Abstract
Glucose and lipid metabolism are linked to each other in many ways. The most important clinical manifestation of this interaction is diabetic dyslipidemia, characterized by elevated triglycerides, low high density lipoprotein cholesterol (HDL-C), and predominance of small-dense LDL particles. However, in the last decade we have learned that the interaction is much more complex. Hypertriglyceridemia and low HDL-C cannot only be the consequence but also the cause of a disturbed glucose metabolism. Furthermore, it is now well established that statins are associated with a small but significant increase in the risk for new onset diabetes. The underlying mechanisms are not completely understood but modulation of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG CoA)-reductase may play a central role as genetic data indicate that mutations resulting in lower HMG CoA-reductase activity are also associated with obesity, higher glucose concentrations and diabetes. Very interestingly, this statin induced increased risk for new onset type 2 diabetes is not detectable in subjects with familial hypercholesterolemia. Furthermore, patients with familial hypercholesterolemia seem to have a lower risk for type 2 diabetes, a phenomenon which seems to be dose-dependent (the higher the low density lipoprotein cholesterol, the lower the risk). Whether there is also an interaction between lipoprotein(a) and diabetes is still a matter of debate.
Dyslipidemia and diabetes mellitus play important roles in clinical medicine since both are well established cardiovascular risk factors and their treatment translates into clinical benefit. Many patients with type 2 diabetes have dyslipidemia and it is believed that this dyslipidemia is important in mediating the cardiovascular risk in diabetes. Therefore, diabetic dyslipidemia has been the main focus of discussions regarding the interaction between glucose and lipid metabolism. However, the link between glucose and lipid metabolism is much more complex (Table 1). This is not surprising considering the fact that both, lipids and glucose play an important role in energy metabolism and that both are regulated by the liver.
It is well known that diabetic patients often present with a typical dyslipidemia, characterized by elevated triglycerides, low high density lipoprotein cholesterol (HDL-C) and predominance of small-dense low density lipoprotein (LDL) particles. However, newer research indicates that these lipid changes may not only be the consequence of diabetes but may also cause disturbances of glucose metabolism. Studies presented during the last decade have shown that statin therapy, one of the most potent strategies to prevent cardiovascular disease increases the risk for new onset diabetes and that at the same time patients with familial hypercholesterolemia have a decreased risk for type 2 diabetes. Whether there is also relationship between lipoprotein(a) and diabetes is still a matter of debate.
This review article will summarize our current knowledge on these topics and discuss them from a clinical point of view.
The majority of patients with type 2 diabetes exhibit a dyslipidemia which is characterized by elevated triglycerides, low HDL-C and the predominance of small-dense LDL particles [1]. Although not all diabetic patients show all manifestations, 60% to 70% of patients show at least some lipid abnormality. This dyslipidemia presents a major (probably the most important) link between diabetes and cardiovascular disease. The characteristic lipid changes are not only seen in patients with overt diabetes but also in patients with metabolic syndrome and are therefore believed to reflect insulin resistance rather than hyperglycemia [2]. Furthermore, it is also known that good glucose control improves dyslipidemia but does not eliminate it. The dyslipidemia is based on inflammatory processes and on flooding of the body with energy rich substrates which then results in hepatic and intestinal lipoprotein overproduction leading to hypertriglyceridemia [34]. The elevated concentration of triglyceride-rich lipoproteins leads to an increased catabolism of HDL (resulting in low HDL-C) and a shift in the LDL phenotype towards small dense LDL which are more atherogenic then "normal" LDL [56].
