Abstract
Background
Langerhans cell histiocytosis (LCH) is a rare disease that involves a clonal proliferation of Langerhans cells. LCH has a predilection for hypothalamo-pituitary axis (HPA) dysfunction, and this leads to diabetes insipidus (DI) and/or anterior pituitary dysfunction. Here, we describe the endocrine dysfunction and clinical characteristics of adult patients with LCH and we analyzed the differences between an adult-onset type and a childhood-onset type.
Methods
The data was obtained from a retrospective chart review of the patients with LCH that involved the HPA and who attended Seoul National University Hospital. The patients were classified into the adult-onset type (age at the time of diagnosis ≥ 16) and the childhood-onset type (age at the time of diagnosis ≤ 15).
Results
Ten patients (9 males and 1 female) were diagnosed with LCH involving the HPA. Five patients were classified as an adultonset type and the other five patients were classified as a childhood-onset type. The median follow-up duration was 6 (3-12) years for the adult-onset type and 16 (15-22) years for the childhood-onset type. All the patients presented with DI as the initial manifestation of HPA involvement. Four adult-onset patients and three childhood-onset patients had a multi-system disease. Panhypopituitarism developed in three adult-onset patients and in one childhood-onset patient. The pituitary lesion of the three adult-onset patients had spread to the brain during the follow-up duration. In contrast, the pituitary lesion of the other two adult-onset patients without panhypopituitarism and all the childhood-onset patients had not changed.
Figures and Tables
Fig. 1
Langerhans cell histiocytosis of the mastoid in a 52-year old man. A. This shows the typical morphology of an inflammatory infiltrate including eosinophils and histiocyte-like mononuclear cells having abundant amphophilic cytoplasm and grooved nuclei (H&E staining, × 400). B. Langerhans cells disclose strong immunoreactivity for S-100 (immunohistochemistry, × 200).
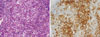
Fig. 2
Different prognosis of pituitary lesion (sella MRI). A. Pituitary stalk mass is seen at baseline (Patient 3). B. Pituitary stalk mass increased after 2 years (Patient 3). C. Pituitary stalk mass is seen at baseline (Patient 4). D. Pituitary stalk mass had no change after 3 years (Patient 4). E. Pituitary stalk thickening is seen at baseline (Patient 5). F. Pituitary stalk thickening disappeared after 12 years (Patient 5).

References
1. Enriquez P, Dahlin DC, Hayles AB, Henderson ED. Histiocytosis X: a clinical study. Mayo Clin Proc. 1967. 42:88–99.
2. Nezelof C, Frileux-Herbet F, Cronier-Sachot J. Disseminated histiocytosis X: analysis of prognostic factors based on a retrospective study of 50 cases. Cancer. 1979. 44:1824–1838.
3. Arceci RJ, Brenner MK, Pritchard J. Controversies and new approaches to treatment of Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998. 12:339–357.
4. Willman CL, Busque L, Griffith BB, Favara BE, McClain KL, Duncan MH, Gilliland DG. Langerhans'-cell histiocytosis (histiocytosis X)--a clonal proliferative disease. N Engl J Med. 1994. 331:154–160.
5. Favara BE, Feller AC, Pauli M, Jaffe ES, Weiss LM, Arico M, Bucsky P, Egeler RM, Elinder G, Gadner H, Gresik M, Henter JI, Imashuku S, Janka-Schaub G, Jaffe R, Ladisch S, Nezelof C, Pritchard J. The WHO Committee On Histiocytic/Reticulum Cell Proliferations. Reclassification Working Group of the Histiocyte Society. Contemporary classification of histiocytic disorders. Med Pediatr Oncol. 1997. 29:157–166.
6. Hicks J, Flaitz CM. Langerhans cell histiocytosis: current insights in a molecular age with emphasis on clinical oral and maxillofacial pathology practice. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 100:S42–S66.
