Abstract
Background
Self-care of diabetes is an essential part for controlling the disease and improvement of quality of life in type 2 diabetes mellitus (T2DM) patients. This study aimed to analyze the associated factors of quality of life in patients with T2DM in order to design effective interventions.
Methods
This cross-sectional study was conducted on 120 T2DM patients referred to health centers of Chaldoran, West Azerbaijan Province, Iran. The quality of life's questionnaires from World Health Organization and the self-care behaviors' questionnaires were used for data collection.
Results
The mean age of patients was 46.30% and 53.30% of them were male. Among demographic variables, gender (P=0.002), age groups (P=0.007), and household monthly income (P=0.009) were significantly associated with total quality of life. Also, self-care nutrition (odds ratio [OR], 1.47; P=0.001), self-management of blood glucose control (OR, 1.29; P=0.002), and self-medication behavior (OR, 1.18; P=0.030) were identified as factors significantly associated with quality of life.
Conclusion
Self-care behaviors were significantly associated with quality of life; among them, the greatest influence was observed in self-care nutrition behavior. According to the findings of this study, appropriate interventions on self-care behaviors about nutrition can improve the quality of life for T2DM patients.
Diabetes is one of the most common metabolic disorders in the world and its prevalence has an upward trend, so that it is called as the “silent epidemic” [1]. According to the World Health Organization (WHO), the prevalence of diabetes will increase from 4% in 1995 to 5.40% in 2035, and burden of the disease will be higher in developing countries. Moreover, the number of patients in low- and middle-income countries will rise from 84 million to 228 million people [2]. According to the WHO in 2011, the prevalence of diabetes in Iranian adults was 10.30%, of which women had the bigger proportion than men [3]. In Iran, diabetes' prevalence of people older than 30 years old counts for more than 14% [4]. In addition to increased mortality, diabetes can cause decreased physical activity, has an influence on mental condition, individual, family, social, and sexual relationships [5], and chronic diseases such as cardiovascular disease, and ultimately reduce the quality of life of the patients [6]. Therefore, in order to prevent or delay the number of fatal complications associated with diabetes mellitus, serious glycemic control is required to achieve target blood glucose levels [45]. To achieve this goal, it is necessary to encourage therapeutic regimens adherence so that patients observe the medical recommendations, take their medication, change their life style, and follow the recommendations of the clinicians [7].
Quality of life literally means how to live, and in scientific definition by WHO means individual's perception of the current situation with respect to the culture and value system in which he/she lives and their relationship with the individual's goals, expectations, standards and priorities [4]. Quality of life is a subjective, multi-dimensional and dynamic factor which is the combination of cognitive factors such as satisfaction and feelings like happiness [8]. Karlsson et al. [9] suggested that in patients, broader dimensions such as the quality of life should be considered instead of indicators of mortality and morbidity. Hall et al. [10] reported that quality of life is affected by daily treatment requirements. Self-care and the ability to compromise with self-care behaviors have a direct relationship with the quality of life.
During the past decades, the main goal of controlling diabetes was shifted to improve the overall patients' quality of life [11]. Because inadequate attention to the quality of life can lead to frustration, lack of motivation to try harder, and reduced socioeconomic activities and health care [12]. By identifying relevant factors and modifiable predictors of quality of life in patients with diabetes, we can design effective interventions for better management of diabetes, in addition to improving the quality of life in these patients.
Considering the importance of the quality of life among patients with diabetes, this study aimed to investigate the associated factors of quality of life among patients with type 2 diabetes mellitus (T2DM) in Chaldoran County in 2015.
In this cross-sectional study, 120 patients with T2DM who were referred to Health Center of Chaldoran County in year 2015 were included in the study. The target population included all T2DM patients referred to the health center in the county. The statistical framework was based on the available household lists from every health centers in the county. Thus, based on the household lists, participants were randomly selected. Afterwards, the questions using a face-to-face interview were completed. Before completing the questionnaires, objectives of the study were explained to patients and informed consent form was also completed by them.
