Abstract
Background
Dipeptidyl peptidase 4/CD26 (DPP-4) is a widely expressed cell surface serine protease. DPP-4 inhibitors, one of common anti-diabetic agents play a protective role in bone metabolism in recent studies. A soluble form of DPP-4 is found in serum, and exhibits DPP-4 enzymatic activity. However, the physiological role of serum or soluble DPP-4 and its relationship with DPP-4 enzymatic function remain poorly understood. The aims of current study were to determine the association between serum DPP-4 activity and bone mineral density (BMD) in postmenopausal women.
Methods
We recruited data and serum samples from 124 consecutive healthy postmenopausal women aged >50 years. We divided study subjects into obese (body mass index [BMI] ≥25 kg/m2) and non-obese (BMI <25 kg/m2) postmenopausal women and examined the correlation between serum DPP-4 activity and clinical variables in each groups.
Results
A total of 124 postmenopausal women was enrolled, with a mean age of 59.9±7.1 years. The mean BMI of the study patients was 24.4±2.8 kg/m2. Regarding bone turnover markers, serum DPP-4 activity was positively correlated with serum calcium concentrations, intact parathyroid hormone, and serum C-telopeptide levels in all of the study subjects. However, there was no association between serum DPP-4 activity and BMD in the spine or femoral neck in all of the study subjects. Serum DPP-4 activity was negatively correlated (R=−0.288, P=0.038) with BMD of the spine in obese postmenopausal women.
Osteoporosis is a common disease in postmenopausal women and elderly people. Osteoporotic fractures are associated with disability, high healthcare costs, and an increased risk of morbidity and mortality. However, the appropriate medical treatment for osteoporosis improves patient survival and reduces fractures [1].
Dipeptidyl peptidase 4/CD26 (DPP-4) is a widely expressed cell surface serine protease that cleaves the N-terminal dipeptide from peptide substrates that contain proline or alanine in the second position. Both membrane-anchored and soluble forms of the enzyme can perform this cleavage reaction [234]. In recent years, studies of DPP-4 enzymatic activity have mainly focused on the metabolic effects linked to glucagon-like peptide-1 (GLP-1) degradation [5], because DPP-4 inhibitors are commonly used as anti-diabetic agents to improve hyperglycemia in patients with type 2 diabetes.
Recent studies have also suggested that DPP-4 inhibitors play a protective role in bone metabolism [6]. For example, in diabetic rat models, sitagliptin treatment decreased the serum levels of a resorption marker and attenuated trabecular bone loss [7]. In a meta-analysis of 28 trials that included 11,880 and 9,175 patients receiving DPP-4 inhibitors and comparative agents, respectively, for a duration of at least 24 weeks, treatment with DPP-4 inhibitors was associated with a reduced risk of bone fractures compared to placebo or active drugs [8]. In another study, treatment with GLP-2 for 4 months in postmenopausal women resulted in increased bone mineral density (BMD) in the hip in a randomized clinical study [9]. Taken together, the above studies suggest that DPP-4 inhibitors might increase endogenous GLP-1 and GLP-2 expression, thereby decreasing osteoporotic fractures.
A soluble form of DPP-4 is found in serum, and exhibits DPP-4 enzymatic activity [101112]. However, the physiological role of serum or soluble DPP-4 and its relationship with DPP-4 enzymatic function remain poorly understood because the mechanisms by which DPP-4 are produced and secreted remain unclear [13]. In the previous study, DPP-4 was known as a novel adipokine showing that the DPP-4 released from adipose tissue correlates with adipocyte size which was linking obesity [14]. There are currently no data regarding serum DPP-4 activity and BMD in humans. Therefore, we designed the current study to elucidate the association between serum DPP-4 activity and BMD in postmenopausal women and we made a subgroup analysis into obese and non-obese group in postmenopausal women because obesity was associated with DPP-4 activity and BMD.
