocorticoid-induced or glucocorticoid-exacerbated diabetes, preference should be given to agents that target postprandial hyperglycemia and have a rapid onset of action. The information currently available in the literature suggests that oral agents do not adequately control hyperglycemia in hospitalized patients, and that sliding-scale regimens have resulted in hypoglycemia [17]. For these reasons, the use of oral hypoglycemic drugs is reserved for the treatment of mild glucocorticoid-induced hyperglycemia (glycemia <200 mg/dL) in patients without known diabetes or with diabetes adequately controlled by lifestyle measures or oral hypoglycemic drugs [2]. In the absence of studies comparing different strategies, the choice of the oral hypoglycemic drug should depend on the type and schedule of the corticosteroid and on the potential advantages and disadvantages of oral hypoglycemic drugs.
Together or after lifestyle measures, metformin and, in cases of intolerance or contraindication to metformin, pioglitazone are useful and can be considered the first choice in patients who receive chronic treatment with low doses of intermediate-acting glucocorticoids administered in the morning [1]. The characteristics of metformin and pioglitazone that contribute to their selection include their insulin-sensitizing effect, which avoids the risk of hypoglycemia, and the low cost of metformin. The dose and use of these drugs in GIDM does not differ from other clinical settings. Metformin is an attractive option because it enhances insulin sensitivity; thus, preventing metabolic side effects during systemic glucocorticoid therapy [36]. However, many patients treated with glucocorticoids receive treatment for conditions associated with hypoxia and renal insufficiency, which are both at least relative contraindications to the use of metformin because of the increased risk of lactic acidosis. In patients requiring long-term glucocorticoid use, metformin could be a reasonable choice given acceptable renal and liver function. Thiazolidinediones (TZDs) may improve diabetes-related parameters by antagonizing the pathways of glucocorticoid-induced insulin resistance and by reversing the adverse effects of glucocorticoids on β-cell function [37]. Therefore, the use of TZDs, such as pioglitazone in GIDM has also been suggested [38]. These agents have been used for the long-term treatment of transplant-induced diabetes mellitus with some success in combination with other agents [38]. Vu et al. [39] also reported the added benefit of increased progression-free survival with the use of metformin and TZDs in acute lymphoblastic leukemia. However, the usefulness of metformin and pioglitazone in the treatment of transient corticosteroid-induced hyperglycemia is limited due to their slow onset of action [2].
Oral secretagogues such as sulfonylurea therapy do not specifically target postprandial hyperglycemia and thus long-acting agents may be associated with hypoglycemia if the patient does not eat meals regularly. In cases where hyperglycemia is induced by intermediate-acting glucocorticoids in 2 or more daily doses, by long-term preparations such as dexamethasone, or by intra-articular glucocorticoids, sulfonylureas may also be a useful therapeutic option because their hyperglycemic effect lasts for 24 hours and the risk of nocturnal hypoglycemia is relatively low [2]. Second-generation sulfonylureas, such as gliclazide, are mainstays of oral treatment due to their rapid onset of action [5]. Doses are most appropriately given at lunch time to target postprandial hyperglycemia. If hyperglycemia remains an issue at a near-maximum dose, initiation of insulin should be contemplated rather than the addition of an alternative oral hypoglycemic agent as they act too slowly to be beneficial in this circumstance. At this point, it would be appropriate to discuss treatment options with a team of diabetes specialists [5]. However, the prolonged duration of action of these agents may increase the risk of hypoglycemia when short-term and tapering doses of glucocorticoids are administered. Shorter-acting agents, such as meglinitide, nateglinide, or repaglinide, might be suitable in this regard [30]. Glinides allow minimal dose titration and have an immediate onset of action and a short effect duration, which allows adaptation to the hyperglycemic profile of the corticosteroids and reduces the risk of hypoglycemia in the morning, coinciding with the disappearance of the hyperglycemic action of corticosteroids [2]. For patients with mild hyperglycemia who are unable or unwilling to perform injections of insulin, a trial of short-acting secretagogues such as nateglinide or repaglinide taken before meals could be considered [5]. Their major disadvantage is the requirement for multiple daily doses.