Inclusion criteria were living in Chaldoran County for at least 1 month, having medical records in the health center, age (over 30 years old), and diagnosis of T2DM in accordance with the national Iranian laboratory instructions of final diagnosis (having been suffering from T2DM [fasting blood sugar ≥126 mg/dL and 2-hour postprandial blood glucose ≥200 mg/dL] [13] for at least 2 years) of T2DM. Exclusion criteria included having other types of diabetes (type 1, gestational diabetes mellitus, other specific types [secondary diabetes]) and unwillingness to participate in the study.
Demographic data were collected by using a researcher-made form including age group (30 to 39, 40 to 49, and >50 years), educational level, marital status, job, and monthly household income. To measure the life's quality of patients, a standardized Persian version of the World Health Organization's questionnaire for quality of life (WHOQOL-BREF) was used. Validity and reliability of WHOQOL-BREF were proved in more than 40 countries and it is accepted by the scientific communities [812]. This questionnaire was also acceptable by Nejat et al. [14] in Iran in a study entitled as “Standardization of Quality of Life Questionnaire of the World Health Organization.” Cronbach's α in four dimensions of physical health (α=0.70), mental health (α=0.73), social relationships (α=0.55), and environment health (α=0.84) was approved [14]. Of 26 questions in the questionnaire, the first two questions are related to the overall assessment of quality of life; seven questions to assess the physical health domains including activity of daily living, pain and discomfort, fatigue, sleep, and rest; six questions to evaluate mental health (the condition of thinking), memory, concentration, feelings, self-esteem, and body image; three questions to investigate social, personal, and marital relationships; and eight questions to evaluate the environmental aspect of home environment, financial resources, the availability and quality of health care service and spare time. The method of scoring in this questionnaire was a five-item Likert scale. The analysis of answers to the questions three, four, and 26 were reversed; after carrying out the necessary calculations at each dimension, a score of four to 20 were obtained (the score of four represented the worst quality of life and 20 counted for the best situation). These scores can be converted to a score of 0 to 100 as well [15]. It should be noted that in this study scores range from 0 to 100 in every dimensions.
Self-care behaviors of patients contained in four dimensions (including nutrition, physical activity, medications for diabetes, and self-monitoring of blood glucose) were assessed based on adherence to the above four dimensions during last 7 days. For example, in the nutrition aspect, the patient in the last week ‘how many times adhered to the nutritional program recommended by the physicians?’ were measured using the scale of self-care activities of Toobert et al. [16] which its Persian version's validity and reliability are approved in the study of Didarloo et al. [17] (α=0.83). This rating scale ranges from 0 to 84, where a higher score indicates a better performance of self-care.
The mean±standard deviation was used to describe the normal quantitative variables; but if there was any skewness in the data, the median and interquartile range was used. The frequency (percent) was used for qualitative variables. To investigate the relationship between variables, the normality assumption of the variables in the study was assessed by the Kolmogorov-Smirnov test. To evaluate significant difference between qualitative variables, the chi-square test was used. For limitations on the observed frequency, the Fisher exact test was applied. To compare the equality of two mean values in qualitative variables and default equality of variances, the t-test exam was adopted. Analysis of variance was applied to compare the difference of means between more than two different levels. Furthermore, hierarchical linear regression method was used to predict the quality of life of patients. It was performed in two stages. In the first phase, only demographic variables and in the second phase, demographic variables along with self-care behaviors were entered into the model. P value less than 0.05 were considered as significant. The data were analyzed by statistical software SPSS version 22 (IBM Co., Armonk, NY, USA).
In total, 120 T2DM patients were participated. The mean age of study participants was 46.30±9.50 and 53.30% of them were male. All patients' educational level was below high school's diploma, and also, the majority of the patients were married (83.40%).
