Abstract
Subclinical hypothyroidism (SCH) is a common disorder that is characterized by elevated thyroid-stimulating hormone levels in conjunction with free thyroxine concentrations within the normal reference range. Thyroid hormones are known to affect the heart and vasculature and, as a result, the impact of SCH on the cardiovascular (CV) system has recently become an important topic of research. Strong evidence points to a link between SCH and CV risk factors such as alterations in blood pressure, lipid levels, and atherosclerosis. Additionally, accumulating evidence indicates that SCH is associated with metabolic syndrome and heart failure. The present review proposes that SCH may be a potentially modifiable risk factor of CV disease and mortality. However, large-scale clinical trials with appropriate power investigating the risks and benefits of SCH treatment are required to determine whether these benefits can be achieved with levothyroxine therapy.
Subclinical hypothyroidism (SCH), which is defined as an isolated elevation of thyroid-stimulating hormone (TSH) levels with a normal free thyroxine (fT4) level, is a relatively common disorder. Most experts agree that SCH represents early, mild thyroid failure [1] and this issue is becoming increasingly recognized because the performance of thyroid function tests have substantially increased in primary care settings [2]. Despite the intuitive appeal of the relationship between elevated TSH levels or SCH and adverse cardiovascular (CV) outcomes, it remains unclear whether variations in thyroid hormone levels within the normal range are also associated with mortality endpoints [3]. The precise definition and clinical significance of SCH are also confounded by controversies regarding the correct upper limit of the reference range for serum TSH. In fact, the optimal TSH cutoff values and clinical significance of these subclinical abnormalities are even more controversial [4]. Typically, the treatment of SCH is considered only for patients who are pregnant, infertile, exhibit associated symptoms, or have a high risk of progression to overt hypothyroidism [3]. Although there is a high prevalence of SCH, the evidence supporting screening for this disorder and the benefits and risks of its treatment remain controversial. Therefore, the primary goals of the present narrative review were to assess current evidence regarding the clinical aspects of SCH and cardiovascular disease (CVD) and to evaluate the mechanisms that are likely to underlie this relationship. To accomplish these goals, an updated search of PubMed was conducted for the most recent articles investigating the risks and treatment of SCH that were published prior to 2015.
SCH has various causes of which the most common (60% to 80%) is chronic autoimmune thyroiditis associated with the presence of anti-thyroid peroxidase antibodies, which is a marker of chronic lymphocytic (Hashimoto's) thyroiditis [4]. Hashimoto's thyroiditis is more common in girls and women, but the overall incidence increases with age in both sexes [1]. Patients who have been treated for overt thyroid failure often exhibit SCH due to inadequate thyroid hormone supplementation, poor adherence to the treatment regimen, drug interactions, or the inadequate monitoring of treatment [1]. The prevalence of SCH varies according to population, age, sex, race, region, and method of TSH measurement [1]. Thus, it is necessary that the normal reference range for TSH levels be standardized and that appropriate quality control procedures be established by each laboratory investigating this phenomenon [3]. In general, SCH is defined as a TSH level greater than 4.0 to 6.0 mIU/L [5]. The prevalence of SCH is relatively high and ranges from 4% to 20% in the adult population with women, elderly people, and iodine-sufficient populations being affected more often [6]. For example, in a recent study using Korean population-based cohorts, the prevalence of SCH was reported to be 11.3% [7].
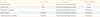
The adverse clinical effects associated with overt thyroid disorders are well known and, given the multiple actions of thyroid hormones on the heart, vessels, bones, and brain, long-term adverse outcomes may manifest as subclinical levels of dysfunction. Table 1 provides an overview of the findings from studies investigating the associations of SCH with various clinical conditions.
For example, the relationship between pathological thyroid dysfunction and body weight is well established [89]. Cross-sectional studies using population cohorts have demonstrated that variations in thyroid function within the population reference range have a substantial impact on weight and body mass index (BMI). Higher levels of TSH are associated with an increased BMI [8] and rising TSH levels which, in turn, are associated with enhanced weight gain [9].