Although hypertriglyceridemia and low HDL-C may be the dominant abnormality, patients benefit most from lowering low density lipoprotein cholesterol (LDL-C). Many studies have shown that diabetic patients experience the same risk reduction from statin based LDL-C lowering as non-diabetic patients [7]. Therefore the primary strategy is to achieve the LDL-C goal [8]. This goal is <70 mg/dL (<1.8 mmol/L) in diabetic patients with additional cardiovascular risk factors or atherosclerotic disease. The goal is <100 mg/dL (<2.3 mmol/L) in all other diabetic patients. If statins are not sufficient to reach this goal then combination therapy with ezetimibe should be used [9]. The recently published data on the IMPROVE-IT (IMProved Reduction of Outcomes: Vytorin Efficacy International Trial) trial indicate that diabetic patients may particularly benefit from statin ezetimibe combination. Whether and how hypertriglyceridemia often observed in diabetic patients should be treated with additional fibrates or omega-3-fatty acids is still a matter of debate [10]. Large outcome trials have been negative but these trials were flawed by methodological problems [111213]. In our department, we first try to achieve the LDL-C goal and then consider additional fibrates or additional omega-3 fatty acids in very high risk patients with elevated triglycerides. Although outcome trials were negative subgroup analyses and a meta-analysis indicate that diabetic patients may benefit from such a strategy [14].
In recent years it was recognized that lipid changes may not only be a consequence of impaired glucose metabolism but also cause them. Hypertriglyceridemia and low HDL-C are important in that context. Elevated levels of triglycerides lead to elevated levels of free fatty acids which may induce insulin resistance and β-cell dysfunction [1516]. Although the exact mechanisms are only partially understood it seems that elevated concentrations of free fatty acids disrupt or modulate the cascade linking insulin receptors with glucose transporters and impair the normal function of the β-cell [17]. Furthermore, free fatty acids are important modulators of inflammation. Therefore hypertriglyceridemia may induce subclinical inflammation which then leads to insulin resistance and β-cell dysfunction. The fact that hypertriglyceridemia can worsen glucose metabolism is clinically important as it explains why it is more difficult to control hyperglycemia in patients with hypertriglyceridemia compared to those with normal triglyceride values. It also explains why patients usually require less intensive antidiabetic treatment once hypertriglyceridemia has resolved.
More recently it was shown that also HDL may directly affect glucose metabolism [18]. In a study evaluating the cholesterylester transfer protein inhibitor torcetrapib it was observed that higher HDL-C concentrations were associated with less hyperglycemia [19]. Also it was demonstrated that the infusion of recombinant HDL can improve glucose metabolism in patients with type 2 diabetes [20]. Since then a number of studies have tried to shed light on the underlying pathophysiology and several mechanisms were identified (Fig. 1) [2122]. HDL induce reverse cholesterol transport and the altered intracellular lipid environment is believed to reduce micro-inflammation. Furthermore, direct anti-inflammatory properties of HDL may also play a role.
Recently it was shown in an animal (mouse) model that apolipoprotein A1 (apoA1) knock-out results in a clinical picture resembling metabolic syndrome while apoA1 overexpression improves glucose metabolism and results in a higher lean body mass and a higher expression of mitochondrial ATP synthase (Fig. 2) [21]. Interestingly, in the same model apoA1 overexpression could also prevent diet induced obesity. Although rodent and human lipoprotein metabolism differs considerably these findings may also help to explain the interaction of HDL and glucose metabolism in humans.
From a clinical point of view it is relevant that dyslipidemia may not only be a consequence but also a cause of glucose dysregulation. This would indicate that subjects with low HDL-C are at higher risk of developing type 2 diabetes. The same holds obviously true for patients with hypertriglyceridemia.
It was first observed in the JUPITER (Justification for the Use of Statins in Primary Prevention: An Intervention Trial Evaluating Rosuvastatin) trial that patients receiving high dose rosuvastatin have a higher risk for developing type 2 diabetes compared to those receiving placebo [23]. This contrasted with earlier studies were no such effect or even a protective effect (The West of Scotland Coronary Prevention Study, WOSCOP study) was observed [24]. Following the WOSCOP study a number of smaller trials tried to clarify the effect of statins on insulin resistance and insulin secretion without giving clear results [25].