We recruited data and serum samples from 124 consecutive healthy postmenopausal women aged >50 years as part of a subset of a study performed from June 2009 to October 2010 at Kangwon National University Hospital, South Korea [15]. Menopause was defined as the absence of menstruation for at least 1 year. Women who had been taking glucocorticoids and estrogen for more than 3 months, and had diseases that could affect bone metabolism such as Graves disease or Cushing syndrome, or conditions such as diabetes mellitus were excluded from the study. Hysterectomized and premenopausal bilaterally ovariectomized women were also excluded.
A self-administered questionnaire, interviews, and anthropometric measurements were used to collect data regarding lifestyle, physical activity, and previous medical and fracture histories. Previous fragility fractures were defined as low-trauma fractures involving the femur, spine, and other sites such as the wrist, ankle, foot, and ribs.
Areal BMD (g/cm2) values were determined in the spine, right femoral neck, and total hip in all of the subjects using a Lunar Prodigy Vision dual-emission X-ray absorptiometry system (Lunar Corp., Madison, WI, USA). According to the World Health Organization definition, osteoporosis was determined as a T-score ≤−2.5 standard deviations (SDs) at any site. One investigator performed the densitometry tests and analyses in all of the subjects. The precision of the equipment, presented as the coefficient of variation, was 0.90% and 1.14% for the lumbar spine and femoral neck, respectively, in 20 volunteers at Kangwon National University who were not enrolled in the study.
Serum DPP-4 activity was measured using a human DPP-4/CD26 immunoassay kit (R&D Systems, Minneapolis, MN, USA). The serum levels of C-terminal telopeptide of type I collagen (C-telopeptide), and intact parathyroid hormone (PTH) were measured by Molecular Analytics (Roche, Mannheim, Germany). The serum levels of osteocalcin and 25-(OH) vitamin D3 were measured using a Y-counter (Packard, Meriden, CT, USA). We examined the association between serum DPP-4 activity and BMD in obese and non-obese groups.
The Institutional Review Board of Kangwon National University Hospital approved the study protocol (IRB number 09–07). Written informed consent was obtained from each individual.
Pearson correlation coefficients were calculated to analyze the relationship between serum DPP-4 levels and clinical parameters, including BMD. Student t tests or chi-square tests were used to compare the baseline characteristics between obese and non-obese menopausal women. Serum DPP-4 activity was normally distributed variable. Statistical analyses were performed using SPSS version 21.0 (IBM Co., Armonk, NY, USA). All P values were two-tailed, and P<0.05 was considered statistically significant.
A total of 124 postmenopausal women were enrolled, with a mean age of 59.9±7.1 years. The mean body mass index (BMI) of the study patients was 24.4±2.8 kg/m2, and the mean age at menopause was 50.8±3.6 years. Table 1 shows the baseline clinical characteristics of study subjects. Obese patients have a higher blood pressure and higher BMD of spine and total hip compared to non-obese patients (Table 1).
Serum DPP-4 activity was negatively correlated with age and systolic blood pressure and serum DPP-4 activity was positively correlated with corrected calcium, C-telopeptide and intact PTH in the whole study population (Table 2). However, there was no association between serum DPP-4 activity and BMD in the spine or femoral neck in all of the study subjects. We divided study subjects into obese (BMI ≥25 kg/m2) and non-obese (BMI <25 kg/m2) postmenopausal women.
In the non-obese group, there was positive correlation between serum DPP-4 activity and corrected calcium (R=0.316, P=0.007) or C-telopeptide (R=0.284, P=0.016) but there was no correlation between serum DPP-4 activity and BMD of spine or femoral neck (Table 3).
Table 4 shows the correlation between serum DPP-4 activity and clinical variables in obese patients (n=52). In Serum DPP-4 activity was negatively correlated with systolic and diastolic BP in obese subjects. Serum DPP-4 activity was also negatively correlated (R=−0.288, P=0.038) with BMD in the spine (Fig. 1).