Incretin-based therapies, such as GLP-1 receptor agonists and DPP-4 inhibitors control glucose levels by stimulating insulin and inhibiting glucagon secretion in the fasting and postprandial setting. Drugs with incretin effects should probably be the drug of choice because of their immediate onset of action, their predominant effect on postprandial glycemia, and their low risk of hypoglycemia related to glucose-dependent effects [40]. A recent study found that concomitant treatment with a DPP-4 inhibitor improved various aspects of pancreatic islet-cell function in patients receiving high-dose prednisolone [41]. Furthermore, an intravenous infusion of exenatide prevented glucose intolerance induced by high doses of prednisolone in healthy patients and may be explored as a potential strategy to prevent GIDM [42].
Insulin therapy is often unavoidable when hyperglycemia is the result of the combined effects of insulin resistance induced by glucocorticoids and inhibition of the biosynthesis and release of insulin [16]. Transient corticosteroid use is one of the most common schedules of treatment, and is characterized by high initial doses and a gradual reduction as the underlying disease ameliorates. These types of glucocorticoid schedules can lead to initial moderate to severe hyperglycemia with rapid changes in glycemia in response to changes in the glucocorticoid dose. This hyperglycemia is temporary according to the duration of corticosteroid treatment. Therefore, the ideal hypoglycemic drug to address these situations should be potent, immediate-acting, and with an unlimited hypoglycemic action in order to control this rapid-onset hyperglycemia. In general, the effectiveness of the various oral hypoglycemic drugs in the treatment of new-onset glucocorticoid-induced hyperglycemia is limited [2]. This is due to their limited hypoglycemic power, which does not allow for the correction of hyperglycemia in many circumstances. Most available oral hypoglycemic drugs have a slow onset of action and/or a very limited or nonexistent ability to be titrated, leaving little capacity to adapt to major changes in the requirements of hypoglycemic action. Furthermore, the action profile of oral hypoglycemic drugs throughout the day does not usually coincide with the pattern of glucocorticoid-induced hyperglycemia. We should also note that many situations that require corticosteroids represent a formal contraindication to the use of oral hypoglycemic drugs. Patients with glycemia >200 mg/dL are frequently encountered and, in these cases, insulin is generally the drug of choice. In all other situations, insulin is usually the treatment of choice because of its efficacy and safety. It provides an immediate onset of action, an unlimited hypoglycemic power, and can be easily titrated. The different types of insulin available allow clinicians to prepare administration schedules with hypoglycemic effects appropriate for different corticosteroid schedules. The choice of the type and schedule of insulin should be determined by the previous hypoglycemic schedules of the patient and the type and schedule of corticosteroid established. The initial insulin dose and increments in insulin dosing should take into account the main variables that increase insulin resistance, which are the patient's weight and the dose of corticosteroid administered (Table 3) [3043]. The algorithm for the management of corticosteroid-induced hyperglycemia that we propose takes into account all these aspects. Basal bolus insulin therapy remains the most flexible option for patients, and includes three components: basal insulin, prandial insulin, and a supplemental correction-factor insulin [44]. Both prandial and basal insulin regimens and premixed insulin are equally effective [11]. The conventional use of long-acting basal insulin with traditional weight-based dosing may cause nocturnal hypoglycemia [31]. More studies exploring the dose titration of insulin in patients on glucocorticoids possibly utilizing technology such as continuous glucose monitoring systems are needed. In general, however, a judicious step would be to time glucocorticoid administration to a midday or an evening meal with concomitant administration of intermediate-acting insulin. Subsequently, the insulin dose can be adjusted according to capillary glycemia with increases and/or decreases of around 20%. Changes in the dosage of glucocorticoids require parallel and proportional adjustments of the insulin dose [530]. In the outpatient setting, it is essential to instruct the patient and/or the patient's family regarding how to adjust the dose of insulin according to glycemia and changes in the dose of glucocorticoids. Once insulin therapy is initiated, it is recommended to adjust the basal insulin dose daily based on the glucose pattern and total amount of correction insulin in the past 24 hours [11].
