Abstract
Background
Whether thyroid lobectomy alone is a sufficient treatment for papillary thyroid microcarcinoma (PTMC) remains controversial. The aim of this study is to evaluate the predictive factors for incidental contralateral carcinoma in patients confirmed of unilateral PTMC preoperatively.
Methods
Between January 2007 and December 2009, 393 patients underwent thyroid surgery for unifocal and unilateral PTMC preoperatively at Pusan National University Hospital. A total thyroidectomy with central neck dissection was routinely performed for these patients during this study period.
Results
Among the 393 cases in the cohort, 77 patients (19.6%) had incidental PTMC in the contralateral lobe. In patients with incidental contralateral carcinoma, there was higher prevalence in extrathyroid extension, occult ipsilateral carcinoma, pathologic Hashimoto's thyroiditis, and central lymph node metastasis compared to those without contralateral carcinoma. The mean tumor size also increased in patients with contralateral carcinoma. Multivariate logistic regression showed that extrathyroid extension (P = 0.049), occult ipsilateral carcinoma (P < 0.001), pathologic Hashimoto's thyroiditis (P = 0.038), and central lymph node metastasis (P = 0.002) were predictive factors for incidental contralateral carcinoma.
Conclusion
In conclusion, multifocality in the ipsilateral lobe, central lymph node metastasis, extrathyroid extension, and Hashimoto's thyroiditis is associated with the presence of contralateral carcinoma. Thus, if these factors are found by preoperative and/or postoperative evaluation, total thyroidectomy or completion thyroidectomy is necessary for the treatment of PTMC.
Papillary thyroid microcarcinoma (PTMC), as s specific subtype of papillary thyroid carcinoma (PTC), which is defined by the World Health Organization as a papillary carcinoma measured at 10 mm or less in its maximal diameter [1]. Recently, technological improvement and widespread use of ultrasonography (US) has helped to identify smaller nodule and routine US-guided fine needle aspiration biopsy (FNAB) for this nodule has facilitated the diagnosis of PTMC. So the incidence of PTMC has increased rapidly [2,3]. PTMC is usually slowly growing and has an excellent prognosis [4,5], so conservative treatment such as unilateral lobectomy has been advocated for some patients with these tumors. However locoregional recurrence has been reported in these patients [6,7] and rare cases distant metastasis have also reported [8].
So the management of PTMC remains controversial [9,10]. Recent consensus guidelines by American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer [11] recommend that lobectomy alone may be sufficient treatment for small (< 1 cm), low-risk, unifocal, and intrathyroidal papillary carcinoma. They classify low risk lesions as those with no lymphovascular invasion or no evidence of more aggressive cellular variants on histologic studies. This recommendation is based, among other considerations, on the risk of contralateral disease [12]. In these patients with PTMC treated by lobectomy, completion thyroidectomy is considered if the risk of PTC in the contralateral lobe was substantial.
The aim of this study was to evaluate any possible predictive factors for incidental contralateral carcinoma in patients confirmed of unifocal and unilateral PTMC preoperatively, then to find out the perioperative factors we could recommend to undergo total thyroidectomy rather than lobectomy in the patients with PTMC.
Between January 2007 and December 2009, 428 patients underwent thyroid surgery for unilateral PTMC, confirmed to the unifocal and unilateral lobe and no evidence of PTC in the contralateral lobe by preoperative US or FNAB at Pusan National University Hospital. The FNAB to diagnose thyroid malignancy was mainly performed in the nodule with ultrasonographic features for suspicious thyroid malignancy such as hypoechogenicity or markedly hypoechogenicity, ill-defined margin, presence of calcification and taller than wide shape. Two surgeons had performed thyroid surgeries during this period. A bilateral central compartment neck dissection was routinely performed during the total thyroidectomy. Of the 428 patients, three patients underwent unilateral lobectomy so they were excluded. In addition, 32 patients were excluded due to following reasons: patients with other coexisting pathologic findings (n = 4; Hürthle cell adenoma [n = 2], follicular adenoma [n = 1], and follicular carcinoma [n = 1]); patients with previous thyroid drug history (n = 13) or unavailable preoperative thyroid stimulating hormone (TSH) (n = 15), to establish the effect of TSH on multifocal disease of PTC. Finally 393 patients with unilateral PTMC preoperatively confirmed were available for this study. Central neck dissection was performed in 390 patients (99.2%) of the patients finally enrolled.
