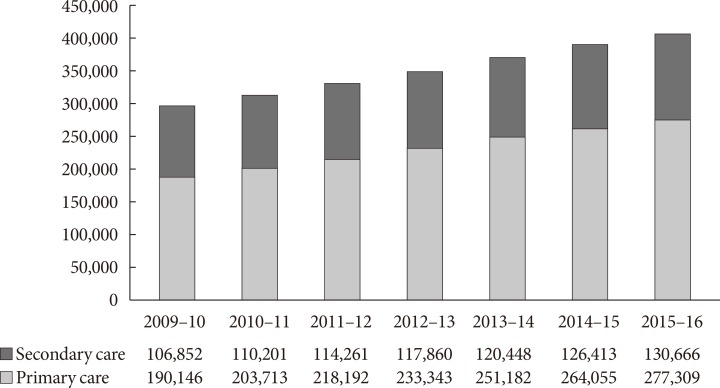
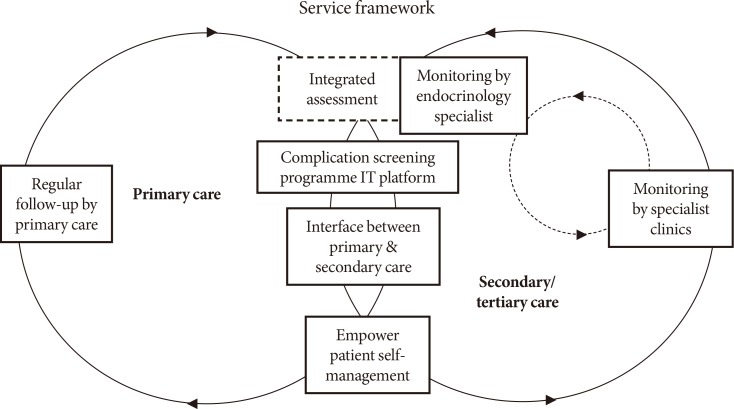
In 2009, the HA introduced a multidisciplinary RAMP-DM to improve the quality of care for patients receiving diabetic care in the GOPCs [
5]. All patients with type 2 diabetes mellitus who are independent in their activities of daily living and being followed up regularly at the GOPCs are eligible for the RAMP. Enrolled patients undergo a comprehensive risk assessment with checking of relevant clinical parameters including HbA1c, blood pressure, LDL-C, and screening for diabetes-related complications according to a standardized protocol. After the assessment, patients are classified into different risk groups according to the Joint Asia Diabetes Evaluation (JADE) criteria [
6] and are offered different management options to receive appropriate interventions and education provided by a team of multidisciplinary healthcare professionals. Low risk patients continue with the usual GOPC care; medium risk patients are given additional intervention by a nurse with special training in diabetes; and high risk/very high risk patients are reviewed by a specialist family physician for intensification. About two-thirds of the diabetic patients under the care of the GOPCs (277,309 in 2015/2016) have been enrolled.
The effect and effectiveness of the RAMP-DM has been evaluated by three prospective cohort studies. Thus, it was found that there was a significant decrease in HbA1c (−0.20%,
P<0.01), systolic blood pressure (SBP; −3.62 mm Hg,
P<0.01), 10-year cardiovascular disease (CVD) risks (total CVD risk, −2.06%,
P<0.01; coronary heart disease [CHD] risk, −1.43%,
P<0.01; stroke risk, −0.71%,
P<0.01) at 12 months in a random sample of 1,248 patients enrolled to RAMP-DM compared with an age-, sex-, and HbA1c-matched group of unenrolled 1,248 patients under the usual primary care. There was a rise in the percentage of patients reaching treatment targets of HbA1c (5.4%,
P<0.01), and SBP/diastolic blood pressure (5.77%,
P<0.01) and a lower cardiovascular events incidence (1.21% vs. 2.89%,
P=0.003) [
7]. More significantly, in another prospective cohort study of 18,188 propensity score matched RAMP-DM participants and patients receiving the usual primary care with a median follow-up of 36 months (9,094 subjects in each group), there were significantly lowered adjusted hazard ratios (HRs) in the RAMP-DM group compared with the usual care group in all-cause deaths (0.363; 95% confidence interval [CI], 0.308 to 0.428;
P<0.001); CHD (0.570; 95% CI, 0.470 to 0.691;
P<0.001); stroke (0.652; 95% CI, 0.546 to 0.780;
P<0.001); and congestive heart failure (0.598; 95% CI, 0.446 to 0.802;
P=0.001) [
8]. Further, a third study comparing RAMP-DM participants with subjects under the usual primary care (14,835 in each group) with a median follow-up of 36 months, RAMP-DM participants had a lower incidence of microvascular complications (760 vs. 935; adjusted HR, 0.73; 95% CI, 0.66 to 0.81;
P<0.001) and lower incidences of all specific microvascular complications except neuropathy (adjusted HR, 0.94; 95% CI, 0.61 to 1.45;
P=0.778). Adjusted HRs for the RAMP-DM versus control group for end stage renal disease, sight threatening diabetic retinopathy or blindness, and lower-limb ulcers or amputation were 0.40 (95% CI, 0.24 to 0.69;
P<0.001), 0.55 (95% CI, 0.39 to 0.78;
P=0.001), and 0.49 (95% CI, 0.30 to 0.80;
P=0.005), respectively [
9]. Although these are not randomized controlled trials, the careful matching, large numbers of patients and long duration of follow-up meant that a program of risk assessment and stratification followed by appropriate intervention is likely to be high effective in improving long term clinical outcomes.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download