INTRODUCTION
With advances in insulin preparations and the use of recombinant human insulin and insulin analogues, there has been a marked decrease in the prevalence and titer of anti-insulin antibodies in insulin-treated patients. Although about 40% of diabetic patients who inject human insulin have insulin antibodies, these antibodies rarely affect glycemic control significantly [1,2]. Diabetic ketoacidosis (DKA) is characterized by hyperglycemia, ketone bodies, and metabolic acidosis, and it can be initiated by a deficit in insulin levels [3]. In contrast, the hypoglycemia in diabetic patients - the most common type of hypoglycemia - usually develops due to an excess of therapeutic insulin [4]. Thus, the clinical manifestations of hypoglycemia are usually not observed in diabetic patients after insulin is discontinued. Hypoglycemia and DKA may exist along an extreme continuum of circulating insulin concentrations and glycemic control.
We describe a rare case of spontaneous hypoglycemia due to insulin antibody after improvement of DKA in a patient with type 2 diabetes mellitus, who had been treated with human insulin.
CASE REPORT
A 71-year-old woman was admitted to our hospital because of vomiting and dyspnea. Diabetes mellitus had been detected 3 years earlier at another facility. She was initially treated with metformin and glimepiride, but she took her medication irregularly. Beginning 2 month before admission to our hospital, she was being treated with 1,500 mg metformin, 2 mg glimepiride and intermediate acting insulin, Humulin N®. However, she had poor compliance and irregular insulin injection. She had an unremarkable medical history other than diabetes mellitus. She had no history of therapy with sulfhydryl-containing drugs. She did not smoke or drink and had no family history of endocrine disorders or diabetes.
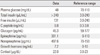
Upon admission, her mental status was drowsy. She was 152.5 cm tall and weighed 58 kg with body mass index of 24.9 kg/m2. She had a body temperature of 36.5℃, a heart rate of 100 beats/min, and a blood pressure of 140/90 mmHg. Physical examination was normal, except for signs of dehydration and Kussmaul's respiration. Chest films were also normal. Laboratory data were consistent with DKA; her plasma glucose was 570 mg/dL, her urinalysis showed 3+ ketones, and she had metabolic acidosis; arterial blood gas analysis showed pH 7.01, PCO2 9.9 mmHg, and HCO3- 2.5 mmol/L. The white blood cell count showed mild leukocytosis at 12,500/mm3. Blood chemistry testing revealed the following: sodium 128 mmol/L, potassium 4.3 mmol/L, chloride 110 mmol/L, creatinine 1.0 mg/dL, lactate 0.9 mmol/L, C-reactive protein 1.2 mg/dL, and HbA1c 8.7%. There were no evidences of infection or infarction, which can precipitate DKA. After insulin and fluid therapy, the glucose level decreased, and the acidosis resolved. Intravenous insulin therapy was changed to subcutaneous insulin therapy with a long-acting insulin analogue glargine, and the patient began to experience hypoglycemia (Fig. 1). The hypoglycemic attacks continued even after discontinuation of the insulin injections, and the patient's daily glucose profile indicated hypoglycemia at dawn or in the early morning, as well as postprandial hyperglycemia, every day. Table 1 show the hormone responses, when hypoglycemic symptoms developed. Insulin antibodies (radioimmunoassay method: Packard, USA) were significantly increased (84.7%; reference range < 7%). On oral glucose tolerance testing, the plasma glucose level had a characteristic diabetic pattern (Table 2). Computed tomography of the abdomen revealed no evidence of a pancreatic tumor. These findings suggested that the hyperglycemic crisis and hypoglycemic attacks might be due to insulin antibodies. Anti-glutamic acid decaroxylase antibody, islet cell antibody, anti-insulin receptor antibody, anti-nuclear antibody, and anti-microsome antibody were all negative.
The patient was treated with α-glucosidase inhibitor in addition to frequent, small, low carbohydrate meals. However, hypoglycemia continued to occur in the morning. 30 mg prednisolone per day was administered to treat hypoglycemia and to suppress production of the autoimmune antibodies. As neither insulin nor insulin secretagogues could be administered for glycemic control, the patient was treated with α-glucosidase inhibitor and prednisolone. The antibody titer decreased significantly after steroid therapy. The patient experienced no further episodes of DKA and hypoglycemia.
DISCUSSION
Ever since Berson et al. [5] reported that the insulin inhibitory factors present in the sera of insulin-treated diabetic patients are immunoglobulins, there have been many studies evaluating the characteristics of insulin antibodies. The antibody responses to foreign proteins are generated from the uptake by dendritic antigen-presenting cells found in insulin delivery sites such as subcutaneous space [6]. Differences in the amino acid sequence between a protein and a self-protein will strengthen the inherent immunogenicity. Thus, the administration of animal-derived insulin might cause greater insulin antibody responses than that of human insulin, and bovine-and porcine-derived insulin is known to induce insulin antibodies in more than 95% of diabetic patients [1]. However, with the use of recombinant human insulin and insulin analogues, there has been a marked decrease in the prevalence of insulin antibody formation in such patients; about 40% of diabetic patients with injection of human insulin may have insulin antibodies [1,2]. The rapid-acting insulin analog lispro may result in development of insulin antibodies, with no significant differences between lispro and human insulin [7]. However, Raskin et al. [8] reported that insulin aspart exhibited robust antibody responses in some patients. Pieber et al. [9] reported that long-acting insulin analogue glargine did not show increased insulin antibody levels. In the present case, the patient had a history of exposure to human insulin during the two months prior to the development of DKA. It has been reported that antibody formation may be induced by as few as four subcutaneous injections of human insulin [10]. However, there seems to be no significant relationship between insulin dose and antibody formation [11].