The TSH level was checked within 3 months before surgery and was determined by immunoradiometric assay (Coat-ACount, TSH IRMA; Diagnostic Products Co., Los Angeles, CA, USA). The analytical sensitivities of the assay for TSH were 0.03 mIU/L and the intra-assay coefficients of variation ranged 1.9-5.8%. Normal reference ranges for TSH were 0.4-5.0 mL/L. Pathologic Hashimoto's thyroiditis was defined as the presence of diffuse plasma and lymphocytic cell infiltration, oxyphilic cells, the formation of lymphoid follicles, and reactive germinal centers. However, a peritumor inflammatory response was not considered Hashimoto's thyroiditis. The pathologic specimens after total thyroidectomy were routinely sectioned every 3 mm and were stained with hematoxylin and eosin for histopathologic examination. Multifocal disease was defined as more than one tumor focus in the ipsilateral or contralateral lobe of the primary tumor.
Informed consent was obtained from each participant at the time of surgery. This retrospective review protocol was approved by the Institutional Review Board at Pusan National University Hospital.
Statistical analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). All data are expressed as mean ± SD. Independent two-sample t-test was used to compare two independent groups. Pearson's χ2 test was performed to analyze categorical data as appropriate. Factors related to incidental contralateral carcinoma were analyzed using multivariate logistic regression according to the procedure "Enter." Multivariate model for incidental contralateral carcinoma was adjusted for age, sex, preoperative TSH level, tumor size, extrathyroid extension, lymphvascular invasion, ipsilateral multifocality, coexsisting Hashimoto's thyroiditis, and central lymph node (LN) metastasis as independent variables. Predicted probability of incidental contralateral carcinoma was assessed by logistic regression and calculated by the following formula:
Predictive probability = 1 / {1 + Exp [-(a0 + a1X1 + a2X2 + a3X3 + a4X4)]},
where Exp represents exponent, a0 is the intercept estimate, a1-4 is the estimate of clinicopathologic variables, and X is the point of clinicopathologic variables. The cut-off values of the point score for predicting incidental contralateral carcinoma was calculated using the receiver operating characteristics (ROC) curve. Subsequently, the sensitivity and specificity of this cut-off value were estimated. A P value of less than 0.05 was considered statistically significant.
The cohort included 53 men and 340 women with ages ranging 20-77 (mean age, 48.0 ± 10.7 years). The mean tumor size was 0.64 ± 0.23 cm in the patients with PTMC. The pathological extrathyroid extension, LN metastasis, and lymphovascular invasion was found in 44.8%, 40.7%, and 1.0% of the analyzed patients, respectively. With regard to LN metastasis, central LN involvement comprised 38.9% (n = 153 of 393), whereas lateral LN involvement comprised 9.7% (n = 38 of 354) of the total patients. No subject was initially diagnosed with distant metastasis. Of the 393 cohort cases, 116 patients (29.3%) had multifocality on tissue pathology. According to the American Joint Committee on Cancer/Union Internationale Contre le Cancer pathologic tumor-node-metastasis classification, there were 218 patients with stage I (55.5%), 150 with stage III (38.2%), and 25 with stage IV disease (6.3%).
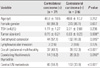
The clinical and pathologic parameters of this study cohort are summarized in Table 1; the patients were divided into those with contralateral carcinoma and those without contralateral carcinoma. Seventy-seven patients (19.6%) had incidental papillary carcinoma in the contralateral lobe. Higher prevalence in extrathyroid extension, occult ipsilateral carcinoma, pathologic Hashimoto's thyroiditis and central LN metastasis was noted compared to those without contralateral carcinoma. The mean tumor size was also increased in the patients with contralateral carcinoma (0.70 ± 0.21 vs. 0.63 ± 0.23 without contralateral carcinoma, P = 0.008). There were no differences in age, gender, preoperative TSH level and lymphovascular invasion between 2 groups.