Glucocorticoids cause hyperglycemia in patients with or without pre-existing diabetes, but it remains to be determined how glucocorticoid-induced hyperglycemia in such patients should be managed and what the effects of management are. The control goals are those recommended for most patients with diabetes mellitus: preprandial glycemia <130 mg/dL, postprandial glycemia <180 mg/dL, and HbA1c <7% without hypoglycemia [2627]. Patients who are diet-controlled may require an oral hypoglycemic agent, similarly to patients at a high risk of developing GIDM. Patients who are already on an oral hypoglycemic regimen may require dose intensification, addition of an alternative agent (with preference given to sulfonylureas and up-titrating the dose to the maximum), or initiation of insulin if despite these measures, blood glucose levels persistently remain >180 mg/dL. However, there is a risk of hypoglycemia when corticosteroid doses are reduced, and this risk is very high when a nocturnal dose of corticosteroids is removed. This therapeutic strategy can also be applied in T2DM patients who are well controlled with lifestyle measures or with oral hypoglycemic drugs that exacerbate their hyperglycemia during corticosteroid treatment. In these cases, the hypoglycemic drug selected would be added to the standard therapy, always considering drugs with synergistic effects with previous treatments and accounting for contraindications [2]. On starting insulin, the dose of sulfonylureas should be reduced to prevent hypoglycemia, while other oral hypoglycemic agents can be continued [5]. In patients previously treated with insulin, the usual schedule should be modified. The increment in the usual daily insulin dose will be estimated considering the patient's body weight, the preparation, and the glucocorticoid [3043]. The calculated dose increment is added to the patient's usual total dose, distributing it in different administrations of insulin according to the usual insulin schedule and the glucocorticoid schedule [45]. Re-evaluation will need to take place daily as the effect of glucocorticoids on glycemic control is cumulative. In patients on a basal-bolus regimen (4 to 5 doses per day), it may be necessary to change the ratio from 50% basal and 50% bolus to 30% basal and 70% bolus, or to keep the same basal dose and increase the meal insulin [5]. In patients only on basal insulin with suboptimal glycemic control, the addition of rapid-acting insulin analogs with lunch and evening meals may be required [2]. For patients with persistent significant hyperglycemia with glucose levels >300 mg/dL, more aggressive insulin therapy is indicated, such as intravenous insulin infusion, a higher dose of insulin, or more frequent correction with rapid-acting insulin [46].
It should be ensured that all patients with diabetes and high-risk patients for GIDM have access to blood glucose monitoring, in order to prevent the development of hyperglycemic emergencies [5]. All patients should be educated on typical hyperglycemic symptoms that should prompt them to check their capillary blood glucose. Once the doses of glucocorticoids are being tapered down, the dosage of oral hypoglycemic agents or insulin should be appropriately reduced to prevent hypoglycemia. The appropriate follow-up of patients with previously unknown diabetes includes an HbA1c test 12 weeks following completion of glucocorticoid therapy to re-assess their diabetes status [17]. Patients on agents that can cause hypoglycemia need to check their blood glucose levels more frequently than usual 1 to 3 days after a glucocorticoid dose reduction, because it may take this amount of time for the glycemic effect of the glucocorticoid to diminish and for them to adjust their diabetes medication to the appropriate dose [47].
