Abstract
A 39-year-old woman presented with a 20 day history of recurrent hypoosmolar hyponatremia. Because her volume status seemed to be normal, the most suspected causes of her hyponatremia were adrenal insufficiency and hypothyroidism. Endocrinologic examination, including a combined pituitary function test, showed TSH and ACTH deficiency without GH deficiency, and hyperprolactinemia was also present. Sella MRI showed a pituitary mass, stalk thickening and loss of the normal neurohypophysial hyperintense signal on the T1 weighted image. Pathologic exam demonstrated granulomatous lesions and Langhans' multinucleated giant cells with inflammatory cell infiltration. After high dose methylprednisolone pulse therapy (1 g/day for 3 days) with subsequent prednisolone and levothyoxine replacement, there was no more recurrence of the hyponatremia. The sella MRI on the 6th month showed decreased mass size, narrowed stalk thickening and the reappearance of the normal neurohyphophysial hyperintense signal. She is currently in a good general condition and is receiving hormone replacement therapy.
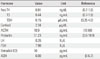
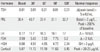
Figures and Tables
 | Fig. 1(A, B) T1-wieghted image of the sella MRI shows homogenously contrast-enhanced soft tissue mass with enlarged pituitary stalk (arrows and arrowheads, respectively). Notice the non-visualization of T1-high signal intensity of the neurohypophysis. (C, D) Follow up MRI of 6 month after High Dose Methylprednisolone Pulse Therapy and prednosolone replacement: Notice the decreased size of remained pituitary mass and improved pituitary stalk thickening (arrows and arrowheads, respectively) with faintly reappeared hyperintense neurohypophysial signal (see the boxed area on right upper part in C). |
 | Fig. 2(A, B) The histologic finding of the inflammatory pituitary tissue. Notice a granulomatous lesion (arrows on A) and Langhans' multinucleated giant cell (arrows on B) with lymphocyte infiltration (H&E stain, × 200: A, × 400: B). |
References
1. Caturegli P, Newschaffer C, Olivi A, Pomper MG, Burger PC, Rose NR. Autoimmune hypophysitis. Endocr Rev. 2005. 26:599–614.
2. Gutenberg A, Hans V, Puchner MJ, Kreutzer J, Brück W, Caturegli P, Buchfelder M. Primary hypophysitis: clinical-pathological correlations. Eur J Endocrinol. 2006. 155:101–107.
3. Lee CI, Chung YG, Kim SD, Lee HK. Idiopathic granulomatous hypophysitis. J Korean Neurosurg Soc. 2003. 34:386–388.
4. Shi J, Zhang JM, Wu Q, Chen G, Zhang H, Bo WL. Granulomatous hypophysitis: two case reports and literature review. J Zhejiang Univ Sci B. 2009. 10:552–558.
5. Yamagami K, Yoshioka K, Sakai H, Fukumoto M, Yamakita T, Hosoi M, Ishii T, Sato T, Tanaka S, Fujii S. Treatment of lymphocytic hypophysitis by high-dose methylprednisolone pulse therapy. Intern Med. 2003. 42:168–173.
6. Jo YS, Lee HJ, Rha SY, Hong WJ, Song CJ, Kim YK, Ro HK. Lymphocytic hypophysitis with diabetes inspidus: improvement by methylprednisolone pulse therapy. Korean J Intern Med. 2004. 19:189–192.
7. Cho GY, Hahm JR, Kim JH, Kang TW, Chung IK, Yang TY, Chung JH, Min YK, Lee MS, Lee MK, Se YL, Kim KW. A case of lymphocytic infundibuloneurohypophysitis presenting as central diabetes insipidus and nodular mass on neurohypophysis. Korean J Med. 2001. 61:168–172.
8. Nagi S, Megdiche H, Nouira K, Bouraoui S, Mekni A, Jemli C, Sebaï R, Zitouna M, Touibi S. Idiopathic granulomatous hypophysitis: clinical appearance and imaging. J Neuroradiol. 2002. 29:43–48.
9. Gutenberg A, Larsen J, Lupi I, Rohde V, Caturegli P. A radiologic score to distinguish autoimmune hypophysitis from nonsecreting pituitary adenoma preoperatively. Am J Neuroradiol. 2009. 30:1766–1772.
10. Kim YI, Jeon JS, Kim YJ, Park SW, Byun YH, Lee JY, Kang HI. A case of lymphocytic hypophysitis associated with Rathke's cleft cyst. Korean J Med. 2005. 69:565–570.
11. Cheung CC, Ezzat S, Smyth HS, Asa SL. The spectrum and significance of primary hypophysitis. J Clin Endocrinol Metab. 2001. 86:1048–1053.
12. Lecube A, Francisco G, Rodríguez D, Ortega A, Codina A, Hernández C, Simó R. Lymphocytic hypophysitis successfully treated with azathioprine: first case report. J Neurol Neurosurg Psychiatry. 2003. 74:1581–1583.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download