Additionally, an increasing amount of evidence indicates that higher levels of TSH are associated with worsening blood pressure (BP) and altered lipid levels. A cross-sectional study demonstrated that subjects with SCH exhibit increased BP [10] and a population-based study observed positive linear associations between TSH levels and systolic and diastolic BP [11]. Similarly, a recent meta-analysis found that SCH is associated with higher systolic BP [12]. Thyroid hormones exert multiple effects on the regulation, absorption, and metabolism of lipid synthesis as well. Previous studies have consistently demonstrated that elevated levels of serum total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), apolipoprotein B, lipoprotein(a), and possibly triglycerides (TG) are reversed in individuals with overt hypothyroidism following levothyroxine (T4) therapy [13]. A number of studies have reported significant increases in serum TC, LDL-C, and TG in patients with SCH [13] and the findings of a meta-analysis found that the TC, LDL-C, and TG levels of SCH subjects are significantly increased relative to euthyroid individuals [14].
Similarly, a Korean study demonstrated that SCH subjects with an intermediate-to-high risk of CVD had higher coronary calcium scores than euthyroid subjects [15] and Marfella et al. [16] identified enhanced inflammatory activity in the asymptomatic carotid plaques of SCH subjects compared to euthyroid subjects. SCH can also lead to vascular problems characterized by increased vascular stiffness and endothelial dysfunction [17]. Studies of euthyroid individuals have shown that fT4 and triiodothyronine (T3) levels, even within the normal range, are inversely associated with the presence and severity of coronary and carotid atherosclerosis as well as carotid artery intima media thickness [18]. Other possible explanations for the increased CV risk in persons with SCH include hypercoagulability, insulin resistance, oxidative stress [4], and endothelial dysfunction [17].
Metabolic syndrome (MetS) is a condition characterized by a cluster of metabolic disorders including abdominal obesity, insulin resistance/glucose intolerance, dyslipidemia, and hypertension [19]. It has been well documented that MetS is associated with increased risks of all-cause mortality and CVD [19]. A systemic review by Iwen et al. [20] found convincing evidence supporting the major impact of SCH on all components of MetS and a cross-sectional analysis of cohort studies highlighted the fact that the odds of having MetS are positively associated with TSH levels within the reference range [9]. Additionally, cross-sectional and longitudinal follow-up studies from Japan observed strong associations between SCH and MetS [21]. In Korea, high normal TSH levels were significantly associated with the increased prevalence of MetS in 7,270 euthyroid men and women [22] and another study of 2,760 young Korean female volunteers with normal TSH levels found that the high TSH group had a 2-fold greater risk of MetS than subjects in the low TSH group [23].
It is well known that thyroid hormones act on the heart and vasculature and, as a result, the impact of subclinical thyroid dysfunction on the CV system has recently become an important topic of research. SCH can lead to impaired systolic and diastolic cardiac function [24] and symptomatic SCH patients often complain of reduced exercise tolerance during effort [25]. This same study found that a slowed rate of left ventricular relaxation might critically impair ventricular filling during exercise and result in left ventricular systolic dysfunction. Older people with SCH and a high CV risk appear to be at an increased risk of incident heart failure [26] and SCH was found to affect left ventricular dysfunction, although this abnormality may be reversed by T4 substitutive therapy [27]. Likewise, a recent cardiac magnetic resonance spectroscopic study demonstrated that early cardiac bio-energetic impairments in SCH patients are reversible with T4 therapy [28]. A pooled analysis from six prospective cohorts also found that the risk of heart failure events increases in conjunction with higher TSH levels [29].