GIDM is a common and potentially harmful problem in clinical practice, affecting almost all medical specialties. However, its diagnosis and treatment are surprisingly undervalued by most healthcare professionals. The knowledge that hyperglycemia leads to longer hospital stays, delayed wound healing, increased infections, and higher mortality rates should encourage health-care providers to monitor its occurrence and to manage it appropriately. Similarly to T2DM in general, the principles of early detection and risk factor modification apply. Screening for GIDM should be considered in all patients (especially in those with risk factors) treated with medium to high doses of glucocorticoids. Diagnosing impaired fasting glucose or impaired glucose tolerance prior to the initiation of chronic glucocorticoids will better identify those who would benefit from glucocorticoid-sparing treatment, or if this is not an option, blood glucose monitoring while starting therapy. Together with, or after, lifestyle measures, hypoglycemic drugs with important insulin-sensitizing effects are indicated. Other oral hypoglycemic drugs or insulin therapy can be considered to be the drug of choice. Treatment, in most cases with insulin, should take into account the degree and pattern of hyperglycemia and the type, dose, and schedule of glucocorticoid used. Treatment should then be adjusted based on capillary glycemia and on changes in the dose of glucocorticoids. Moreover, it is essential to instruct the patient and/or the patient's family about how to perform these adjustments. Further investigation into the precise mechanism of glucocorticoid-induced insulin resistance will provide insights for future diabetes prevention efforts and targeted therapies.
Figures and Tables
Table 1
Risk Factors for Glucocorticoid-Induced Diabetes Mellitus

Table 2
Mechanisms of Glucocorticoid-Induced Diabetes Mellitus

References
1. Fathallah N, Slim R, Larif S, Hmouda H, BenSalem C. Drug-induced hyperglycaemia and diabetes. Drug Saf. 2015; 38:1153–1168.
2. Perez A, Jansen-Chaparro S, Saigi I, Bernal-Lopez MR, Minambres I, Gomez-Huelgas R. Glucocorticoid-induced hyperglycemia. J Diabetes. 2014; 6:9–20.
3. Hwang JL, Weiss RE. Steroid-induced diabetes: a clinical and molecular approach to understanding and treatment. Diabetes Metab Res Rev. 2014; 30:96–102.
4. Conn JW, Fajans SS. Influence of adrenal cortical steroids on carbohydrate metabolism in man. Metabolism. 1956; 5:114–127.
5. Mills E, Devendra S. Steroid-induced hyperglycaemia in primary care. London J Prim Care (Abingdon). 2015; 7:103–106.
6. Blackburn D, Hux J, Mamdani M. Quantification of the risk of corticosteroid-induced diabetes mellitus among the elderly. J Gen Intern Med. 2002; 17:717–720.
7. Donihi AC, Raval D, Saul M, Korytkowski MT, DeVita MA. Prevalence and predictors of corticosteroid-related hyperglycemia in hospitalized patients. Endocr Pract. 2006; 12:358–362.
8. Kasiske BL, Snyder JJ, Gilbertson D, Matas AJ. Diabetes mellitus after kidney transplantation in the United States. Am J Transplant. 2003; 3:178–185.
9. Kim SY, Yoo CG, Lee CT, Chung HS, Kim YW, Han SK, et al. Incidence and risk factors of steroid-induced diabetes in patients with respiratory disease. J Korean Med Sci. 2011; 26:264–267.
10. Gulliford MC, Charlton J, Latinovic R. Risk of diabetes associated with prescribed glucocorticoids in a large population. Diabetes Care. 2006; 29:2728–2729.
11. Kwon S, Hermayer KL. Glucocorticoid-induced hyperglycemia. Am J Med Sci. 2013; 345:274–277.
12. Panthakalam S, Bhatnagar D, Klimiuk P. The prevalence and management of hyperglycaemia in patients with rheumatoid arthritis on corticosteroid therapy. Scott Med J. 2004; 49:139–141.
13. Liu XX, Zhu XM, Miao Q, Ye HY, Zhang ZY, Li YM. Hyperglycemia induced by glucocorticoids in nondiabetic patients: a meta-analysis. Ann Nutr Metab. 2014; 65:324–332.