The several factors such as genetic factors, insulin purity, insulin formulation, and insulin aggregation may influence the generation of insulin antibodies to exogenous insulin [1]. The HLA-DR7 allele is related to the presence of insulin antibodies after insulin therapy. Soluble form is less immunogenic than depot preparations, and acid preparations are more immunogenic than neutral ones. Insulin aggregation may also affect immunogenic potential due to longer residence of aggregates at the injection site and the easy uptake by antigen presenting cells.
The development of insulin antibodies may alter insulin pharmacokinetics [12]. The insulin-antibody interaction is reversible and dependent on the affinity and capacity of the antibody to bind insulin. Thus, the amount of insulin bound by an antibody depends on the insulin concentration, antibody affinity, and antibody concentration. Some studies have reported that the insulin antibodies induced in response to insulin therapy are polyclonal IgG with kappa and lambda light chains and two classes of insulin-binding sites characterized by high affinity/low capacity and low affinity/high capacity [13]. Insulin antibodies with low affinity and high binding capacity seem more likely to cause hypoglycemia than antibodies with high affinity and low capacity do [14,15].
To the best of our knowledge, no investigator has previously reported that insulin antibody formation in human insulin-exposed diabetes mellitus patients is associated with DKA and subsequent hypoglycemia. Patients with elevated levels of insulin antibodies exhibit a reduced initial rate of rise, a delayed time to peak, and a prolonged return of plasma free insulin levels to baseline [16]. Delays in the initial increase in plasma free insulin levels may cause greater postprandial hyperglycemia because antibody-bound insulin is unavailable to tissues, but the prolongation of postprandial hyperinsulinemia may result in late hypoglycemia in patients with antibodies [16]. In the present case, the patient showed fasting hypoglycemia preceded by initial hyperglycemia in response to a meal. The patient had no significant changes in the plasma free insulin concentrations, irrespective of changes in the plasma glucose concentration. However, when spontaneous fasting hypoglycemia developed, the patient exhibited a transient rise in plasma free insulin levels suggestive of dissociation of a large amount of insulin bound to insulin antibodies. This differed from previous reports that showed a gradual rise in plasma free insulin levels in response to an oral glucose load [17,18]. Thus, insulin-antibody complexes may serve as an excessive buffer in the present case, which leads to relative insulin deficiency. This relative insulin deficit due to blocking of insulin action may be associated with the development of DKA. Additionally, decreased tissue perfusion in the setting of DKA can aggravate insulin resistance by decreasing insulin delivery to the sites of insulin-mediated glucose disposal as well as by stimulating of catecholamine and glucocorticoid secretion [3]. Thus, in the present case, the resolution of DKA and glucotoxicity may also have contributed to the development of hypoglycemia due to insulin antibodies with the improvement in insulin resistance. However, contribution of improved glucotoxicity to hypoglycemia may be trivial because as blood glucose falls into hypoglycemic range, insulin is generally suppressed in the absence of exogenous insulin and insulin secretagogues.
Insulin-antibody complex may also be associated with severe insulin resistance. The incidence of immunological insulin resistance has been reported to be about 0.1% [1]. Its clinical course may be associated with poor glycemic control, and rarely with episodes of diabetic ketoacidosis and hyperglycemic hyperosmolar coma [19]. The duration of insulin therapy before its onset is varied from less than 1 month to 15 years [19]. Treatment for immunological insulin resistance entails the switch to alternative insulin formulations and the administration of glucocorticoid to reduce production of insulin antibodies [1].
To reduce postprandial hyperglycemia and the stimulus to insulin secretion, we implemented frequent, small, low-carbohydrate meals and treated the patient with an α-glucosidase inhibitor. However, the patient continued to have hypoglycemic attacks in the early morning, though they were milder than before. The treatment of hypoglycemia caused by insulin antibodies has not been established. However, because glucocorticoid therapy has been used to lower the titer of insulin antibodies [17], we gave the patient prednisolone in combination with an α-glucosidase inhibitor to reduce postprandial glucose excretion. After glucocorticoid administration, the patient experienced no recurrence of hypoglycemic symptoms, but exhibited a decrease in the antibody titer.
The results of this case suggest that frequent hypoglycemia in diabetic patients with ketoacidosis should raise the suspicion of insulin antibody, as well as excessive insulin administration, as a cause of hypoglycemia; however, additional study is necessary to evaluate the nature of insulin antibodies with respect to extreme glycemic instability.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download