No significant difference was seen between males and females in demographic characteristics of educational level, marital status, job, income status, and duration of disease; however, a significant difference was observed among age groups (P=0.001) (Table 1).
Of participants, 52.50% were noted to be diagnosed of diabetes from 5 to 10 years ago. The mean of patients' overall quality of life score was 49.30±12.20. The mean scores of self-care behaviors including the self-care nutrition, self-management of blood glucose control, self-management of physical activity, and self-medication were not statistically different between male and female patients (P>0.05) (Table 2).
In terms of gender, significant differences were observed in all aspects of life's quality of the patients. Among quality of life's dimensions, there was a statistical difference only between physical health dimension and age groups (P<0.001) (Table 3). The patients' educational level was significantly associated with physical health dimension of quality of life (P=0.04), and those with higher educational levels had a better physical health (Table 3).
In terms of economic status, physical health in people with less than 313 dollars per month income level was significantly lower than in those with 313 to 470 dollars per month and more than 470 dollars per month income level (P<0.001). The mental health of married cases was significantly better than single ones (P<0.001) (Table 3).
To predict patients' quality of life, hierarchical multiple linear regression test was performed. As it can be seen in Table 4, results of the univariate analysis showed that among demographic variables, only employment was associated with the quality of life (P<0.001). Of the self-care behaviors, self-care nutrition behavior (49%), self-management of blood glucose control (37%), and self-medication behavior (19%) were predictors of the quality of life.
While the results of the multivariate analysis showed that indicators of self-care behavior, including self-care nutrition behavior (odds ratio [OR], 1.47), self-management of blood glucose control (OR, 1.29), and self-medication behavior (OR, 1.18) were predictors of quality of life in patients with T2DM (P<0.05). Among self-care behaviors, only self-management of physical activity (exercise) was not a predictor of the quality of life (P=0.985) and the strongest predictor was self-care nutrition behavior (OR, 1.47; P=0.001) (Table 4).
In the present study, gender had significant association with all dimensions of the quality of life; and variables of age, education, income, and marital status showed a significant association with physical health in patients' quality of life. Among self-care behaviors, only self-management of physical activity (exercise) was not a predictor of the quality of life (P=0.985) and the strongest predictor was self-care nutrition behavior (OR, 1.47; P=0.001).
In similar study, Mohammad pour et al. [18] reported that 80.70% of T2DM patients had good mental health. Also the study of Wang et al. [19] on T2DM patients in China, reported that the quality of life of participants was lower in mental health dimension than physical health. It seems that the lower quality of life of patients in the mental aspect depends on long-term or chronic disease and the effect of physical disorders on mental health.
A significant relationship was observed between age groups and physical health. Thus, older age groups had lower mean scores of the quality of life in physical health dimension. These findings have been confirmed in another studies, for example, Mohammad pour's study in Iran [18]. It might be the result of increased symptoms and physical limitations that goes up with age.
Patients with higher educational level had higher average score for the quality of life in physical health dimension. These findings are similar to previous study [20]. Zagozdzon et al. [21] also reported that higher education can play an important role in improvement of people's quality of life. It seems that people with higher education levels pay more attention to health care, and are looking for more health information to improve their health.
The income level was an effective factor on the patients' mental and physical health. In other words, patients that their economic situation was reported as “good” had a better quality of life in their mental and physical health. Similar to the finding of this study, Parvan et al. [22] reported that low economic status is associated with poor quality of life. Moreover, Mohammad pour et al. [18] in their study concluded that economic factors can affect the quality of life and cause a change in it.
Similar to the findings of this study, Arslantas et al. [23] reported that being married has a positive impact on the quality of life. Married people can have high quality of life because of the spouse's supporting role.
No significant association was found between employment status and quality of life (Table 4). This finding is different to result of the study conducted by Genga et al. [24] reported that having a job can improve the scores of the quality of life in physical and social domain. These inconsistent findings indicate the necessity of more precise examination of the quality of life with people's job.