After the JUPITER trial many data sets were reanalyzed and it was shown that the risk for new onset diabetes is increased with statin therapy. The increased incidence was confirmed in the Women's Health Initiative (odds ratio [OR], 1.7) [26] and also in a Finish observational study evaluating almost 8,500 nondiabetic men (OR, 1.24) [27] as well as in a number of meta-analyses. One such meta-analysis evaluated whether reaching certain LDL-C levels is associated with an increased risk for type 2 diabetes. It was shown that the OR for developing diabetes is 1.33 in those reaching an LDL-C <70 mg/dL (<1.8 mmol/L), while the OR is 1.16 in those achieving an LDL-C between 70 and 100 mg/dL (1.8 and 2.3 mmol/L) and not elevated in those with LDL-C above 100 mg/dL (2.3 mmol/L) [28]. Further analyses then indicated that the risk for new onset diabetes holds probably true for all statins and occurs in a dose dependent fashion (Table 2) [29].
Although all statins may induce type 2 diabetes risk may be particularly high with atorvastatin and rosuvastatin and less so with pravastatin and lovastatin. These differences probably reflect differences in potency, lipophilic/hydrophilic properties and organ specificity. Generally, higher doses of statins increase the risk more than lower doses [30]. It was also shown that patients with metabolic syndrome have the highest risk for developing diabetes during statin therapy. The underlying mechanism is not completely understood but current evidence indicates that it may either be the modulation of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA)-reductase or the low LDL-C itself that induces these changes in glucose metabolism (Fig. 3). There is, however, no evidence that statins directly impact on glucose metabolism. Very interesting genetic data indicate that mutations which decrease the activity of HMG-CoA-reductase are associated with lower LDL-C and lower cardiovascular risk but also with higher body weight, higher plasma glucose concentrations and higher risk for diabetes [31]. Interestingly statin therapy is also associated with a slight but significant increase in body weight (0.24 kg) [31]. Since statins inhibit HMG-CoA reductase it could be hypothesized that modulation of HMG-CoA reductase activity affects glucose metabolism. However, the observation could also relate to a more general phenomenon, namely that the lipid concentration in certain intracellular compartments modulates glucose metabolism. In the liver and in the muscle this may result in a reduced insulin effect while in the β-cells of the pancreas this results in dysregulation of insulin secretion.
Interestingly, ezetimibe (at least in addition to statins) and proprotein convertase subtilisin/kexin type 9 (PCSK9) antibodies do not seem to have an impact on glucose metabolism [93233]. This would indicate, that the increased risk is primarily related to modulating the activity of HMG-CoA-reductase.
The clinical significance of the observed increased risk for new onset diabetes with statin therapy is unclear as in most situation benefit of statin induced LDL-C lowering dramatically outweighs the risk of new onset diabetes. Furthermore, statin therapy decreases overall mortality in primary and secondary prevention settings. Nevertheless, it may be prudent to evaluate glucose levels regularly in patients with metabolic syndrome on higher doses of statins.
In recent years patients with familial hypercholesterolemia have returned into the focus of lipidology [3435]. Familial hypercholesterolemia can be caused by mutations affecting the LDL-receptor gene, the gene encoding apolipoprotein B, the protein binding to the LDL-receptor, or the gene encoding PCSK9, a regulator of LDL-receptor recycling [3435]. All mutations result in a decreased catabolism of LDL-particles through the LDL-receptor. The decreased catabolism of LDL directly translates into elevated LDL-C levels. The elevated cholesterol levels are causally linked to cardiovascular disease. In addition, the elevated concentration of plasma lipoproteins can result in the deposition of lipids in a number of other organs resulting in the formation of xanthomas and arcus lipoides. Thus, patients with familial hypercholesterolemia are characterized by elevated LDL-C plasma concentration, premature cardiovascular disease, skin manifestation and usually a strong positive family history for hypercholesterolemia and atherosclerotic disease. The risk for cardiovascular events in affected individuals is approximately 10 to 20 folds higher than in those not affected [36]. A number of studies have shown that LDL-C lowering therapy with statins can dramatically improve the prognosis of these subjects [3738]. It is therefore recommended that statin therapy is initiated early in life (childhood or young adulthood) with some variation depending on the LDL-C level, the family history and the presence of additional risk factors [3435].