Regarding bone turnover markers, serum DPP-4 activity was positively correlated with serum calcium concentrations, intact PTH, and serum C-telopeptide levels in all of the study subjects (Table 2). There was also a positive correlation between serum DPP-4 activity and serum C-telopeptide levels in non-obese subjects (R=0.284, P=0.016, n=76) (Table 3). However, there was no correlation between serum DPP-4 activity and bone turnover markers such as C-telopeptide or osteocalcin in the obese subjects (Table 4).
The current study demonstrated for the first time that serum soluble DPP-4 activity was negatively correlated with spine BMD in obese postmenopausal women. However, there was no significant association between serum DPP-4 activity and BMD in non-obese postmenopausal women. It is unclear why serum DPP-4 activity was only associated with BMD in obese postmenopausal women.
DPP-4 substrates are proline- or alanine-containing peptides including chemokines, neuropeptides, and vasoactive peptides such as interleukin 2 (IL-2), IL-1β, and GLP-1 [16]. It is widely distributed in the placenta, kidney, liver, intestine, brain, lymphocytes, endothelial cells, and lungs [31617]. DDP-4 enzyme activity regulates the postprandial availability of different gut hormones that might affect bone metabolism, including GLP-1, GLP-2, glucose-dependent insulinotropic peptide, and peptide YY [18]. Therefore, additional beneficial effects on bone health could be achieved using DPP-4 inhibitors compared to those achieved using GLP-1 receptor agonists [18]. Therefore, the current study suggests that the activity of serum soluble DPP-4 might influence a variety of gut hormones that regulate bone metabolism in obese postmenopausal women.
Several studies have revealed a positive relationship between DPP-4 inhibitors and bone metabolism [678]. However, another study showed that the use of DPP-4 inhibitors was not associated with fracture risk [19]. In addition, the DPP-4 inhibitor MK-0626 showed neutral effects on the bone in diabetic muscle-lysine-arginine (MKR) mice or during osteoblast differentiation [20].
The current study showed that serum DPP-4 activity was positively correlated with serum C-telopeptide levels in non-obese subjects (n=76) and the entire study population (n=124), suggesting that there is a possible correlation between serum DPP-4 activity and bone resorption markers. Interestingly, serum DPP-4 levels were correlated with serum intact PTH levels and corrected calcium levels in all of the study subjects, but not in the obese group. Interestingly, previous reports have demonstrated that PTH is a DPP-4 inhibitor [2122]. Our study showed no association between DPP-4 and osteocalcin such as bone formation marker but recent study demonstrated that increased plasma DPP-4 activity was positively associated with C-telopeptide and osteocalcin and negatively with active GLP-1 and BMD [23].
Nevertheless, further studies with a sufficient sample size in the obese group are needed to clarify the association between serum DPP-4 activity and serum C-telopeptide concentrations or intact PTH levels.
Recently, Nishida et al. [23] demonstrated that blocking DPP-4 signaling inhibits the development of human osteoclasts, suggesting that there is an association between DPP-4 and bone resorption. Zheng T et al. also showed that postmenopausal women with the highest quartile of DPP-4 activity showed lower BMD compared with whose in the lowest quartile [24]. Another study showed that Dpp4–/– ovarectomized female mice exhibited reductions in femoral geometry and femoral structural properties [25]. However, another study showed that treatment with vildagliptin (100 mg daily) for 1 year did not change postprandial serum C-telopeptide levels in a single center, double blinded randomized clinical trial of 59 patients with drug-naïve type 2 diabetes [26].
In the recent years, DPP-4 activity was regarded as a new adipokine highly expressed and released from adipocytes and DPP-4 concentrations are higher in obese subjects suggesting the linking between type 2 diabetes and atherosclerosis [14]. However, our study demonstrated there was no significantly difference of the DPP-4 activity between obese and non-obese postmenopausal women and we showed the inverse association between DPP-4 activity and BMD of spine only in obese postmenopausal women. Further study with larger study population is need to clarify above discrepancies.