Many studies have examined the relationship between SCH and CVD. Studies of euthyroid individuals observed a positive association between TSH levels and mortality due to coronary heart disease (CHD) [1130]. TSH levels within the normal range are inversely associated with all-cause mortality [313233] and adult Taiwanese subjects with SCH were shown to have an increased risk for all-cause mortality and CVD death over a 10-year period [34]. However, other studies did not find any associations with all-cause [35363738] or CV [313639] mortality rates. These discrepant findings may be due to differences in sample size and power, the inconsistent age and sex ratios of the study populations, or the varied iodine intakes of different regions. Two meta-analyses [4041] investigating this matter demonstrated that SCH may be associated with a modest increase in the risks of CHD and mortality, particularly in subjects with higher TSH levels. A more recent review of the clinical consequences of variations in thyroid function within the normal reference range found that even modest elevations of TSH may have substantial health outcomes, including CV mortality [9]. In a Korean cohort that was followed for 10 years, elevated serum TSH levels significantly increased the risk of CVD by approximately 20% per one standard deviation in males [7]. More recently, fT4 and fT3 levels within the normal range were inversely associated with the risks of all-cause and cancer mortality in a Korean cohort of euthyroid men and women (n=212,456) [42].
A number of placebo-controlled studies have assessed the effects of T4 replacement therapy on the symptoms of patients with SCH. However, the reported benefits of various SCH treatments are limited and evidence regarding the association of SCH with CVD remains controversial [43]. An intervention study of 56 women with SCH identified elevated systolic and diastolic BP and increased serum cholesterol and homocysteine levels compared to healthy controls [44]; these factors were normalized after 18 months of T4 therapy. A systematic review of 13 heterogeneous studies concluded that T4 treatment leads to a reduction in serum TC and LDL-C levels in patients with SCH [45]; this finding has been confirmed in subsequent randomized controlled trials (RCTs) [17]. However, to date, clinical trials have not consistently shown the beneficial effects of T4 treatment on serum lipid levels in SCH patients [13]. Nonetheless, reductions in carotid intima-media thickness [46] and improvements in brachial artery endothelial function have been observed in individuals with SCH following T4 replacement [17]. Thus, the negative effects of SCH on CV function might be improved or reversed by replacement doses of T4. Although only a few studies investigating the CV effects of T4 have been double-blinded and placebo-controlled, these trials concur that T4 replacement therapy improves systolic and diastolic heart function, endothelial function, and carotid intima-media thickness [46]. Similarly, in a small RCT, the normalization of TSH levels following T4 replacement therapy led to an improvement in cardiac function [24]. Moreover, there are new data supporting improved outcomes in younger (<70 years) CHD patients treated with T4 [47]. On the other hand, a Cochrane review from 2007 assessed 12 RCTs of T4 replacement in patients with SCH and concluded that replacement therapy for SCH did not result in improved survival or decreased CV morbidity [48].
The indications for the screening of SCH and the determination of TSH threshold levels for the treatment of SCH have remained a clinical controversy for over many years. Additional observational data are unlikely to adequately address the uncertainties associated with the risks of SCH or the potential benefits and risks of replacement therapy. These concerns will be best addressed in an appropriately powered RCT that assesses clinical outcomes. The European Commission has now funded such a trial; the Thyroid Hormone Replacement for Untreated Older Adults with Subclinical Hypothyroidism (TRUST) study. The TRUST study is a multicenter, double-blinded, placebo-controlled randomized trial designed to assess the multimodal effects of thyroid hormone replacement in 3,000 adults 65 years of age and older with persistent SCH (Clinicaltrials.gov: NCT01660126). In addition to CV events such as CHD, stroke, and heart failure, this trial will evaluate disease-specific and health-related quality of life, muscle function, and cognitive function. This study should definitively clarify the populations that may benefit from T4 replacement by assessing multiple clinical outcomes as well as whether these benefits may be offset by the potential adverse effects of replacement therapy, such as atrial fibrillation and osteoporosis.