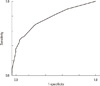
Multivariate logistic regression showed that extrathyroid extension (P = 0.049), occult ipsilateral carcinoma (P < 0.001), pathologic Hashimoto's thyroiditis (P = 0.038), and central LN metastasis (P = 0.002) were predictive for the incidental contralateral carcinoma (Table 2). Age, gender, size, and lymphovascular invasion were not associated with the presence of incidental carcinoma in contralateral lobe. Four clinicopathological parameters (extrathyroid extension, occult ipsilateral multifocality, coexisting Hashimoto's thyroiditis, and central LN metastasis), selected by logistic regression analysis, were used to evaluate the risk of incidental contralateral carcinoma and the estimate and point of each characteristic are shown in Table 3. We constructed ROC curves using these data (Fig. 1). The integrated ROC curve expressed an important sensitivity (67.5%), specificity (73.1%), and area under the curve (0.759). The predictive probability of incidental contralateral metastasis at this point was 0.31.
In this study, the operation method such as total thyroidectomy and central neck dissection were routinely performed in the same manner in most PTMC during study period. Throughout the homogenous study patients, we could derive the result that patients who had multifocal tumor in the ipsilateral lobe, coexisting Hashimoto's thyroiditis, extrathyroid extension of primary tumor and central LN metastasis have the possibility of having additional contralateral cancer.
The reported rates of contralateral PTC discovered in completion thyroidectomy or total thyroidectomy specimens ranges 13-56% [13,14]. For PTMC, up to 40% of patients have been reported to have contralateral carcinoma at the time of histological review, but these incidence show a considerable difference according to study population [14,15]. In our results, 19.6% of PTMC had contralateral carcinoma and this incidence is consistent with previous study restricted to those with preoperatively unilateral confined PTMC [16].
Multifocality is defined as more than one cancerous lesion can be located in the ipsilateral lobe only. Some previous studies reported similar findings to our study that ipsilateral multifocal disease was the predictive factor for contralateral cancer in PTMC [16]. But the relation between multifocality and LN metastasis or recurrence is controversial. Several studies reported that multifocal disease was significant factors for recurrence in PTC [15]. But other studies reported that there was no significant association between multifocality and LN metastasis or recurrence [17]. One explanation for this observation is that multifocality most often is the result of the development of multiple independent tumors and not a manifestation of intraglandular dissemination, as demonstrated by recent molecular investigations of multifocal PTC [17-20]. Each of the different microtumors seems to have the limited growth potential. But to evaluate the prognostic effect of multifocality, it is considered that the other further long-term studies may be necessary.
In the previous reports, other multiple factors have been shown to predict the contralateral cancer. Positive LN metastasis at the initial operation had been associated with PTC in remaining lobe [21,22]. In addition, the infiltrations of thyroid capsule have been linked to bilateral PTC [22]. But these reported were conducted from PTC. Our results for PTMC are consistent with these reports, and extrathyroid extension and central LN metastasis are predictive factors for contralateral cancer. In addition, the strengths of this study different from similar studies are that this study had more large number of patients. The operations were performed in the same manner such as routine total thyroidectomy and central LN dissection during short term period. Thus, more accurate prevalence of incidental contralateral carcinoma could be achieved and more reliable results were acquired regarding the predictive factors for contralateral tumors.
Interestingly, in our study the presence of Hashimoto's thyroiditis was also a significant predictive factor for the presence of contralateral PTC. Patients with Hashimoto's thyroiditis are believed to be at higher risk for PTC compared with patients without Hashimoto's thyroiditis [23]. A few previous reports have shown that the cases of PTC coexisted with Hashimoto's thyroiditis are more multicentric than those without Hashimoto's thyroiditis [24]. And Kim et al. [25] reported that multifocality and bilaterality are more frequent with the coexistence of Hashimoto's thyroiditis and PTC including PTMC, consistent with our results. The pathogenesis and the prognosis of the coexistence of PTC and Hashimoto's thyroiditis remain controversial. But Hashimoto's thyroiditis might represent the host immune response to preexisting PTC; PTC might be induced or triggered by preexisting Hashimoto's thyroiditis, and a common mechanism, such as imbalance between apoptotic/antiapoptotic pathways, may be involved in the two diseases [26]. Previous studies have reported that chronic inflammation responses such as those associated with autoimmune thyroiditis might act as carcinogens [27] or rearranged in transformation/PTC oncogene that is known to be highly specific to PTC might be expressed in Hashimoto's thyroiditis [28]. Chronic inflammatory change may occur in the whole thyroid gland with multifocal foci, so increase the incidence of multifocality and contralateral cancer.