7. Lahey E. Histiocytosis x--an analysis of prognostic factors. J Pediatr. 1975. 87:184–189.
8. Arico M, Egeler RM. Clinical aspects of Langerhans cell histiocytosis. Hematol Oncol Clin North Am. 1998. 12:247–258.
9. Dunger DB, Broadbent V, Yeoman E, Seckl JR, Lightman SL, Grant DB, Pritchard J. The frequency and natural history of diabetes insipidus in children with Langerhans-cell histiocytosis. N Engl J Med. 1989. 321:1157–1162.
10. Malpas JS. Langerhans cell histiocytosis in adults. Hematol Oncol Clin North Am. 1998. 12:259–268.
11. Arico M, Girschikofsky M, Genereau T, Klersy C, McClain K, Grois N, Emile JF, Lukina E, De Juli E, Danesino C. Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society. Eur J Cancer. 2003. 39:2341–2348.
12. Kaltsas GA, Powles TB, Evanson J, Plowman PN, Drinkwater JE, Jenkins PJ, Monson JP, Besser GM, Grossman AB. Hypothalamo-pituitary abnormalities in adult patients with langerhans cell histiocytosis: clinical, endocrinological, and radiological features and response to treatment. J Clin Endocrinol Metab. 2000. 85:1370–1376.
13. Kim BC, Lee MY, Kim YK, Lee OJ, Koong SS, Oh TK. A case of Langerhans cell histiocytosis presented with central diabetes insipidus. J Korean Soc Endocrinol. 2005. 20:513–518.
14. Kim CK, Ahn KJ, Jung JH, Koh EM, Lee MK, Lee MS, Min YK, Jung MP, Kim KW. A case of diabetes insipidus with Langerhans cell histiocytosis in adult. J Korean Soc Endocrinol. 1996. 11:330–335.
15. Islinger RB, Kuklo TR, Owens BD, Horan PJ, Choma TJ, Murphey MD, Temple HT. Langerhans' cell histiocytosis in patients older than 21 years. Clin Orthop Relat Res. 2000. 231–235.
16. Makras P, Alexandraki KI, Chrousos GP, Grossman AB, Kaltsas GA. Endocrine manifestations in Langerhans cell histiocytosis. Trends Endocrinol Metab. 2007. 18:252–257.
17. Baumgartner I, von Hochstetter A, Baumert B, Luetolf U, Follath F. Langerhans'-cell histiocytosis in adults. Med Pediatr Oncol. 1997. 28:9–14.
18. Maghnie M, Cosi G, Genovese E, Manca-Bitti ML, Cohen A, Zecca S, Tinelli C, Gallucci M, Bernasconi S, Boscherini B, Severi F, Arico M. Central diabetes insipidus in children and young adults. N Engl J Med. 2000. 343:998–1007.
19. Nanduri VR, Bareille P, Pritchard J, Stanhope R. Growth and endocrine disorders in multisystem Langerhans' cell histiocytosis. Clin Endocrinol (Oxf). 2000. 53:509–515.
20. Makras P, Papadogias D, Kontogeorgos G, Piaditis G, Kaltsas GA. Spontaneous gonadotrophin deficiency recovery in an adult patient with Langerhans cell histiocytosis (LCH). Pituitary. 2005. 8:169–174.
21. Satter EK, High WA. Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society. Pediatr Dermatol. 2008. 25:291–295.
22. Gadner H, Grois N, Arico M, Broadbent V, Ceci A, Jakobson A, Komp D, Michaelis J, Nicholson S, Potschger U, Pritchard J, Ladisch S. A randomized trial of treatment for multisystem Langerhans' cell histiocytosis. J Pediatr. 2001. 138:728–734.
23. Amato MC, Elias LL, Elias J, Santos AC, Bellucci AD, Moreira AC, De Castro M. Endocrine disorders in pediatric - onset Langerhans Cell Histiocytosis. Horm Metab Res. 2006. 38:746–751.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download