Considering the increased risk for new onset diabetes associated with statin therapy it is of particular interest to evaluate how familial hypercholesterolemia and its treatment is linked to glucose metabolism. In a Dutch study it was recently demonstrated that the prevalence of type 2 diabetes in patients with familial hypercholesterolemia was significantly lower than among unaffected relatives (Table 3) [39]. It was shown that patients with familial hypercholesterolemia have an almost 40% reduction in relative risk (prevalence of type 2 diabetes 1.75% in familial hypercholesterolemia and 2.93% in unaffected relatives). After adjusting for potential confounders such as age, body mass index, statin use, etc., the relative risk was even further decreased (OR, 0.49). Furthermore this association seemed dose dependent since patients with a LDL receptor mutation had the lowest diabetes prevalence while those with apoB mutations (which usually have lower LDL-C concentrations) were at intermediate risk. Similarly, LDL receptor negative carriers (highest LDL-C concentration) had a lower risk than LDL receptor defective carriers. These data confirm previous smaller studies [40].
This raises again the question which mechanisms mediate this observation. Due to the decreased uptake of LDL via the LDL-receptor in familial hypercholesterolemia, cholesterol concentration may be lower in certain intracellular compartments. At the same time HMG-CoA-reductase activity may be increased [41]. Both phenomena are opposite to those observed during statin therapy. This indicates again that either the modulation of HMG-CoA-reductase or the intracellular lipid concentration is directly linked to glucose metabolism.
Considering the increased risk for new onset diabetes associated with statin therapy it is obviously of interest to evaluate whether patients who receive statins for most of their lives are also characterized by changes in glucose metabolism. Recent analyses indicate that in patients with familial hypercholesterolemia long-term statin therapy is not associated with an increased risk for new onset diabetes [42]. Kusters et al. [43] followed children with familial hypercholesterolemia and their non-affected siblings and did not find a difference in new onset diabetes over a period of 10 years. Similarly Skoumas et al. [44] reported 10-year data in adult patients with familial hypercholesterolemia and again did not find the diabetes risk being increased by statin therapy. From the available data it is however unclear whether statin therapy "increases" diabetes risk from subnormal levels to normal levels in familial hypercholesterolemia patients or whether the risk remains decreased.
In summary these data indicate that patients with familial hypercholesterolemia have a decreased risk for diabetes mellitus and that statin therapy in familial hypercholesterolemia patients is not associated with an increased risk for new onset diabetes. As outlined above this contrasts with non-familial hypercholesterolemia populations where statin therapy is associated with new onset diabetes in a dose-dependent manner.
These findings have considerable clinical impact as there was some concern in the past about treating patients with familial hypercholesterolemia, especially children, with statins for decades. However, these data indicate that such therapy does not increase the risk for type 2 diabetes.
Whether or not lipoprotein(a) concentrations or metabolism is related to disturbances of glucose metabolism or development of type 2 diabetes is still a matter of debate. Some studies report a negative relationship between lipoprotein(a) concentrations and the incidence of type 2 diabetes [45] others show a strong positive association [46] and again others no association [47]. The relationship between elevated lipoprotein(a) and glucose metabolism is further complicated by the fact that lipoprotein(a) concentration itself is weakly correlated with other lipid abnormalities. Thus, lipoprotein(a) concentration is positively correlated with apoB100 levels and non-HDL-C concentration and inversely correlated with triglyceride concentrations [48]. Thus, it could be that lipoprotein(a)-concentrations and glucose metabolism are not directly linked to each other but that the associations observed in some studies reflect indirect aspects.
Glucose and lipids are both important components of energy metabolism. It is therefore not surprising that glucose metabolism and lipid metabolism are closely linked to each other. This has important clinical implications. Thus, diabetic patients are characterized by a typical dyslipidemia which is closely linked to the cardiovascular disease in these patients. However, hypertriglyceridemia and low HDL-C may also induce disturbances of glucose metabolism and may thus be the consequence and the source of hyperglycemia. Surprisingly, statin therapy is associated with a small but significant increase in the rate of new onset diabetes but benefit of statin therapy outweighs risk in almost all clinical situations. Finally, patients with familial hypercholesterolemia have a decreased risk of type 2 diabetes which depends on the severity of the LDL elevation (the higher the LDL-C the lower the risk). It is important to understand the underlying pathophysiology to better address the clinical aspects and to develop new strategies against dyslipidemia and diabetes.
