Abstract
Parathyroid cysts, which can be divided into functional and non-functional cysts, are rare causes of primary hyperparathyroidism. A technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi) parathyroid scan is a sensitive diagnostic tool for the localization, although it sometimes shows a false-negative result. Here we report a case of presumed cystic parathyroid adenoma based on clinical findings and analysis of cystic fluid with negative findings in a parathyroid scan. A 44-year-old male patient visited the hospital due to leg pain and compressive symptoms (dysphagia, hoarseness) that had started 4-5 months before. His serum calcium level was 14.4 mg/dL and his intact parathyroid hormone (iPTH) had increased to 478.1 pg/mL. On neck computed tomography, a cystic nodule measuring 6.2 cm was detected in the inferior part of the right thyroid gland. Sestamibi uptake for this nodule was not detected on 2-h delayed imaging, and fluorodeoxyglucose positron emission tomography showed only subtle uptake. Fine-needle aspiration was performed and intracystic iPTH had increased to 61,600 pg/mL. Focused parathyroidectomy guided by intraoperative iPTH monitoring led to successful enucleation of the right inferior parathyroid gland. A parathyroid adenoma was confirmed, and his laboratory results had normalized. This study shows that cystic parathyroid adenoma can sometimes be difficult to detect on a 99mTc-sestamibi parathyroid scan.
Primary hyperparathyroidism (PHPT) is a condition characterized by an excess secretion of parathyroid hormone by adenomatous or hyperplastic glands or rarely by parathyroid cysts or parathyroid carcinomas. PHPT is a relatively common disorder but a parathyroid cyst is very rare among the causes of PHPT. Epidemiological studies have found incidence rates of PHPT ranging from 25 to 28 cases/100,000 population annually, and approximately 350 cases (or 0.5-1% of all parathyroid pathologies) of cystic parathyroid lesions have been reported in the literature. Almost 90% of these are classified as non-functioning cystic lesions, and have been found in individuals with normal calcium concentrations. In the remaining approximately 10% of cases, the cystic parathyroid lesions were functional, and responsible for PHPT.
Surgical removal of hyperfunctioning parathyroid tissue by an experienced endocrine surgeon achieves permanent remission in 85-90% of initial neck explorations [1,2]. Thus, accurate preoperative localization of parathyroid adenoma is important to reduce the operative failure rate. A major diagnostic technique is a technetium-99m-methoxyisobutylisonitrile (99mTc-sestamibi or methoxy isobutyl isonitrile [MIBI]) scan.
In this report, we present a rare case of a parathyroid adenoma that was cystic and not detected by 99mTc-sestamibi scanning. Usually, it is difficult to make a confirmative diagnosis of hyperfunctioning cystic parathyroid adenoma before operation. But in this case, we could diagnose a hyperfunctioning cystic parathyroid adenoma before surgery by measuring intact parathyroid hormone (iPTH) level of cyst fluid aspirate and accomplish successful focused enucleation of cystic parathyroid adenoma.
A 44-year-old man was referred and admitted to the endocrine department for examination of hypercalcemia and an extremely high level of iPTH. He presented with progressive hip, thigh and calf pain that had started 5 months ago. In addition, 4 months ago, compressive symptoms including dysphagia and hoarseness occurred. He had no specific history of other disease, except for appendicitis and no significant family history. On physical examination, there was a palpable solid mass on the right side of the neck, but no lymphadenopathy or bony tenderness. Neurological examination was normal. On admission, his calcium level was 14.4 mg/dL, phosphorus 2.0 mg/dL, iPTH 478.1 pg/mL and alkaline phosphatase 125 IU/L. His renal function was chemically normal. Serum creatinine level was 0.99 mg/dL.
The patient was assumed to have PHPT. X-rays of the pelvis and spine showed no osteolytic lesions and no radio-opacity suggesting urinary stones. His bone mineral density was within the normal range. The T-score was -0.8 at the femur neck and -1.0 at the lumbar region. Computed tomography (CT) examination of the neck revealed a predominantly cystic mass, 6.2 × 3.8 × 2.7 cm in size, situated in the lower lobe of right thyroid gland. There were a few small lymph nodes both at level V, but no vascular invasion (Fig. 1).