The significance of SCH is now widely studied and the data continue to accumulate. In summary, the present review has highlighted the fact that SCH is associated with an increased risk of developing a wide range of adverse health outcomes and that SCH might represent a potentially modifiable risk factor of CVD and mortality. Therefore, understanding the prevalence and risk factors of SCH could aid in the prevention of CVD in this population. However, until the results of the TRUST study are published and current clinical recommendations [349] are updated, the decision to treat or not treat an SCH patient will be based on clinical judgment, clinical practice guidelines, and expert opinion.
Figures and Tables
Table 1
Summary of the Associations between Variations in Thyroid Hormone Parameters within the Population Reference Range and Key Phenotypic Outcomes
References
1. Cooper DS, Biondi B. Subclinical thyroid disease. Lancet. 2012; 379:1142–1154.
2. Leese GP, Flynn RV, Jung RT, Macdonald TM, Murphy MJ, Morris AD. Increasing prevalence and incidence of thyroid disease in Tayside, Scotland: the Thyroid Epidemiology Audit and Research Study (TEARS). Clin Endocrinol (Oxf). 2008; 68:311–316.
3. Surks MI, Ortiz E, Daniels GH, Sawin CT, Col NF, Cobin RH, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA. 2004; 291:228–238.
4. Biondi B, Cooper DS. The clinical significance of subclinical thyroid dysfunction. Endocr Rev. 2008; 29:76–131.
5. Kim YA, Park YJ. Prevalence and risk factors of subclinical thyroid disease. Endocrinol Metab (Seoul). 2014; 29:20–29.
6. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000; 160:526–534.
7. Kim TH, Choi HS, Bae JC, Moon JH, Kim HK, Choi SH, et al. Subclinical hypothyroidism in addition to common risk scores for prediction of cardiovascular disease: a 10-year community-based cohort study. Eur J Endocrinol. 2014; 171:649–657.
8. Knudsen N, Laurberg P, Rasmussen LB, Bulow I, Perrild H, Ovesen L, et al. Small differences in thyroid function may be important for body mass index and the occurrence of obesity in the population. J Clin Endocrinol Metab. 2005; 90:4019–4024.
9. Taylor PN, Razvi S, Pearce SH, Dayan CM. Clinical review: a review of the clinical consequences of variation in thyroid function within the reference range. J Clin Endocrinol Metab. 2013; 98:3562–3571.
10. Liu D, Jiang F, Shan Z, Wang B, Wang J, Lai Y, et al. A cross-sectional survey of relationship between serum TSH level and blood pressure. J Hum Hypertens. 2010; 24:134–138.
11. Asvold BO, Bjoro T, Nilsen TI, Vatten LJ. Association between blood pressure and serum thyroid-stimulating hormone concentration within the reference range: a population-based study. J Clin Endocrinol Metab. 2007; 92:841–845.
12. Ye Y, Xie H, Zeng Y, Zhao X, Tian Z, Zhang S. Association between subclinical hypothyroidism and blood pressure: a meta-analysis of observational studies. Endocr Pract. 2014; 20:150–158.
13. Pearce EN. Update in lipid alterations in subclinical hypothyroidism. J Clin Endocrinol Metab. 2012; 97:326–333.
14. Liu XL, He S, Zhang SF, Wang J, Sun XF, Gong CM, et al. Alteration of lipid profile in subclinical hypothyroidism: a meta-analysis. Med Sci Monit. 2014; 20:1432–1441.
15. Park YJ, Lee YJ, Choi SI, Chun EJ, Jang HC, Chang HJ. Impact of subclinical hypothyroidism on the coronary artery disease in apparently healthy subjects. Eur J Endocrinol. 2011; 165:115–121.
16. Marfella R, Ferraraccio F, Rizzo MR, Portoghese M, Barbieri M, Basilio C, et al. Innate immune activity in plaque of patients with untreated and L-thyroxine-treated subclinical hypothyroidism. J Clin Endocrinol Metab. 2011; 96:1015–1020.
17. Razvi S, Ingoe L, Keeka G, Oates C, McMillan C, Weaver JU. The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trial. J Clin Endocrinol Metab. 2007; 92:1715–1723.
18. Takamura N, Akilzhanova A, Hayashida N, Kadota K, Yamasaki H, Usa T, et al. Thyroid function is associated with carotid intima-media thickness in euthyroid subjects. Atherosclerosis. 2009; 204:e77–e81.
19. Suh S, Lee MK. Metabolic syndrome and cardiovascular diseases in Korea. J Atheroscler Thromb. 2014; 21:Suppl 1. S31–S35.
20. Iwen KA, Schroder E, Brabant G. Thyroid hormones and the metabolic syndrome. Eur Thyroid J. 2013; 2:83–92.
21. Nakajima Y, Yamada M, Akuzawa M, Ishii S, Masamura Y, Satoh T, et al. Subclinical hypothyroidism and indices for metabolic syndrome in Japanese women: one-year follow-up study. J Clin Endocrinol Metab. 2013; 98:3280–3287.
22. Lee YK, Kim JE, Oh HJ, Park KS, Kim SK, Park SW, et al. Serum TSH level in healthy Koreans and the association of TSH with serum lipid concentration and metabolic syndrome. Korean J Intern Med. 2011; 26:432–439.
23. Oh JY, Sung YA, Lee HJ. Elevated thyroid stimulating hormone levels are associated with metabolic syndrome in euthyroid young women. Korean J Intern Med. 2013; 28:180–186.
24. Monzani F, Di Bello V, Caraccio N, Bertini A, Giorgi D, Giusti C, et al. Effect of levothyroxine on cardiac function and structure in subclinical hypothyroidism: a double blind, placebo-controlled study. J Clin Endocrinol Metab. 2001; 86:1110–1115.
25. Brenta G, Mutti LA, Schnitman M, Fretes O, Perrone A, Matute ML. Assessment of left ventricular diastolic function by radionuclide ventriculography at rest and exercise in subclinical hypothyroidism, and its response to L-thyroxine therapy. Am J Cardiol. 2003; 91:1327–1330.
26. Nanchen D, Gussekloo J, Westendorp RG, Stott DJ, Jukema JW, Trompet S, et al. Subclinical thyroid dysfunction and the risk of heart failure in older persons at high cardiovascular risk. J Clin Endocrinol Metab. 2012; 97:852–861.
27. Biondi B, Fazio S, Palmieri EA, Carella C, Panza N, Cittadini A, et al. Left ventricular diastolic dysfunction in patients with subclinical hypothyroidism. J Clin Endocrinol Metab. 1999; 84:2064–2067.
28. Madathil A, Hollingsworth KG, Blamire AM, Razvi S, Newton JL, Taylor R, et al. Levothyroxine improves abnormal cardiac bioenergetics in subclinical hypothyroidism: a cardiac magnetic resonance spectroscopic study. J Clin Endocrinol Metab. 2015; 100:E607–E610.
29. Gencer B, Collet TH, Virgini V, Bauer DC, Gussekloo J, Cappola AR, et al. Subclinical thyroid dysfunction and the risk of heart failure events: an individual participant data analysis from 6 prospective cohorts. Circulation. 2012; 126:1040–1049.
30. Asvold BO, Bjoro T, Platou C, Vatten LJ. Thyroid function and the risk of coronary heart disease: 12-year follow-up of the HUNT study in Norway. Clin Endocrinol (Oxf). 2012; 77:911–917.
31. Ceresini G, Ceda GP, Lauretani F, Maggio M, Usberti E, Marina M, et al. Thyroid status and 6-year mortality in elderly people living in a mildly iodine-deficient area: the aging in the Chianti Area Study. J Am Geriatr Soc. 2013; 61:868–874.
32. Gussekloo J, van Exel E, de Craen AJ, Meinders AE, Frolich M, Westendorp RG. Thyroid status, disability and cognitive function, and survival in old age. JAMA. 2004; 292:2591–2599.
33. Pereg D, Tirosh A, Elis A, Neuman Y, Mosseri M, Segev D, et al. Mortality and coronary heart disease in euthyroid patients. Am J Med. 2012; 125:826.e7–826.e12.
34. Tseng FY, Lin WY, Lin CC, Lee LT, Li TC, Sung PK, et al. Subclinical hypothyroidism is associated with increased risk for all-cause and cardiovascular mortality in adults. J Am Coll Cardiol. 2012; 60:730–737.
35. Ittermann T, Haring R, Sauer S, Wallaschofski H, Dorr M, Nauck M, et al. Decreased serum TSH levels are not associated with mortality in the adult northeast German population. Eur J Endocrinol. 2010; 162:579–585.
36. Parle JV, Maisonneuve P, Sheppard MC, Boyle P, Franklyn JA. Prediction of all-cause and cardiovascular mortality in elderly people from one low serum thyrotropin result: a 10-year cohort study. Lancet. 2001; 358:861–865.
37. Westerink J, van der Graaf Y, Faber DR, Spiering W, Visseren FL. SMART study group. Relation between thyroid-stimulating hormone and the occurrence of cardiovascular events and mortality in patients with manifest vascular diseases. Eur J Prev Cardiol. 2012; 19:864–873.
38. Selmer C, Olesen JB, Hansen ML, von Kappelgaard LM, Madsen JC, Hansen PR, et al. Subclinical and overt thyroid dysfunction and risk of all-cause mortality and cardiovascular events: a large population study. J Clin Endocrinol Metab. 2014; 99:2372–2382.
39. Hyland KA, Arnold AM, Lee JS, Cappola AR. Persistent subclinical hypothyroidism and cardiovascular risk in the elderly: the cardiovascular health study. J Clin Endocrinol Metab. 2013; 98:533–540.
40. Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010; 304:1365–1374.
41. Ochs N, Auer R, Bauer DC, Nanchen D, Gussekloo J, Cornuz J, et al. Meta-analysis: subclinical thyroid dysfunction and the risk for coronary heart disease and mortality. Ann Intern Med. 2008; 148:832–845.
42. Zhang Y, Chang Y, Ryu S, Cho J, Lee WY, Rhee EJ, et al. Thyroid hormones and mortality risk in euthyroid individuals: the Kangbuk Samsung health study. J Clin Endocrinol Metab. 2014; 99:2467–2476.
43. Li M, Tang Z. Subclinical hypothyroidism: to treat or not to treat? Med Princ Pract. 2015; 24:99–100.
44. Adrees M, Gibney J, El-Saeity N, Boran G. Effects of 18 months of L-T4 replacement in women with subclinical hypothyroidism. Clin Endocrinol (Oxf). 2009; 71:298–303.
45. Danese MD, Ladenson PW, Meinert CL, Powe NR. Clinical review 115: effect of thyroxine therapy on serum lipoproteins in patients with mild thyroid failure: a quantitative review of the literature. J Clin Endocrinol Metab. 2000; 85:2993–3001.
46. Monzani F, Caraccio N, Kozakowa M, Dardano A, Vittone F, Virdis A, et al. Effect of levothyroxine replacement on lipid profile and intima-media thickness in subclinical hypothyroidism: a double-blind, placebo-controlled study. J Clin Endocrinol Metab. 2004; 89:2099–2106.
47. Razvi S, Weaver JU, Butler TJ, Pearce SH. Levothyroxine treatment of subclinical hypothyroidism, fatal and nonfatal cardiovascular events, and mortality. Arch Intern Med. 2012; 172:811–817.
48. Villar HC, Saconato H, Valente O, Atallah AN. Thyroid hormone replacement for subclinical hypothyroidism. Cochrane Database Syst Rev. 2007; (3):CD003419.
49. Helfand M. U.S. Preventive Services Task Force. Screening for subclinical thyroid dysfunction in nonpregnant adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004; 140:128–141.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download