Figures and Tables
Fig. 1
High density lipoprotein (HDL) may be linked to glucose metabolism in multiple ways. HDL (at least certain subtypes) have direct anti-inflammatory properties. HDL are also the central component of reverse cholesterol transport and mediate cholesterol efflux from many tissues. This may change the micro environment such that insulin sensitivity and insulin secretion improve.

Fig. 2
Animal studies indicate that knock-out and overexpression of apolipoprotein A1 (apoA1) affect many metabolic pathways related to diabetes development [21]. Whether the results observed in rodents are also valid in humans is unknown. HDL, high density lipoprotein; HbA1c, glycosylated hemoglobin.

Fig. 3
Statin therapy is associated with a small increase in new-onset diabetes type 2. The underlying pathophysiology is not well understood. A number of different mechanisms may lead to decreased insulin sensitivity and altered β-cell function. In predisposed subjects this may induce the manifestation of type 2 diabetes. HMG-CoA, 3-hydroxy-3-methylglutaryl-coenzyme A.

Table 1
Selected aspects of clinically relevant interactions between glucose and lipid metabolism

Table 2
Association of different statins and development of diabetes [29]
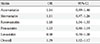
| Statin | OR | 95% CI |
|---|---|---|
| Atorvastatin | 1.14 | 0.89-1.46 |
| Simvastatin | 1.11 | 0.97-1.26 |
| Rosuvastatin | 1.18 | 1.04-1.33 |
| Pravastatin | 1.03 | 0.90-1.19 |
| Lovastatin | 0.98 | 0.70-1.38 |
| Overall | 1.09 | 1.02-1.17 |
Table 3
Association between type 2 diabetes mellitus and familial hypercholesterolemia [39]

| Adjusted OR | |
|---|---|
| Not affected | 1 |
| All affected | 0.49 |
| apoB mutation | 0.65 |
| LDL-R mutation | 0.45 |
| LDL-R defective | 0.49 |
| LDL-R negative | 0.38 |
References
1. Wu L, Parhofer KG. Diabetic dyslipidemia. Metabolism. 2014; 63:1469–1479.
2. Avramoglu RK, Basciano H, Adeli K. Lipid and lipoprotein dysregulation in insulin resistant states. Clin Chim Acta. 2006; 368:1–19.
3. Adiels M, Olofsson SO, Taskinen MR, Boren J. Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2008; 28:1225–1236.
4. Duez H, Lamarche B, Uffelman KD, Valero R, Cohn JS, Lewis GF. Hyperinsulinemia is associated with increased production rate of intestinal apolipoprotein B-48-containing lipoproteins in humans. Arterioscler Thromb Vasc Biol. 2006; 26:1357–1363.
5. Guerin M, Le Goff W, Lassel TS, Van Tol A, Steiner G, Chapman MJ. Atherogenic role of elevated CE transfer from HDL to VLDL(1) and dense LDL in type 2 diabetes: impact of the degree of triglyceridemia. Arterioscler Thromb Vasc Biol. 2001; 21:282–288.
6. Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002; 43:1363–1379.
7. Cholesterol Treatment Trialists' (CTT) Collaborators. Kearney PM, Blackwell L, Collins R, Keech A, Simes J, Peto R, Armitage J, Baigent C. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008; 371:117–125.
8. Catapano AL, Reiner Z, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman M, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D. European Society of Cardiology (ESC). European Atherosclerosis Society (EAS). ESC/EAS Guidelines for the management of dyslipidaemias The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Atherosclerosis. 2011; 217:3–46.
9. Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, Darius H, Lewis BS, Ophuis TO, Jukema JW, De Ferrari GM, Ruzyllo W, De Lucca P, Im K, Bohula EA, Reist C, Wiviott SD, Tershakovec AM, Musliner TA, Braunwald E, Califf RM. IMPROVE-IT Investigators. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015; 372:2387–2397.