One of the limitations of this study is that it is not population-based, and is a single center study with a small sample size. Second, it is a cross-sectional study that failed to identify a causal relationship between serum DPP-4 activity and BMD. Third, the study subjects are postmenopausal women, and we did not clarify the interaction between serum DPP-4 activity and estrogen levels (menopausal status). Additional prospective studies are needed with a larger sample size to obtain sufficient statistical power to demonstrate the association between DPP-4 activity and bone metabolism.
In conclusion, we demonstrated that serum DPP-4 activity was negatively associated with BMD of the spine in obese postmenopausal women. These findings have implications for increasing our understanding of serum soluble DPP-4 activity on bone metabolism, and give clues for future prospective studies to help clarify causality of DPP-4 activity and advance this area of research.
Figures and Tables
Fig. 1
Correlation analysis showing the association between bone mineral density and serum dipeptidyl peptidase 4/CD26 (DPP-4) activity levels in obese postmenopausal women (n=52). BMD, bone mineral density.
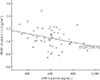
Table 1
Baseline Clinical Characteristics of the Study Subjects (n=124)

Table 2
Correlation between Serum DPP-4 Activity and Other Variables in the Whole Study Population (n=124)
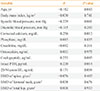
Table 3
Correlation between Serum DPP-4 Activity and Other Variables in Non-Obese Subjects (n=72)
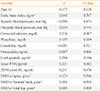
Table 4
Correlation between Serum DPP-4 Activity and Other Variables in Obese Subjects (n=52)

ACKNOWLEDGMENTS
This study was supported by research grant from Gangwon branch of Korean Endocrine Society and Korean Diabetes Association and by 2013 Research Grant from Kangwon National University (120131863).
References
1. Sattui SE, Saag KG. Fracture mortality: associations with epidemiology and osteoporosis treatment. Nat Rev Endocrinol. 2014; 10:592–602.
2. de Meester I, Lambeir AM, Proost P, Scharpe S. Dipeptidyl peptidase IV substrates. An update on in vitro peptide hydrolysis by human DPPIV. Adv Exp Med Biol. 2003; 524:3–17.
3. Lambeir AM, Durinx C, Scharpe S, De Meester I. Dipeptidyl-peptidase IV from bench to bedside: an update on structural properties, functions, and clinical aspects of the enzyme DPP IV. Crit Rev Clin Lab Sci. 2003; 40:209–294.
4. Polgar L, Szabo E. Prolyl endopeptidase and dipeptidyl peptidase IV are distantly related members of the same family of serine proteases. Biol Chem Hoppe Seyler. 1992; 373:361–366.
5. Pala L, Rotella CM. The role of DPP4 activity in cardiovascular districts: in vivo and in vitro evidence. J Diabetes Res. 2013; 2013:590456.
6. Dicembrini I, Mannucci E, Rotella CM. Bone: incretin hormones perceiver or receiver? Exp Diabetes Res. 2012; 2012:519784.
7. Glorie L, Behets GJ, Baerts L, De Meester I, D'Haese PC, Verhulst A. DPP IV inhibitor treatment attenuates bone loss and improves mechanical bone strength in male diabetic rats. Am J Physiol Endocrinol Metab. 2014; 307:E447–E455.
8. Monami M, Dicembrini I, Antenore A, Mannucci E. Dipeptidyl peptidase-4 inhibitors and bone fractures: a meta-analysis of randomized clinical trials. Diabetes Care. 2011; 34:2474–2476.
9. Henriksen DB, Alexandersen P, Hartmann B, Adrian CL, Byrjalsen I, Bone HG, et al. Four-month treatment with GLP-2 significantly increases hip BMD: a randomized, placebo-controlled, dose-ranging study in postmenopausal women with low BMD. Bone. 2009; 45:833–842.
10. Durinx C, Lambeir AM, Bosmans E, Falmagne JB, Berghmans R, Haemers A, et al. Molecular characterization of dipeptidyl peptidase activity in serum: soluble CD26/dipeptidyl peptidase IV is responsible for the release of X-Pro dipeptides. Eur J Biochem. 2000; 267:5608–5613.