A 99mTc-sestamibi scan was performed to diagnose parathyroid adenoma and to determine the location of the cystic mass before operation. However, the scan unexpectedly failed to detect a parathyroid tumor (Fig. 2). Fluorodeoxyglucose positron emission tomography (FDG-PET) showed only subtle uptake on the lower lobe of right thyroid gland (Fig. 3). Based on these findings, there was insufficient evidence to determine whether the cystic mass was a parathyroid lesion or a thyroid lesion. Ultrasound-guided aspiration of the cystic mass contained bloody fluid and presented insufficient tissue for pathologic diagnosis. But the iPTH level of intracystic fluid aspirate was 61,600 pg/mL, which strongly suggested that the cystic mass was a parathyroid lesion.
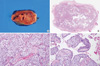
Hyperfunctioning cystic parathyroid adenoma was highly suspected and an operation was performed after correction of hypercalcemia. During the operation, a large cyst of about 6 cm in diameter was revealed. The surgeons aspirated the cyst because it was so tense and large that it made enucleation of the mass difficult. Blood was sampled to monitor the iPTH level intra- and perioperatively, which was measured by a chemiluminescence immunoassay. The iPTH level decreased almost immediately after enucleation; from a pre-incision value of 300.3 pg/mL to a 5-minute post-incision value of 49.5 pg/mL. The mass was surgically removed and tissues were sent for pathological examination. Sections revealed a parathyroid neoplasm, size 2.3 × 2.0 × 1.4 cm, weight 11.5 g, mainly composed of parathyroid chief cells without focal atypical nuclei. It was well vascularized and showed no angiolymphatic invasions. Mitotic figures and tumor necrosis were not present. In cystic areas of the tumor, epithelial lining cells were not observed. This tumor was therefore compatible with a cystic parathyroid adenoma (Fig. 4).
Sixteen hours after the operation, the iPTH level had decreased to value of < 5 pg/mL. Serum calcium and phosphorus levels were 8.6 and 3.2 mg/dL, respectively, on the discharge date. After 1 week of follow-up, the patient remained normocalcemic (calcium, 9.0 mg/dL; phosphorus, 3.8 mg/dL) and the hip pain had markedly improved.
The pathogenesis of parathyroid cysts remains unclear. Parathyroid cysts can be divided into functional and non-functional cysts depending on their association with hypercalcemia. A series of 813 parathyroidectomies for PHPT at the Mayo clinic showed that 3% of the cases were cystic in nature [3]. Treatment of parathyroid cyst includes aspiration, injection of sclerosing agents or surgical excision. Fine-needle aspiration may be curative in some of the non-functional cysts but parathyroidectomy seems to be the treatment of choice for functional parathyroid cysts.
The accurate localization of a hyperfunctioning gland among the four parathyroid glands is very important for successful focused neck exploration and parathyroidectomy. A 99mTc-sestamibi scan provides a simple and non-invasive test for the localization of a hyperfunctioning parathyroid gland. The 'single isotope, double-phase technique' is based on the fact that MIBI washes out more rapidly from the normal thyroid than from hyperfunctioning parathyroid tissue. However, some parathyroid lesions do not retain sestamibi whereas others (such as the thyroid and lymph nodes) do, resulting in false-negative or false-positive studies. The overall reported sensitivity and specificity for the 99mTc-sestamibi scan is variable from center to center, with values of 98.1% and 97%, respectively, in one study, 70.2% and 50.0% respectively, in others [4,5]. The reasons for this variability in sensitivity and specificity are unclear.
Ujiki et al. [6] reported that 99mTc-sestamibis were performed in three of the seven patients who had parathyroid cysts, including two with functional cysts. None of them showed focal uptake. Negative findings for PHPT on 99mTc-sestamibi scanning have been reported in several studies and some probable factors relating to the failure of 99mTc-sestamibi to identify a hyperfunctioning parathyroid gland have been suggested, as follows.