10. Hegele RA, Ginsberg HN, Chapman MJ, Nordestgaard BG, Kuivenhoven JA, Averna M, Boren J, Bruckert E, Catapano AL, Descamps OS, Hovingh GK, Humphries SE, Kovanen PT, Masana L, Pajukanta P, Parhofer KG, Raal FJ, Ray KK, Santos RD, Stalenhoef AF, Stroes E, Taskinen MR, Tybjaerg-Hansen A, Watts GF, Wiklund O. European Atherosclerosis Society Consensus Panel. The polygenic nature of hypertriglyceridaemia: implications for definition, diagnosis, and management. Lancet Diabetes Endocrinol. 2014; 2:655–666.
11. ORIGIN Trial Investigators. Bosch J, Gerstein HC, Dagenais GR, Diaz R, Dyal L, Jung H, Maggiono AP, Probstfield J, Ramachandran A, Riddle MC, Ryden LE, Yusuf S. n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med. 2012; 367:309–318.
12. ACCORD Study Group. Ginsberg HN, Elam MB, Lovato LC, Crouse JR 3rd, Leiter LA, Linz P, Friedewald WT, Buse JB, Gerstein HC, Probstfield J, Grimm RH, Ismail-Beigi F, Bigger JT, Goff DC Jr, Cushman WC, Simons-Morton DG, Byington RP. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1563–1574.
13. Kromhout D, Giltay EJ, Geleijnse JM. Alpha Omega Trial Group. n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med. 2010; 363:2015–2026.
14. Jun M, Foote C, Lv J, Neal B, Patel A, Nicholls SJ, Grobbee DE, Cass A, Chalmers J, Perkovic V. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010; 375:1875–1884.
15. Briaud I, Harmon JS, Kelpe CL, Segu VB, Poitout V. Lipotoxicity of the pancreatic beta-cell is associated with glucose-dependent esterification of fatty acids into neutral lipids. Diabetes. 2001; 50:315–321.
16. Lee Y, Hirose H, Ohneda M, Johnson JH, McGarry JD, Unger RH. Beta-cell lipotoxicity in the pathogenesis of non-insulin-dependent diabetes mellitus of obese rats: impairment in adipocyte-beta-cell relationships. Proc Natl Acad Sci U S A. 1994; 91:10878–10882.
17. Rachek LI. Free fatty acids and skeletal muscle insulin resistance. Prog Mol Biol Transl Sci. 2014; 121:267–292.
18. Drew BG, Rye KA, Duffy SJ, Barter P, Kingwell BA. The emerging role of HDL in glucose metabolism. Nat Rev Endocrinol. 2012; 8:237–245.
19. Barter PJ, Rye KA, Tardif JC, Waters DD, Boekholdt SM, Breazna A, Kastelein JJ. Effect of torcetrapib on glucose, insulin, and hemoglobin A1c in subjects in the Investigation of Lipid Level Management to Understand its Impact in Atherosclerotic Events (ILLUMINATE) trial. Circulation. 2011; 124:555–562.
20. Drew BG, Duffy SJ, Formosa MF, Natoli AK, Henstridge DC, Penfold SA, Thomas WG, Mukhamedova N, de Courten B, Forbes JM, Yap FY, Kaye DM, van Hall G, Febbraio MA, Kemp BE, Sviridov D, Steinberg GR, Kingwell BA. High-density lipoprotein modulates glucose metabolism in patients with type 2 diabetes mellitus. Circulation. 2009; 119:2103–2111.
21. Lehti M, Donelan E, Abplanalp W, Al-Massadi O, Habegger KM, Weber J, Ress C, Mansfeld J, Somvanshi S, Trivedi C, Keuper M, Ograjsek T, Striese C, Cucuruz S, Pfluger PT, Krishna R, Gordon SM, Silva RA, Luquet S, Castel J, Martinez S, D'Alessio D, Davidson WS, Hofmann SM. High-density lipoprotein maintains skeletal muscle function by modulating cellular respiration in mice. Circulation. 2013; 128:2364–2371.
22. Mortensen SP, Boushel R. High-density lipoprotein: a new therapeutic target for glucose intolerance? Circulation. 2013; 128:2349–2350.
23. Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ. JUPITER Study Group. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008; 359:2195–2207.