11. Lee SA, Kim YR, Yang EJ, Kwon EJ, Kim SH, Kang SH, et al. CD26/DPP4 levels in peripheral blood and T cells in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2013; 98:2553–2561.
12. Iwaki-Egawa S, Watanabe Y, Kikuya Y, Fujimoto Y. Dipeptidyl peptidase IV from human serum: purification, characterization, and N-terminal amino acid sequence. J Biochem. 1998; 124:428–433.
13. Cordero OJ, Salgado FJ, Nogueira M. On the origin of serum CD26 and its altered concentration in cancer patients. Cancer Immunol Immunother. 2009; 58:1723–1747.
14. Lamers D, Famulla S, Wronkowitz N, Hartwig S, Lehr S, Ouwens DM, et al. Dipeptidyl peptidase 4 is a novel adipokine potentially linking obesity to the metabolic syndrome. Diabetes. 2011; 60:1917–1925.
15. Cho EH, Cho KH, Lee HA, Kim SW. High serum osteopontin levels are associated with low bone mineral density in postmenopausal women. J Korean Med Sci. 2013; 28:1496–1499.
16. Drucker DJ. Dipeptidyl peptidase-4 inhibition and the treatment of type 2 diabetes: preclinical biology and mechanisms of action. Diabetes Care. 2007; 30:1335–1343.
17. Abbott CA, Baker E, Sutherland GR, McCaughan GW. Genomic organization, exact localization, and tissue expression of the human CD26 (dipeptidyl peptidase IV) gene. Immunogenetics. 1994; 40:331–338.
18. Walsh JS, Henriksen DB. Feeding and bone. Arch Biochem Biophys. 2010; 503:11–19.
19. Driessen JH, van Onzenoort HA, Henry RM, Lalmohamed A, van den Bergh JP, Neef C, et al. Use of dipeptidyl peptidase-4 inhibitors for type 2 diabetes mellitus and risk of fracture. Bone. 2014; 68:124–130.
20. Gallagher EJ, Sun H, Kornhauser C, Tobin-Hess A, Epstein S, Yakar S, et al. The effect of dipeptidyl peptidase-IV inhibition on bone in a mouse model of type 2 diabetes. Diabetes Metab Res Rev. 2014; 30:191–200.
21. Huber BC, Brunner S, Segeth A, Nathan P, Fischer R, Zaruba MM, et al. Parathyroid hormone is a DPP-IV inhibitor and increases SDF-1-driven homing of CXCR4(+) stem cells into the ischaemic heart. Cardiovasc Res. 2011; 90:529–537.
22. Grabmaier U, Brandl L, Kreiner J, Negele T, Huber BC, Rimmbach C, et al. Increased numbers of bone marrow-derived cells in parathyroid adenoma. Eur J Clin Invest. 2014; 44:833–839.
23. Nishida H, Suzuki H, Madokoro H, Hayashi M, Morimoto C, Sakamoto M, et al. Blockade of CD26 signaling inhibits human osteoclast development. J Bone Miner Res. 2014; 29:2439–2455.
24. Zheng T, Yang L, Liu Y, Liu H, Yu J, Zhang X, et al. Plasma DPP4 activities are associated with osteoporosis in postmenopausal women with normal glucose tolerance. J Clin Endocrinol Metab. 2015; 100:3862–3870.
25. Kyle KA, Willett TL, Baggio LL, Drucker DJ, Grynpas MD. Differential effects of PPAR-{gamma} activation versus chemical or genetic reduction of DPP-4 activity on bone quality in mice. Endocrinology. 2011; 152:457–467.
26. Bunck MC, Poelma M, Eekhoff EM, Schweizer A, Heine RJ, Nijpels G, et al. Effects of vildagliptin on postprandial markers of bone resorption and calcium homeostasis in recently diagnosed, well-controlled type 2 diabetes patients. J Diabetes. 2012; 4:181–185.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download