The findings of this study showed that in patients with the history of disease more than 10 years, the quality of life was significantly low in terms of physical, mental, and environmental health. Therefore, it is necessary to consider the history of the disease and it's reducing impact on quality of life during patient's needs assessment and designing the training programs.
In this study, the relationship between gender and the quality of life was significant, so that the quality of life in women was lower than men. Study of Hatamloo Sadabadi et al. [25] on the quality of life in T2DM and non-diabetic patients, one possible reason for the lower quality of life in women might be that the disease has more psychological impact on women. Therefore, these results emphasize the need to design different interventions for different sexes to improve their quality of life. Furthermore, psychological empowerment training, appropriate exposure with the disease and its complications in female patients should be of most interest.
Among demographic variables in linear regression analysis, marital status, monthly household income, and job had reverse relationships with the quality of life; but only educational level had a direct demographic in the predictive. Similar to our findings, Nadrian et al. [26] reported that self-care behaviors can be a predictor of the quality of life in patients with rheumatoid arthritis. In another study, therefore, paying attention to self-care behaviors in patients can help improving their quality of life.
The results showed that the self-care behavior of nutrition was a stronger predictor of quality of life than self-care behaviors, blood glucose control and drug self-care. Considering the fact that most participants had primary education or illiterate, it seems difficult for them to control their blood glucose. On the other hand, the medical therapeutic protocols for the patients of diabetes is similar or almost the same. Therefore, nutritional self-care seems to be important in the quality of life of these patients. Naghibi et al. [27] also reported a direct relationship between nutritional performance and quality of life. Therefore, interventions with aimed at increasing the quality of life of diabetic patients should be taken in to account the nutrition and education of these patients. Furthermore, this shows that improving the nutritional status of patients can be effective on their quality of life's improvement.
Diabetes self-management supports are critical elements of care for all patients with diabetes and are necessary to improve outcomes in a disease that is largely self-managed. For many subjects with diabetes, the most challenging part of the treatment plan is determining what to eat.
The average age of the participants in this study was 46.50 which are relatively low. Another studies in Iran also reported that the mean age of the diabetes T2DM are relatively low [4]. WHO had estimated that the trends of incidence rate of diabetes is shifting towards lower ages [20]. The lower age of the patients in the present study calls for proper intervention and plans to tackle this problem and prevent the diabetes especially among young and middle-aged individuals.
Similar to the study of Kueh et al. [28], in our study, self-care behavior of blood sugar control was correlated with the quality of life of patients with T2DM patients. Findings of the study also are in line with those of similar study performed by Lukacs et al. [29] on T2DM patients that found an association between increased physical activity and higher quality of life. Therefore, it can be recommended that the health workers may promote physical activity among T2DM patients to help them improve their quality of life.
Strengths of this study include the use of standard tools for measuring the quality of life, which allows the measurement of physical, psychological, social, and environmental aspects of life in diabetes. Another strength is using interview method for data collection, which is more appropriate method compared to self-completion questionnaire method due to low literacy level of the participants. However, the limitations of this study include psychological conditions that may affect the subjects in an interview. Similarly using two interviewers to collect data, which may be different from each other but the interviewers were trained how to question the interviewees in order to reduce this variation. Furthermore, because of the lack of a comprehensive data registry in country we couldn't consider the possible impacts of some laboratory data, medication, and other comorbidities which could affect quality of life. The cross-sectional nature of the study also makes us cautious about causal relations. Furthermore, due to small sample size, gender specific analysis was not applicable in this study.
Finally, it can be concluded that the quality of life in peoples with T2DM is influenced by demographic factors such as gender, age, educational level, marital status, socioeconomic status, and also disease-related factors such as history of illnesses, chronic diseases, and self-care behaviors. Although demographic variables alone were very poor predictive factors of the quality of life in patients, self-care behaviors including nutrition and blood glucose control were identified as important predictors of the quality of life in these patients. Among the self-care behaviors, nutrition was the most important predictive factor. Therefore, training and appropriate interventions are needed in this area to improve self-care behaviors in T2DM patients and thus their quality of life.
