Abstract
Background
Tri-iodothyronine (T3) is the main active hormone, and 20% of this is derived from the thyroid gland and 80% is from the peripheral tissue according to 5'-monodeiodination of thyroxine (T4). In the previous studies, normal T3 levels were achieved with traditional levothyroxine (LT4) therapy alone in athyreotic patients, but there has been no data about the factors influencing peripheral conversion of LT4. The aim of this study was to determine the factor(s) influencing peripheral conversion of LT4 to T3 in athyreotic patients during LT4 replacement.
Methods
The patients who underwent total-thyroidectomy for any cause, and mostly for thyroid cancers, at Asan Medical Center between 2000 and 2008 were enrolled. The free T4, T3 and thyroid stimulating hormone (TSH) levels and age, gender, weight, height, body mass index (BMI) and the T4 dose were measured. Only patients with normal ranges of free T4 and TSH were included in the analysis.
Results
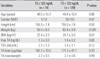
A total of 143 patients were enrolled. The mean T3, free T4 and TSH levels were 143.7 ng/dL, 1.4 ng/dL and 1.6 µU/mL, respectively. The mean weight and BMI were 62.9 kg and 24.6 kg/m2, respectively. We divided them into two groups according to the serum T3 level and we compared the characteristics of the groups. There were no differences in age, the gender distribution, the T4 dose/weight and the BMI between the low T3 group (T3 ≤ 122 ng/dL, n = 14) and the normal T3 group (T3 > 122 ng/dL, n = 129). In the low T3 group, the mean body weight was significantly lower than that of the normal T3 group (59.0 ± 6.0 vs. 63.4 ± 9.9, respectively, P = 0.025).
Conclusion
Lean body mass seems to be an important factor for determining the peripheral conversion of T4 to T3 in human. This suggest that a combination of T3/T4 is better than T4 only when we treat the patients with hypothyroidism and who have a negligible amount of functioning thyroid tissue, if they have a low lean body mass.
Figures and Tables
Fig. 1
Tri-iodothyronine and free thyroxine ratio (T3/fT4) according to the level of free T4 (n = 771). T3, tri-iodothyronine; T4, thyroxine.

Fig. 2
Body mass index (BMI) (A) and body weight (B) according to the level of tri-iodothyronine. T3, tri-iodothyronine.

References
1. Braverman LE, Ingbar SH, Sterling K. Conversion of thyroxine (T4) to triiodothyronine (T3) in athyreotic human subjects. J Clin Invest. 1970. 49:855–864.
2. Braverman LE, Vagenakis A, Downs P, Foster AE, Sterling K, Ingbar SH. Effects of replacement doses of sodium L-thyroxine on the peripheral metabolism of thyroxine and triiodothyronine in man. J Clin Invest. 1973. 52:1010–1017.
3. Nicoloff JT, Lum SM, Spencer CA, Morris R. Peripheral autoregulation of thyroxine to triiodothyronine conversion in man. Horm Metab Res Suppl. 1984. 14:74–79.
4. Escobar-Morreale HF, del Rey FE, Obregón MJ, de Escobar GM. Only the combined treatment with thyroxine and triiodothyronine ensures euthyroidism in all tissues of the thyroidectomized rat. Endocrinology. 1996. 137:2490–2502.
5. Escobar-Morreale HF, Obregón MJ, Escobar del Rey F, Morreale de Escobar G. Replacement therapy for hypothyroidism with thyroxine alone does not ensure euthyroidism in all tissues, as studied in thyroidectomized rats. J Clin Invest. 1995. 96:2828–2838.
6. Escobar-Morreale HF, Obregón MJ, Escobar del Rey F, Morreale de Escobar G. Tissue-specific patterns of changes in 3,5,3'-triiodo-L-thyronine concentrations in thyroidectomized rats infused with increasing doses of the hormone. Which are the regulatory mechanisms? Biochimie. 1999. 81:453–462.
7. Escobar-Morreale HF, Obregón MJ, Hernandez A, Escobar del Rey F, Morreale de Escobar G. Regulation of iodothyronine deiodinase activity as studied in thyroidectomized rats infused with thyroxine or triiodothyronine. Endocrinology. 1997. 138:2559–2568.
8. Bartalena L, Pinchera A. Effects of thyroxine excess on peripheral organs. Acta Med Austriaca. 1994. 21:60–65.
9. Fazio S, Palmieri EA, Lombardi G, Biondi B. Effects of thyroid hormone on the cardiovascular system. Recent Prog Horm Res. 2004. 59:31–50.