First, the size of the parathyroid tumor is the major factor influencing the sensitivity of the 99mTc-sestamibi scan [7,8]. The size of parathyroid cyst is variable. Calandra et al. [9] reported 11 parathyroid cysts ranged in size from 1.6 to 10 cm with a mean of 3.9 cm. False-negative 99mTc-sestamibi scans have been reported in very small or large tumors [10,11]. In this case, the mass size was about 6 cm, which could be related to the false-negative scan result.
Second, serum iPTH level is associated with sestamibi scan findings. Of 83 patients who had imaging by 99mTc-sestamibi, there were 21 false negatives, and the difference in the mean iPTH level in patients with positive and negative findings was found to be statistically significant (367 pg/mL vs. 148 pg/mL) [12]. However, the overlap of iPTH levels in positive and negative scans does not allow confident selection for preoperative scanning. In addition, as the parathyroid adenoma size may be correlated to the iPTH level, the preoperative iPTH level might be useful for estimating the amount of hyperfunctioning parathyroid tissue to be secreted [10]. This case showed serum iPTH level as 478.1 pg/mL. Compared to previous cases, patients had relatively high iPTH level, severe hypercalcemia and symptoms, which could suggest higher possibilities of positive scan findings reflecting the abundant amount of hyperfunctioning parathyroid tissue. However, in this case, 99mTc-sestamibi scan showed a negative result. There was a strong possibility of false-negative scan result, since serum iPTH was considerably high.
Third, parathyroid cell types are correlated with the detectability of parathyroid tumors by 99mTc-sestamibi scanning. The lipophilic radiotracer 99mTc-sestamibi becomes concentrated in cells and inside the mitochondria through active transport and passive diffusion. Uptake of the 99mTc-sestamibitracer has been correlated with oxyphile cell content [13] and metabolic activity within the cells could determine the amount of sestamibi uptake [14]. However, in metabolically hyperactive cells, the amount of sestamibi uptake reveals variation, reflecting the numbers of mitochondria and the degree of cellular activity [13]. The histology results showed the cystic area of tumor had low cellular components in the cystic area of tumor which could contribute to the false-negative result in the 99mTc-sestamibi scan.
Fourth, P-glycoprotein (P-gp) expression in parathyroid adenomas has been considered to be another possible factor inducing false-negative findings in 99mTc-sestamibi scan. P-gp is a plasma-membrane lipoprotein encoded by the human multidrug resistance (MDR) gene. On the basis of the chemical structure of 99mTc-sestamibi, it has been suggested that P-gp may act as a drug efflux pump able to transport substrates out of the cell. Sun et al. [15] reported two out of 16 cases of parathyroid adenoma with negative findings on the scan. They revealed positive P-gp expression on immunohistochemistry. However, some authors have reported no correlation with preoperative 99mTc-sestamibi scan [16]. There has been much debate on the correlation of P-gp and false-negative findings.
Finally, serum calcium levels may modify radiotracer kinetics by influencing the membrane potential. Some authors have found a correlation between calcium levels and early tracer uptake. This study supports the concept that serum calcium levels play a key role in modifying sestamibi kinetics by influencing the membrane potential [17].
Each of the above causes could not explain the false-negative results of the 99mTc-sestamibi scan. The exact mechanism by which 99mTc-sestamibi accumulates in hyperfunctional parathyroid tissue is not yet known. Although some controversial results have been reported in the literature, the above-described factors may each play a role in individual cases. The large size, high calcium level and low cellular component in cystic area of tumor could have contributed to the false-negative result of 99mTc-sestamibi scan in this case.
Before the use of fine-needle aspiration and fluid analysis for iPTH level, most parathyroid cysts were discovered during surgery for presumed thyroid disease, in patients presenting with a neck mass, with or without symptoms of compression. With only imaging tools, it is difficult to differentiate parathyroid cysts from thyroid cysts, thyroglossal duct cyst and even thyroid carcinomas. The iPTH level of the cystic fluid cannot differentiate between functioning and nonfunctioning parathyroid cyst. However, functional cysts may contain foci of hemorrhage or necrosis and brown, turbid or even bloody cystic fluid compared to nonfunctional cysts, which usually contain clear, colorless cystic fluid. It is believed that these cysts may arise from degenerating adenomas. In this case, both the aspect of the extracted cystic fluid and the histology of resected mass indicate a functional cyst. A high iPTH level and characteristic in aspirated cystic fluid could help to determine the origin of the cyst (parathyroid or thyroid) and localizing hyperfunctioning parathyroid mass [18].