In this study, the scores of each clinical variable for predicted probability of contralateral carcinoma were selected by logistic regression analysis. Findings suggesting absence of contralateral carcinoma were scored as 0, while those indicating contralateral carcinoma were scored as 1. Using this scoring system from perioperative and/or postoperative clinicopathological factors, we could recommend completion thyroidectomy due to high probability of incidental contralateral carcinoma if someone underwent prior lobectomy has high scoring point, although this score system exhibited relatively fair diagnostic accuracy.
The limitations of this study are that it was not based on longitudinal observations but was conducted with a cross-sectional design. Moreover, even though multifocality in the ipsilateral lobe, coexisting Hashimoto's thyroiditis, extrathyroid extension of primary tumor and central LN metastasis have the possibility of having additional contralateral cancer, its effect in the overall prognostic factors such as tumor recurrence and survival has not yet been determined. The second, the predictive factors associated with incidental contralateral carcinoma in this study could be detected retrospectively after ipsilateral lobectomy and central neck dissection. Thus, it is considered to have more clinically potential meaning to find out preoperatively the predictive factors related to contralateral carcinoma. The third, the patients of this study were mainly performed US to diagnose for PTC but not to revaluate tumor staging preoperatively. Thus, we cannot assess which preoperative US characteristics incidental papillary carcinoma of this study did have and cannot convince that multifocal disease of our study absolutely was incidental papillary carcinoma.
In conclusion, multifocality in the ipsilateral lobe, lymph nodule metastasis, extrathyroid extension, and coexisting Hashimoto's thyroiditis is associated with the presence of incidental contralateral cancer. So, if these factors are found by perioperative and/or postoperative evaluation, total thyroidectomy or completion thyroidectomy is necessary for the treatment of PTMC.
Figures and Tables
Fig. 1
Receiver-operating characteristics curves for point score associated with incidental contralateral carcinoma.
References
1. Hedinger C, Williams ED, Sobin LH. The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 1989. 63:908–911.
2. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006. 295:2164–2167.
3. Leenhardt L, Grosclaude P, Chérié-Challine L. Thyroid Cancer Committee. Increased incidence of thyroid carcinoma in france: a true epidemic or thyroid nodule management effects? Report from the French Thyroid Cancer Committee. Thyroid. 2004. 14:1056–1060.
4. Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1,779 patients surgically treated at one institution during 1940 through 1989. Surgery. 1993. 114:1050–1057.
5. Sugitani I, Fujimoto Y. Symptomatic versus asymptomatic papillary thyroid microcarcinoma: a retrospective analysis of surgical outcome and prognostic factors. Endocr J. 1999. 46:209–216.
6. Hazard JB. Small papillary carcinoma of the thyroid. A study with special reference to so-called nonencapsulated sclerosing tumor. Lab Invest. 1960. 9:86–97.
7. Hubert JP Jr, Kiernan PD, Beahrs OH, McConahey WM, Woolner LB. Occult papillary carcinoma of the thyroid. Arch Surg. 1980. 115:394–398.
8. Strate SM, Lee EL, Childers JH. Occult papillary carcinoma of the thyroid with distant metastases. Cancer. 1984. 54:1093–1100.
9. Shindo M, Wu JC, Park EE, Tanzella F. The importance of central compartment elective lymph node excision in the staging and treatment of papillary thyroid cancer. Arch Otolaryngol Head Neck Surg. 2006. 132:650–654.
10. Ito Y, Uruno T, Nakano K, Takamura Y, Miya A, Kobayashi K, Yokozawa T, Matsuzuka F, Kuma S, Kuma K, Miyauchi A. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid. 2003. 13:381–387.
11. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009. 19:1167–1214.