Figures and Tables
Table 1
Distribution of demographic characteristics among 120 patients with type 2 diabetes mellitus in Chaldoran County, West Azerbaijan Province, Iran in 2015

Table 2
Comparison of the self-care behaviors in male (n=64) and female (n=56) patients with type 2 diabetes mellitus in Chaldoran County, West Azerbaijan Province, Iran in 2015
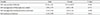
Table 3
The relationship between quality of life and some of demographic characteristics in patients with type 2 diabetes mellitus in Chaldoran County, West Azerbaijan Province, Iran in 2015

Table 4
Linear regression analysis and predictive variables of overall quality of life's score in patients with type 2 diabetes mellitus in Chaldoran County, West Azerbaijan Province, Iran in 2015

ACKNOWLEDGMENTS
This study was supported by grants from the Tabriz University of Medical Sciences. Authors would like to thank all personnel of Health vice-chancellery of Urmia University of Medical Sciences for their kind co-operation. This study is a part of a clinical trial in Student Research Committee of Tabriz University of Medical Sciences confirmed by code 588.
References
1. Ahmann AJ. Guidelines and performance measures for diabetes. Am J Manag Care. 2007; 13:Suppl 2. S41–S46.
2. Nagelkerk J, Reick K, Meengs L. Perceived barriers and effective strategies to diabetes self-management. J Adv Nurs. 2006; 54:151–158.
3. World Health Organization. Media centre: diabetes. cited 2017 Jul 18. Available from: http://www.who.int/mediacentre/factsheets/fs312/en.
4. Delavari AR, Mahdavihazaveh AR, Norozinejad A, Yarahmadi SH. Country programme of prevention and control of diabetes. 2nd ed. Tehran: Seda Publication;2004. p. 2.
5. Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2008; 26:77–82.
6. Adachi M, Yamaoka K, Watanabe M, Nishikawa M, Hida E, Kobayashi I, Tango T. Effects of lifestyle education program for type 2 diabetes patients in clinics: study design of a cluster randomized trial. BMC Public Health. 2010; 10:742.
7. Chapter 6, The history and meaning of patient compliance as an ideology. In : Gochman DS, editor. Handbook of health behavior research. II. Provider determinants. New York: Plenum Press;1997. p. 109–124.
8. Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999; 15:205–218.
9. Karlsson I, Berglin E, Larsson PA. Sense of coherence: quality of life before and after coronary artery bypass surgery: a longitudinal study. J Adv Nurs. 2000; 31:1383–1392.
10. Hall PA, Rodin GM, Vallis TM, Perkins BA. The consequences of anxious temperament for disease detection, self-management behavior, and quality of life in type 2 diabetes mellitus. J Psychosom Res. 2009; 67:297–305.
11. Shayeghian Z, Aguilar-Vafaie M, Besharat MA, Amiri P, Parvin M, Roohi-Gilani K. The association between self-care and control of blood sugar and health-related quality of life in type II diabetes patients. Iran J Endocrinol Metab. 2014; 15:545–551.
12. Lloyd CE, Orchard TJ. Physical and psychological well-being in adults with type 1 diabetes. Diabetes Res Clin Pract. 1999; 44:9–19.
13. AminiLari Z, Fararouei M, Amanat S, Sinaei E, Dianatinasab S, AminiLari M, Daneshi N, Dianatinasab M. The effect of 12 weeks aerobic, resistance, and combined exercises on omentin-1 levels and insulin resistance among type 2 diabetic middle-aged women. Diabetes Metab J. 2017; 41:205–212.