The efficacy of PET scan for cystic parathyroid adenoma was reported to be more sensitive than 99mTc-sestamibi scan in preoperative detection and localization of parathyroid adenomas [19]. However, in this case, the FDG-PET scan showed subtle uptake of cystic mass in right thyroid lobe on the FDG-PET. The FDG-PET scan helped to detect and localize abnormal tissue, but could not differentiate the origin of abnormal tissue. The use of FDG-PET rather than 99mTc-sestamibi is not recommended for diagnosis of hyperparathyroidism, because the sensitivity of FDG-PET is still questionable and cost is considerable higher than 99mTc-sestamibi scan.
In case of hyperparathyroidism with negative 99mTc-sestamibi scan, bilateral neck exploration is usually performed due to possibility of other pathologic glands. Intraoperative iPTH monitoring has helped to confirm the diagnosis of PHPT and to do minimally invasive parathyroidectomy [20]. The iPTH level declined more than 50% at 5 minutes after enucleation of cystic mass in this case. Monitoring of intraoperative iPTH levels helps successful focused neck exploration and parathyroidectomy, especially in patients with negative 99mTc-sestamibi scan.
Cystic parathyroid adenoma is rare and an unusual cause of PHPT. We have reported the case of a cystic parathyroid adenoma with PHPT that did not show up in a 99mTc-sestamibi scan. Serum and cystic fluid examination for iPTH level and neck CT findings helped with the diagnosis in the absence of typical 99mTc-sestamibi findings for PHPT. This case illustrates that the accurate diagnosis should be made on the basis of fine needle aspiration and analysis of cystic fluid for iPTH, combined with serum iPTH level, and that FDG-PET scan hardly help to distinguish the origin of cystic mass. In addition, experienced surgeons should use supplementary tools such as intraoperative iPTH monitoring for successful focused neck exploration and parathyroidectomy.
Figures and Tables
Fig. 1
Neck computed tomography shows a cystic lesion that measured 6.2 × 3.8 × 2.7 cm on the inferior side of the right thyroid lobe.
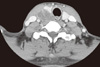
Fig. 2
After injection of 555 MBq (15 mCi) 99mTc-sestamibi, dual-phase scintigraphy was performed. Early (A, at 15 minute) and late (B, at 2.5 hour) images of the anterior neck were obtained using a low-energy high-resolution parallel-hole collimator. There was no 99mTc-sestamibi accumulation corresponding to the cystic lesion detected by neck computed tomography on either the early (A) or delayed (B) images.

Fig. 3
Fluorodeoxyglucose positron emission tomography showed subtle uptake on the lower lobe of right thyroid gland.
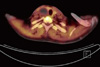
Fig. 4
Gross and microscopic findings of enucleated parathyroid adenoma. A. The tumor was encapsulated and cut surface showed brown color and cystic change. B. Low power view of parathyroid gland showing solid and cystic area (H&E stain, × 0.5). C. The solid area of tumor was showed hypercellular chief cells and well-vascularized (H&E stain, × 200). D. The cystic area of tumor showed vacant cavity with hemorrhage (H&E stain, × 200).
References
1. Rose DM, Wood TF, Van Herle AJ, Cohan P, Singer FR, Giuliano AE. Long-term management and outcome of parathyroidectomy for sporadic primary multiple-gland disease. Arch Surg. 2001. 136:621–626.
2. Udelsman R. Six hundred fifty-six consecutive explorations for primary hyperparathyroidism. Ann Surg. 2002. 235:665–670.
3. Armstrong J, Leteurtre E, Proye C. Intraparathyroid cyst: a tumour of branchial origin and a possible pitfall for targeted parathyroid surgery. ANZ J Surg. 2003. 73:1048–1051.