10. Sawin CT, Geller A, Wolf PA, Belanger AJ, Baker E, Bacharach P, Wilson PW, Benjamin EJ, D'Agostino RB. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med. 1994. 331:1249–1252.
11. Uzzan B, Campos J, Cucherat M, Nony P, Boissel JP, Perret GY. Effects on bone mass of long term treatment with thyroid hormones: a meta-analysis. J Clin Endocrinol Metab. 1996. 81:4278–4289.
12. England ML, Hershman JM. Serum TSH concentration as an aid to monitoring compliance with thyroid hormone therapy in hypothyroidism. Am J Med Sci. 1986. 292:264–266.
13. Franklyn JA, Black EG, Betteridge J, Sheppard MC. Comparison of second and third generation methods for measurement of serum thyrotropin in patients with overt hyperthyroidism, patients receiving thyroxine therapy, and those with nonthyroidal illness. J Clin Endocrinol Metab. 1994. 78:1368–1371.
14. Kaplan MM. Thyroid hormone therapy. What, when, and how much. Postgrad Med. 1993. 93:249–252.
15. Mandel SJ, Brent GA, Larsen PR. Levothyroxine therapy in patients with thyroid disease. Ann Intern Med. 1993. 119:492–502.
16. Rosenbaum RL, Barzel US. Levothyroxine replacement dose for primary hypothyroidism decreases with age. Ann Intern Med. 1982. 96:53–55.
17. Roti E, Minelli R, Gardini E, Braverman LE. The use and misuse of thyroid hormone. Endocr Rev. 1993. 14:401–423.
18. Sawin CT, Herman T, Molitch ME, London MH, Kramer SM. Aging and the thyroid. Decreased requirement for thyroid hormone in older hypothyroid patients. Am J Med. 1983. 75:206–209.
19. Toft AD. Thyroxine therapy. N Engl J Med. 1994. 331:174–180.
20. Woeber KA. Levothyroxine therapy and serum free thyroxine and free triiodothyronine concentrations. J Endocrinol Invest. 2002. 25:106–109.
21. Cunningham JJ, Barzel US. Lean body mass is a predictor of the daily requirement for thyroid hormone in older men and women. J Am Geriatr Soc. 1984. 32:204–207.
22. Alexander EK, Marqusee E, Lawrence J, Jarolim P, Fischer GA, Larsen PR. Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism. N Engl J Med. 2004. 351:241–249.
23. da Costa VM, Moreira DG, Rosenthal D. Thyroid function and aging: gender-related differences. J Endocrinol. 2001. 171:193–198.
24. Wu S-Y, Visser TJ. Thyroid hormone metabolism. 1994. 1st ed. Florida: CRC Press;78–80.
25. Larsen PR, Silva JE, Kaplan MM. Relationships between circulating and intracellular thyroid hormones: physiological and clinical implications. Endocr Rev. 1981. 2:87–102.
26. Santini F, Pinchera A, Marsili A, Ceccarini G, Castagna MG, Valeriano R, Giannetti M, Taddei D, Centoni R, Scartabelli G, Rago T, Mammoli C, Elisei R, Vitti P. Lean body mass is a major determinant of levothyroxine dosage in the treatment of thyroid diseases. J Clin Endocrinol Metab. 2005. 90:124–127.
27. Morgan DJ, Bray KM. Lean body mass as a predictor of drug dosage. Implications for drug therapy. Clin Pharmacokinet. 1994. 26:292–307.
28. Salvatore D, Bartha T, Harney JW, Larsen PR. Molecular biological and biochemical characterization of the human type 2 selenodeiodinase. Endocrinology. 1996. 137:3308–3315.
29. Bianco AC, Salvatore D, Gereben B, Berry MJ, Larsen PR. Biochemistry, cellular and molecular biology, and physiological roles of the iodothyronine selenodeiodinases. Endocr Rev. 2002. 23:38–89.
30. Streckfuss F, Hamann I, Schomburg L, Michaelis M, Sapin R, Klein MO, Köhrle J, Schweizer U. Hepatic deiodinase activity is dispensable for the maintenance of normal circulating thyroid hormone levels in mice. Biochem Biophys Res Commun. 2005. 337:739–745.
31. Jonklaas J, Davidson B, Bhagat S, Soldin SJ. Triiodothyronine levels in athyreotic individuals during levothyroxine therapy. JAMA. 2008. 299:769–777.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download