14. Gurwitz JH, Bohn RL, Glynn RJ, Monane M, Mogun H, Avorn J. Glucocorticoids and the risk for initiation of hypoglycemic therapy. Arch Intern Med. 1994; 154:97–101.
15. Katsuyama T, Sada KE, Namba S, Watanabe H, Katsuyama E, Yamanari T, et al. Risk factors for the development of glucocorticoid-induced diabetes mellitus. Diabetes Res Clin Pract. 2015; 108:273–279.
16. Geer EB, Islam J, Buettner C. Mechanisms of glucocorticoid-induced insulin resistance: focus on adipose tissue function and lipid metabolism. Endocrinol Metab Clin North Am. 2014; 43:75–102.
17. Brady VJ, Grimes D, Armstrong T, LoBiondo-Wood G. Management of steroid-induced hyperglycemia in hospitalized patients with cancer: a review. Oncol Nurs Forum. 2014; 41:E355–E365.
18. Pagano G, Cavallo-Perin P, Cassader M, Bruno A, Ozzello A, Masciola P, et al. An in vivo and in vitro study of the mechanism of prednisone-induced insulin resistance in healthy subjects. J Clin Invest. 1983; 72:1814–1820.
19. van Raalte DH, Ouwens DM, Diamant M. Novel insights into glucocorticoid-mediated diabetogenic effects: towards expansion of therapeutic options? Eur J Clin Invest. 2009; 39:81–93.
20. Sakoda H, Ogihara T, Anai M, Funaki M, Inukai K, Katagiri H, et al. Dexamethasone-induced insulin resistance in 3T3-L1 adipocytes is due to inhibition of glucose transport rather than insulin signal transduction. Diabetes. 2000; 49:1700–1708.
21. Weinstein SP, Wilson CM, Pritsker A, Cushman SW. Dexamethasone inhibits insulin-stimulated recruitment of GLUT4 to the cell surface in rat skeletal muscle. Metabolism. 1998; 47:3–6.
22. Vegiopoulos A, Herzig S. Glucocorticoids, metabolism and metabolic diseases. Mol Cell Endocrinol. 2007; 275:43–61.
23. Boden G, Shulman GI. Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and beta-cell dysfunction. Eur J Clin Invest. 2002; 32:Suppl 3. 14–23.
24. Delaunay F, Khan A, Cintra A, Davani B, Ling ZC, Andersson A, et al. Pancreatic beta cells are important targets for the diabetogenic effects of glucocorticoids. J Clin Invest. 1997; 100:2094–2098.
25. van Raalte DH, Nofrate V, Bunck MC, van Iersel T, Elassaiss Schaap J, Nassander UK, et al. Acute and 2-week exposure to prednisolone impair different aspects of beta-cell function in healthy men. Eur J Endocrinol. 2010; 162:729–735.
26. American Diabetes Association. 14. Diabetes care in the hospital. Diabetes Care. 2017; 40:Suppl 1. S120–S127.
27. Umpierrez GE, Hellman R, Korytkowski MT, Kosiborod M, Maynard GA, Montori VM, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012; 97:16–38.
28. Baldwin D, Apel J. Management of hyperglycemia in hospitalized patients with renal insufficiency or steroid-induced diabetes. Curr Diab Rep. 2013; 13:114–120.
29. American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017; 40:Suppl 1. S11–S24.
30. Clore JN, Thurby-Hay L. Glucocorticoid-induced hyperglycemia. Endocr Pract. 2009; 15:469–474.
31. Burt MG, Roberts GW, Aguilar-Loza NR, Frith P, Stranks SN. Continuous monitoring of circadian glycemic patterns in patients receiving prednisolone for COPD. J Clin Endocrinol Metab. 2011; 96:1789–1796.