4. Alabdulkarim Y, Nassif E. Sestamibi (99mTc) scan as a single localization modality in primary hyperparathyroidism and factors impacting its accuracy. Indian J Nucl Med. 2010. 25:6–9.
5. Akbaba G, Berker D, Isik S, Aydin Y, Ciliz D, Peksoy I, Ozuguz U, Tutuncu YA, Guler S. A comparative study of preoperative imaging methods in patients with primary hyperparathyroidism: Us, Mibi, Spect and Mri. J Endocrinol Invest. 2011. In press.
6. Ujiki MB, Nayar R, Sturgeon C, Angelos P. Parathyroid cyst: often mistaken for a thyroid cyst. World J Surg. 2007. 31:60–64.
7. Swanson TW, Chan SK, Jones SJ, Bugis S, Irvine R, Belzberg A, Levine D, Wiseman SM. Determinants of Tc-99m sestamibi SPECT scan sensitivity in primary hyperparathyroidism. Am J Surg. 2010. 199:614–620.
8. Chiu B, Sturgeon C, Angelos P. What is the link between nonlocalizing sestamibi scans, multigland disease, and persistent hypercalcemia? A study of 401 consecutive patients undergoing parathyroidectomy. Surgery. 2006. 140:418–422.
9. Calandra DB, Shah KH, Prinz RA, Sullivan H, Hofmann C, Oslapas R, Ernst K, Lawrence AM, Paloyan E. Parathyroid cysts: a report of eleven cases including two associated with hyperparathyroid crisis. Surgery. 1983. 94:887–892.
10. Biertho LD, Kim C, Wu HS, Unger P, Inabnet WB. Relationship between sestamibi uptake, parathyroid hormone assay, and nuclear morphology in primary hyperparathyroidism. J Am Coll Surg. 2004. 199:229–233.
11. Bénard F, Lefebvre B, Beuvon F, Langlois MF, Bisson G. Rapid washout of technetium-99m-MIBI from a large parathyroid adenoma. J Nucl Med. 1995. 36:241–243.
12. Siegel A, Alvarado M, Barth RJ Jr, Brady M, Lewis J. Parameters in the prediction of the sensitivity of parathyroid scanning. Clin Nucl Med. 2006. 31:679–682.
13. Melloul M, Paz A, Koren R, Cytron S, Feinmesser R, Gal R. 99mTc-MIBI scintigraphy of parathyroid adenomas and its relation to tumour size and oxyphil cell abundance. Eur J Nucl Med. 2001. 28:209–213.
14. Hetrakul N, Civelek AC, Stagg CA, Udelsman R. In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria. Surgery. 2001. 130:1011–1018.
15. Sun SS, Shiau YC, Lin CC, Kao A, Lee CC. Correlation between P-glycoprotein (P-gp) expression in parathyroid and Tc-99m MIBI parathyroid image findings. Nucl Med Biol. 2001. 28:929–933.
16. Jorna FH, Hollema H, Hendrikse HN, Bart J, Brouwers AH, Plukker JT. P-gp and MRP1 expression in parathyroid tumors related to histology, weight and (99m)Tc-sestamibi imaging results. Exp Clin Endocrinol Diabetes. 2009. 117:406–412.
17. Carpentier A, Jeannotte S, Verreault J, Lefebvre B, Bisson G, Mongeau CJ, Maheux P. Preoperative localization of parathyroid lesions in hyperparathyroidism: relationship between technetium-99m-MIBI uptake and oxyphil cell content. J Nucl Med. 1998. 39:1441–1444.
18. Fortson JK, Patel VG, Henderson VJ. Parathyroid cysts: a case report and review of the literature. Laryngoscope. 2001. 111:1726–1728.
19. Neumann DR, Esselstyn CB, Maclntyre WJ, Go RT, Obuchowski NA, Chen EQ, Licata AA. Comparison of FDG-PET and sestamibi-SPECT in primary hyperparathyroidism. J Nucl Med. 1996. 37:1809–1815.
20. Chen H, Pruhs Z, Starling JR, Mack E. Intraoperative parathyroid hormone testing improves cure rates in patients undergoing minimally invasive parathyroidectomy. Surgery. 2005. 138:583–587.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download