12. Grigsby PW, Reddy RM, Moley JF, Hall BL. Contralateral papillary thyroid cancer at completion thyroidectomy has no impact on recurrence or survival after radioiodine treatment. Surgery. 2006. 140:1043–1047.
13. Schonberger J, Marienhagen J, Agha A, Rozeboom S, Bachmeier E, Schlitt H, Eilles C. Papillary microcarcinoma and papillary cancer of the thyroid <or=1 cm: modified definition of the WHO and the therapeutic dilemma. Nuklearmedizin. 2007. 46:115–120.
14. Pasieka JL, Thompson NW, McLeod MK, Burney RE, Macha M. The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg. 1992. 16:711–716.
15. Chow SM, Law SC, Chan JK, Au SK, Yau S, Lau WH. Papillary microcarcinoma of the thyroid-prognostic significance of lymph node metastasis and multifocality. Cancer. 2003. 98:31–40.
16. Koo BS, Lim HS, Lim YC, Yoon YH, Kim YM, Park YH, Rha KS. Occult contralateral carcinoma in patients with unilateral papillary thyroid microcarcinoma. Ann Surg Oncol. 2010. 17:1101–1105.
17. Neuhold N, Schultheis A, Hermann M, Krotla G, Koperek O, Birner P. Incidental papillary microcarcinoma of the thyroid: further evidence of a very low malignant potential: a retrospective clinicopathological study with up to 30 years of follow-up. Ann Surg Oncol. 2011. 18:3430–3436.
18. Sugg SL, Ezzat S, Rosen IB, Freeman JL, Asa SL. Distinct multiple RET/PTC gene rearrangements in multifocal papillary thyroid neoplasia. J Clin Endocrinol Metab. 1998. 83:4116–4122.
19. Lin X, Finkelstein SD, Zhu B, Silverman JF. Molecular analysis of multifocal papillary thyroid carcinoma. J Mol Endocrinol. 2008. 41:195–203.
20. Bansal M, Mantha G, Nikiforov YE. Molecular and histopathological features of multifocal papillary thyroid carcinomas. Mod Pathol. 2010. 23:Suppl 1. 126A–133A.
21. Pacini F, Elisei R, Capezzone M, Miccoli P, Molinaro E, Basolo F, Agate L, Bottici V, Raffaelli M, Pinchera A. Contralateral papillary thyroid cancer is frequent at completion thyroidectomy with no difference in low- and high-risk patients. Thyroid. 2001. 11:877–881.
22. Miccoli P, Minuto MN, Ugolini C, Panicucci E, Berti P, Massi M, Basolo F. Intrathyroidal differentiated thyroid carcinoma: tumor size-based surgical concepts. World J Surg. 2007. 31:888–894.
23. Holm LE, Blomgren H, Lowhagen T. Cancer risks in patients with chronic lymphocytic thyroiditis. N Engl J Med. 1985. 312:601–604.
24. Kim SS, Lee BJ, Lee JC, Kim SJ, Jeon YK, Kim MR, Huh JE, Mok JY, Kim BH, Kim YK, Kim IJ. Coexistence of Hashimoto's thyroiditis with papillary thyroid carcinoma: the influence of lymph node metastasis. Head Neck. 2011. 33:1272–1277.
25. Kim HS, Choi YJ, Yun JS. Features of papillary thyroid microcarcinoma in the presence and absence of lymphocytic thyroiditis. Endocr Pathol. 2010. 21:149–153.
26. Antonaci A, Consorti F, Mardente S, Giovannone G. Clinical and biological relationship between chronic lymphocytic thyroiditis and papillary thyroid carcinoma. Oncol Res. 2009. 17:495–503.
27. Cornetta AJ, Russell JP, Cunnane M, Keane WM, Rothstein JL. Cyclooxygenase-2 expression in human thyroid carcinoma and Hashimoto's thyroiditis. Laryngoscope. 2002. 112:238–242.
28. Wirtschafter A, Schmidt R, Rosen D, Kundu N, Santoro M, Fusco A, Multhaupt H, Atkins JP, Rosen MR, Keane WM, Rothstein JL. Expression of the RET/PTC fusion gene as a marker for papillary carcinoma in Hashimoto's thyroiditis. Laryngoscope. 1997. 107:95–100.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download