32. Valderhaug TG, Jenssen T, Hartmann A, Midtvedt K, Holdaas H, Reisaeter AV, et al. Fasting plasma glucose and glycosylated hemoglobin in the screening for diabetes mellitus after renal transplantation. Transplantation. 2009; 88:429–434.
33. Imatoh T, Sai K, Hori K, Segawa K, Kawakami J, Kimura M, et al. Development of a novel algorithm for detecting glucocorticoid-induced diabetes mellitus using a medical information database. J Clin Pharm Ther. 2017; 42:215–220.
34. Gonzalez-Gonzalez JG, Mireles-Zavala LG, Rodriguez-Gutierrez R, Gomez-Almaguer D, Lavalle-Gonzalez FJ, Tamez-Perez HE, et al. Hyperglycemia related to high-dose glucocorticoid use in noncritically ill patients. Diabetol Metab Syndr. 2013; 5:18.
35. Suh S, Kim JH. Glycemic variability: how do we measure it and why is it important? Diabetes Metab J. 2015; 39:273–282.
36. Seelig E, Meyer S, Timper K, Nigro N, Bally M, Pernicova I, et al. Metformin prevents metabolic side effects during systemic glucocorticoid treatment. Eur J Endocrinol. 2017; 176:349–358.
37. Willi SM, Kennedy A, Brant BP, Wallace P, Rogers NL, Garvey WT. Effective use of thiazolidinediones for the treatment of glucocorticoid-induced diabetes. Diabetes Res Clin Pract. 2002; 58:87–96.
38. Luther P, Baldwin D Jr. Pioglitazone in the management of diabetes mellitus after transplantation. Am J Transplant. 2004; 4:2135–2138.
39. Vu K, Busaidy N, Cabanillas ME, Konopleva M, Faderl S, Thomas DA, et al. A randomized controlled trial of an intensive insulin regimen in patients with hyperglycemic acute lymphoblastic leukemia. Clin Lymphoma Myeloma Leuk. 2012; 12:355–362.
40. Yanai H, Masui Y, Yoshikawa R, Kunimatsu J, Kaneko H. Dipeptidyl peptidase-4 inhibitor for steroid-induced diabetes. World J Diabetes. 2010; 1:99–100.
41. van Genugten RE, van Raalte DH, Muskiet MH, Heymans MW, Pouwels PJ, Ouwens DM, et al. Does dipeptidyl peptidase-4 inhibition prevent the diabetogenic effects of glucocorticoids in men with the metabolic syndrome? A randomized controlled trial. Eur J Endocrinol. 2014; 170:429–439.
42. van Raalte DH, van Genugten RE, Linssen MM, Ouwens DM, Diamant M. Glucagon-like peptide-1 receptor agonist treatment prevents glucocorticoid-induced glucose intolerance and islet-cell dysfunction in humans. Diabetes Care. 2011; 34:412–417.
43. Saigi I, Perez A. Management of glucocorticoid induced hyperglycemia. Rev Clin Esp. 2010; 210:397–403.
44. Burt MG, Drake SM, Aguilar-Loza NR, Esterman A, Stranks SN, Roberts GW. Efficacy of a basal bolus insulin protocol to treat prednisolone-induced hyperglycaemia in hospitalised patients. Intern Med J. 2015; 45:261–266.
45. Grommesh B, Lausch MJ, Vannelli AJ, Mullen DM, Bergenstal RM, Richter SA, et al. Hospital insulin protocol aims for glucose control in glucocorticoid-induced hyperglycemia. Endocr Pract. 2016; 22:180–189.
46. Hawkins K, Donihi AC, Korytkowski MT. Glycemic management in medical and surgical patients in the non-ICU setting. Curr Diab Rep. 2013; 13:96–106.
47. Lansang MC, Hustak LK. Glucocorticoid-induced diabetes and adrenal suppression: how to detect and manage them. Cleve Clin J Med. 2011; 78:748–756.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download