14. Nejat S, Montazeri A, Holakouie Naieni K, Mohammad K, Majdzadeh SR. The World Health Organization quality of Life (WHOQOL-BREF) questionnaire: translation and validation study of the Iranian version. J Sch Public Health Inst Public Health Res. 2006; 4:1–12.
15. Nedjat S, Montazeri A, Holakouie K, Mohammad K, Majdzadeh R. Psychometric properties of the Iranian interview-administered version of the World Health Organization’s Quality of Life Questionnaire (WHOQOL-BREF): a population-based study. BMC Health Serv Res. 2008; 8:61.
16. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000; 23:943–950.
17. Didarloo AR, Shojaeizadeh D, Gharaaghaji Asl R, Habibzadeh H, Niknami Sh, Pourali R. Prediction of self-management behavior among Iranian women with type 2 diabetes: application of the theory of reasoned action along with self-efficacy (ETRA). Iran Red Crescent Med J. 2012; 14:86–95.
18. Mohammad pour Y, Haririan HR, Moghaddasian S, Ebrahimi H. Surveying the quality of life and its dimensions among the type 2 diabetes patients referred to the Diabetes Center of Tabriz University of Medical Sciences: 1386. J Urmia Nurs Midwifery Fac. 2008; 6:26–37.
19. Wang W, Shi L, Wang K. Assessment of quality of life in patients with diabetes mellitus and impaired glucose tolerance. Zhonghua Yu Fang Yi Xue Za Zhi. 2001; 35:26–29.
20. Babazadeh T, Taghdisi MH, Sherizadeh Y, Mahmoodi H, Ezzati E, Rezakhanimoghaddam H, BanayeJeddi M. The survey of health-related quality of life and its effective factors on the intercity bus drivers of the west terminal of Tehran in 2015. Community Health J. 2015; 9:19–27.
21. Zagozdzon P, Kolarzyk E, Marcinkowski JT. Quality of life and rural place of residence in Polish women: population based study. Ann Agric Environ Med. 2011; 18:429–432.
22. Parvan K, Lakdizaji S, Roshangar F, Mostofi M. Assessment of quality of life in patients undergoing continuous hemodialysis in four hospitals of East Azarbayjan, in 2012. Razi J Med Sci. 2014; 21:19–28.
23. Arslantas D, Unsal A, Metintas S, Koc F, Arslantas A. Life quality and daily life activities of elderly people in rural areas, Eskisehir (Turkey). Arch Gerontol Geriatr. 2009; 48:127–131.
24. Genga EK, Otieno FC, Ogola EN, Maritim MC. Assessment of the perceived quality of life of non insulin dependent diabetic patients attending the Diabetes Clinic in Kenyatta National Hospital. IOSR J Pharm. 2014; 4:15–21.
25. Hatamloo Sadabadi M, Babapour Kheirodin J. Comparison of quality of life and coping strategies in diabetic and non diabetic people. J Shahid Sadoughi Univ Med Sci. 2013; 20:581–592.
26. Nadrian H, Morovati Sharifabad MA, Mirzaei A, Bahmanpur K, Moradzadeh R, Shariaty AM. Relationship between quality of life, health status and self-care behaviors in patients with rheumatoid arthritisi in yazd (central Iran). J Ilam Univ Med Sci. 2011; 19:15–25.
27. Naghibi F, Golmakani N, Ismaili H, Moharreri F. Studying the relationship between lifestyle and health-related quality of life among adolescent girls in Mashhad high schools. Iran J Obstet Gynecol Infertil. 2013; 16:9–19.
28. Kueh YC, Morris T, Borkoles E, Shee H. Modelling of diabetes knowledge, attitudes, self-management, and quality of life: a cross-sectional study with an Australian sample. Health Qual Life Outcomes. 2015; 13:129.
29. Lukacs A, Sasvari P, Torok A, Barkai L. Generic and disease-specific quality of life in adolescents with type 1 diabetes: comparison to age-matched healthy peers. J Pediatr Endocrinol Metab. 2016; 29:769–775.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download