24. Freeman DJ, Norrie J, Sattar N, Neely RD, Cobbe SM, Ford I, Isles C, Lorimer AR, Macfarlane PW, McKillop JH, Packard CJ, Shepherd J, Gaw A. Pravastatin and the development of diabetes mellitus: evidence for a protective treatment effect in the West of Scotland Coronary Prevention Study. Circulation. 2001; 103:357–362.
25. Huptas S, Geiss HC, Otto C, Parhofer KG. Effect of atorvastatin (10 mg/day) on glucose metabolism in patients with the metabolic syndrome. Am J Cardiol. 2006; 98:66–69.
26. Culver AL, Ockene IS, Balasubramanian R, Olendzki BC, Sepavich DM, Wactawski-Wende J, Manson JE, Qiao Y, Liu S, Merriam PA, Rahilly-Tierny C, Thomas F, Berger JS, Ockene JK, Curb JD, Ma Y. Statin use and risk of diabetes mellitus in postmenopausal women in the Women's Health Initiative. Arch Intern Med. 2012; 172:144–152.
27. Cederberg H, Stancakova A, Yaluri N, Modi S, Kuusisto J, Laakso M. Increased risk of diabetes with statin treatment is associated with impaired insulin sensitivity and insulin secretion: a 6 year follow-up study of the METSIM cohort. Diabetologia. 2015; 58:1109–1117.
28. Cai R, Yuan Y, Zhou Y, Xia W, Wang P, Sun H, Yang Y, Huang R, Wang S. Lower intensified target LDL-c level of statin therapy results in a higher risk of incident diabetes: a meta-analysis. PLoS One. 2014; 9:e104922.
29. Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, Seshasai SR, McMurray JJ, Freeman DJ, Jukema JW, Macfarlane PW, Packard CJ, Stott DJ, Westendorp RG, Shepherd J, Davis BR, Pressel SL, Marchioli R, Marfisi RM, Maggioni AP, Tavazzi L, Tognoni G, Kjekshus J, Pedersen TR, Cook TJ, Gotto AM, Clearfield MB, Downs JR, Nakamura H, Ohashi Y, Mizuno K, Ray KK, Ford I. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 2010; 375:735–742.
30. Preiss D, Seshasai SR, Welsh P, Murphy SA, Ho JE, Waters DD, DeMicco DA, Barter P, Cannon CP, Sabatine MS, Braunwald E, Kastelein JJ, de Lemos JA, Blazing MA, Pedersen TR, Tikkanen MJ, Sattar N, Ray KK. Risk of incident diabetes with intensive-dose compared with moderate-dose statin therapy: a meta-analysis. JAMA. 2011; 305:2556–2564.
31. Swerdlow DI, Preiss D, Kuchenbaecker KB, Holmes MV, Engmann JE, Shah T, Sofat R, Stender S, Johnson PC, Scott RA, Leusink M, Verweij N, Sharp SJ, Guo Y, Giambartolomei C, Chung C, Peasey A, Amuzu A, Li K, Palmen J, Howard P, Cooper JA, Drenos F, Li YR, Lowe G, Gallacher J, Stewart MC, Tzoulaki I, Buxbaum SG, van der AD, Forouhi NG, Onland-Moret NC, van der Schouw YT, Schnabel RB, Hubacek JA, Kubinova R, Baceviciene M, Tamosiunas A, Pajak A, Topor-Madry R, Stepaniak U, Malyutina S, Baldassarre D, Sennblad B, Tremoli E, de Faire U, Veglia F, Ford I, Jukema JW, Westendorp RG, de Borst GJ, de Jong PA, Algra A, Spiering W, Maitland-van der Zee AH, Klungel OH, de Boer A, Doevendans PA, Eaton CB, Robinson JG, Duggan D, Kjekshus J, Downs JR, Gotto AM, Keech AC, Marchioli R, Tognoni G, Sever PS, Poulter NR, Waters DD, Pedersen TR, Amarenco P, Nakamura H, McMurray JJ, Lewsey JD, Chasman DI, Ridker PM, Maggioni AP, Tavazzi L, Ray KK, Seshasai SR, Manson JE, Price JF, Whincup PH, