Abstract
Acute suppurative thyroiditis (AST) is a rare condition, as the thyroid gland is relatively resistant to infection. Thyroid function tests are usually normal in AST. A few cases of AST associated with thyrotoxicosis have been reported in adults. We report a case of AST that was associated with thyrotoxicosis in a 70-year-old woman. We diagnosed AST with thyroid ultrasonography and fine needle aspiration of pus. The patient improved after surgical intervention and had no anatomical abnormality. Fine needle aspiration is the best method for the difficult task of differentiating malignancy and subacute thyroiditis from AST with thyrotoxicosis. Earlier diagnosis and proper treatment for AST might improve the outcome.
Acute suppurative thyroiditis (AST) is an uncommon condition that occurs in 0.1% to 0.7% of thyroid diseases [1]. Anatomically, the thyroid gland is a completely capsulated structure that has sufficient blood supply and lymphatic vessels. It is an organ that is not so susceptible to infections due to the high concentration of iodine [2]. It has been reported that 5% to 10% of AST cases show abnormal levels of thyroid hormone, but cases accompanied by thyrotoxicosis are quite rare [3]. In the literature, there have only been eight cases of AST combined with thyrotoxicosis overseas from 1996 to 2001 [4], and 10 cases after 2004 [1]. In Korea, six cases were reported since 2004, with three of the cases in children [2,5-9]. Among the cases reported locally and internationally, most patients had underlying diseases such as AIDS, diabetes and cancer, or had anatomical deformities such as pyriform sinus fistula and thyroglossal duct cyst. Here, we report a literature review and our experience with one case of AST accompanied with thyrotoxicosis in an elderly 70-year-old patient who had no special medical history other than hypertension and had no abnormal anatomical structure.
The patient was transferred to our hospital due to the finding of thyrotoxicosis during an in-patient stay at another hospital where she was being treated for a 2-week fever and systemic debilitation.
The patient had hypertension and had taken antihypertensive medication for 20 years.
The patient was quite alert, but showed signs of acute illness. Her blood pressure measured 120/80 mm Hg, pulse rate was 110 bpm, respiratory rate was 20 times per minutes and axillary temperature was 38.4℃. Based on examinations of her head and neck, a lump was detected and palpitation of the lump was accompanied by local heatness and minor tenderness. The lump was fixated and soft. There was no finding of tenderness of the paranasal sinus or pharyngolaryngeal flare, tonsillar hypertrophy, or enlargements of lymph node.
The blood assay revealed that white blood cell (WBC) count was 13,500/mm3 (neutrophils, 80.9%), hemoglobin was 9.3 g/dL, and platelet was 456,000/µL. The erythrocyte sedimentation rate (ESR) increased to 151 mm/hr, and C-reactive protein increased to 24.7 mg/dL. The endocrinology report showed that T3 was 228.0 ng/dL (normal range, 80 to 200), free T4 (FT4) was >7.77 ng/dL (normal range, 0.93 to 1.7), thyroid stimulating hormone (TSH) was 0.02 µIU/mL (normal range, 0.27 to 4.2), and thyroglobulin was >5,000 ng/mL (normal range, 1.4 to 78). Antimicrosome antibody (Ab), antithyroglobulin Ab, and thyroid stimulating Ab were in the normal ranges. Serum calcitonin was in the normal range of less than 1.0 pg/mL, and the HIV Ab test was negative.
The 99mTc thyroid scan showed that the radioactive isotope intake of the thyroid was reduced and irregular (Fig. 1).
The margin of the right side of the thyroid was unclear and a multilobulated lump with poor contrast was observed. Multiple lymph nodes were observed from the IV, V, and VI areas of the right side of the neck (Fig. 2).
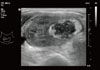
Neck sonography revealed that there were no abnormal structures found in the homogeneous image of the left lobe of the thyroid, but in the right lobe, there was a mass that was about 4.5×2.5×4.6 cm in size with heterogeneous echogenicity (Fig. 3). Using fine needle aspiration biopsy, we obtained chocolate-colored abscess fluid that was chocolate in color (Fig. 4), and a cytopathogenic test revealed no atypical cells or malignant cells, but many neutrophil cells and histiocytes were observed.
Immediately, we commenced with treatment by administration of amoxicillin/clavulanate 1 g/200 mg three times a day and prescribed 40 mg propranolol four times a day for relieving the symptoms of thyrotoxicosis. No microbes were identified from the culture test of aspirated samples from blood or thyroid gland. Hyperpyrexia gradually disappeared within 3 days after administration of antibiotics, but the feeling of local fever, neck swelling and tenderness continued for up to 10 days after administration of antibiotics. We performed a thyroid lobectomy and found that the abscess was accompanied by fibrosis in the right lobe of the thyroid. The pathological findings revealed inflammation accompanied by necrotic tissue and abscess.
After the surgery, the patient showed symptomatic recovery from neck pain and swelling, and was discharged from the hospital. We performed outpatient follow-up with esophagography and neck computed tomography (CT) and we could not find any anatomical defect such as fistula. A thyroid function test in the outpatient department at 2 months after surgery revealed that FT4 was 1.02 ng/dL and TSH was 2.40 µIU/mL, indicating that thyroid function had been restored to normal.
AST is a rare infectious disease that occurs mostly in patients with existing thyroid diseases or in immunocompromised patients. Many cases of AST are accompanied by anatomical deformities such as pyriform sinus fistula and thyroglossal duct cyst, and in rare cases it occurs as a complication induced by fine needle aspiration test or esophageal microperforation [4,10,11]. The clinical symptoms are lump, flare and pain mainly in the anterior neck, accompanied by fever. An increase in WBC count and left-shift was observed in 57% to 73% of AST cases, but if the infection involved anaerobic bacteria, the patient showed a normal WBC count. AST is associated with an elevation in the ESR and increase in the C-reaction protein level, but the results of most thyroid function tests and autoantibodies are normal. Based on thyroid scanning, cold-nodule can be found from the site where the lesion is. Ultrasound examination and CT scan become helpful for structural observation of abscess and around abscess [1,11,12].
Serum levels of thyroid hormone can be transiently increased due to release of preformed thyroid hormone into the circulation resulting from the destruction of the thyroid follicles in the acute phase, but most cases are normal. As seen in this case, the AST was accompanied by thyrotoxicosis with suppurative inflammation, pus, and thyroid cellular disruptions inducing excessive discharge of thyroid hormone.
The case of AST accompanied by thyrotoxicosis is difficult to differentiate from subacute thyroiditis or thyroid cancer. The subacute thyroiditis occurs after an upper airway infection and is the most common cause of painful thyroid disease. It is similar to AST in the onset profile. The thyroid scan revealed decreased and inhomogeneous radioactive isotope uptake. Subacute thyroiditis involves the entire thyroid and thyrotoxicosis occurs due to the temporary discharge of thyroid hormone caused by the destruction of about 50% of the thyroid tissue in the early stage of disease. Meanwhile, AST is rarely accompanied by thyrotoxicosis, so that it is an important finding for differentiation from subacute thyroiditis [5,6,13]. As in this case, AST accompanied by thyrotoxicosis is more difficult to differentiate from subacute thyroiditis, resulting in cases with delayed diagnosis due to misdiagnosis as subacute thyroiditis [1,5]. The aggressive malignant thyroid tumor also has a similar onset profile to that of AST, which makes differentiation even more difficult. In a patient with a family history of medullary thyroid cancer, the level of calcitonin measured from the substances obtained by the fine needle aspiration of serum or thyroid can be somewhat helpful [1]. Therefore, when there is no improvement in the clinical profile in spite of suitable antibiotic treatment and drainage of pus for 1 week, then thyroid cancer should be suspected [14]. The most important diagnostic method that can differentiate AST from the other diseases is fine needle aspiration of the thyroid to detect pus or bacteria [1,5,8,15]. In the case of subacute thyroiditis, it is possible to observe multinucleated giant cell granuloma and mononuclear cell infiltration [1]. In this case, we found pus from the fine needle aspiration and we were able to make the diagnosis of AST.
The most common causative bacteria of AST are Streptococcus pyogenes and Staphylococcus aureus and they have been verified as the causative bacteria from about 39% of reported cases. In addition, Gram-negative bacilli, anaerobes, tubercle bacilli and fungi can be causes, and polymicrobial infection has been reported in about 30% of cases [1,8,11,12]. There has been a reported case with no identified microbe [16,17], but nothing is clearly known about the identification rate with bacterial culture [1]. In this case, there were attempts to culture anaerobes, tubercle bacilli and fungi, but no microbe was identified. In this case, it was thought that the culture test results were affected by the fact that the patient had received a combination of ≥2 types of broad-spectrum antibiotics for 1 week from another hospital.
The treatment of AST involves the use of antibiotics or antifungal agents and surgical resection of the thyroid lobe or drainage of the pus. When any anatomical defect such as pyriform sinus fistula is identified and thyroiditis occurs repeatedly, fistulectomy should be performed [5,18]. Recently, it has become the trend to treat AST without undergoing any surgical treatment by using suitable antibiotics when the size of abscess is small enough that it cannot be seen by CT scan [3], or if it is a single lump with relatively clear margin [1,3,19]. Ilyin et al. [19] treated AST without surgical intervention by draining pus with needle aspiration and direct injection of antibiotics into the drainage site. However, this case involved a broad spectrum infection accompanied by thyrotoxicosis and the lump involved multiple lobes, so there were limits in the drainage, and even after administration of antibiotics, there was still local fever, neck swelling and tenderness. Therefore, we decided to perform surgical treatment. The postoperative symptoms of the patients and the thyroid function test demonstrated gradual improvement and esophagography and neck CT scan revealed that there were no anatomical defects.
In summary, we diagnosed one case of AST accompanied by thyrotoxicosis in an elderly patient who had no other underlying disease other than hypertension, and who had no anatomical deformities around the thyroid. After implementing a treatment with antibiotics and surgical intervention, there was a good postoperative prognosis. In this report, we discuss the case and provide a review of the literature. AST accompanied by thyrotoxicosis is difficult to differentiate from subacute thyroiditis and thyroid cancer. So, any sudden aggravation and occurrence of complications may be prevented by detection of pus or bacteria through thyroid fine needle aspiration test and by suitable postdiagnostic treatment.
Figures and Tables
Fig. 2
Computed tomography scan showed a large, multiseptated, low attenuated mass in the right thyroid lobe and enlarged lymph node in the right neck level IV, V, and VI areas.

References
1. Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, Kloos RT. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010. 20:247–255.
2. Nam SM, Lee MY, Koh JH, Sung KJ, Chung CH. A case of acute perithyroiditis with transient thyrotoxicosis in childhood. J Korean Soc Endocrinol. 2006. 21:142–145.
3. Lethert K, Bowerman J, Pont A, Earle K, Garcia-Kennedy R. Methicillin-resistant Staphylococcus aureus suppurative thyroiditis with thyrotoxicosis. Am J Med. 2006. 119:e1–e2.
4. Nishihara E, Miyauchi A, Matsuzuka F, Sasaki I, Ohye H, Kubota S, Fukata S, Amino N, Kuma K. Acute suppurative thyroiditis after fine-needle aspiration causing thyrotoxicosis. Thyroid. 2005. 15:1183–1187.
5. Kim KW, Park YJ, Kim TY, Moon MK, Han SW, Eun CJ, Kim YA, Jin TH, Chung HS, Park DJ, Cho BY. A case of acute suppurative thyroiditis caused by pyriform sinus fistula with thyrotoxicosis. J Korean Soc Endocrinol. 2004. 19:69–75.
6. Sung KH, Chung S. A child of acute suppurative thyroiditis with transient thyrotoxicosis. J Korean Soc Pediatr Endocrinol. 2006. 11:209–212.
7. Yoo CH, Kim YN, Shon CB, Park EH, Choi YS, Park YH, Kim JH. A case of acute suppurative thyroiditis with thyrotoxicosis. Korean J Med. 2008. 75:242–245.
8. Jee SH, Kim EY. Acute suppurative thyroiditis caused by methicillin: resistant Staphylococcus aureus in healthy children. J Korean Soc Pediatr Endocrinol. 2011. 16:128–132.
9. Choi HS, Ahn HY, Lee JS, Kim H, Lim JA, Kim TH, Kim M, Lee Y, Park DJ, Cho BY. A case of acute suppurative thyroiditis in a patient with leukemia who was treated with chemotherapy. J Korean Endocr Soc. 2009. 24:38–41.
10. Yung BC, Loke TK, Fan WC, Chan JC. Acute suppurative thyroiditis due to foreign body-induced retropharyngeal abscess presented as thyrotoxicosis. Clin Nucl Med. 2000. 25:249–252.
11. Singer PA. Thyroiditis. Acute, subacute, and chronic. Med Clin North Am. 1991. 75:61–77.
12. Herndon MD, Christie DB, Ayoub MM, Duggan AD. Thyroid abscess: case report and review of the literature. Am Surg. 2007. 73:725–728.
13. Houghton DJ, Gray HW, MacKenzie K. The tender neck: thyroiditis or thyroid abscess? Clin Endocrinol (Oxf). 1998. 48:521–524.
14. Lin KD, Lin JD, Huang MJ, Huang HS, Jeng LB, Ho YS. Acute suppurative thyroiditis and aggressive malignant thyroid tumors: differences in clinical presentation. J Surg Oncol. 1998. 67:28–32.
15. McLaughlin SA, Smith SL, Meek SE. Acute suppurative thyroiditis caused by Pasteurella multocida and associated with thyrotoxicosis. Thyroid. 2006. 16:307–310.
16. Brook I. Microbiology and management of acute suppurative thyroiditis in children. Int J Pediatr Otorhinolaryngol. 2003. 67:447–451.
17. Yu EH, Ko WC, Chuang YC, Wu TJ. Suppurative Acinetobacter baumanii thyroiditis with bacteremic pneumonia: case report and review. Clin Infect Dis. 1998. 27:1286–1290.
18. Fukata S, Miyauchi A, Kuma K, Sugawara M. Acute suppurative thyroiditis caused by an infected piriform sinus fistula with thyrotoxicosis. Thyroid. 2002. 12:175–178.
19. Ilyin A, Zhelonkina N, Severskaya N, Romanko S. Nonsurgical management of thyroid abscess with sonographically guided fine needle aspiration. J Clin Ultrasound. 2007. 35:333–337.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download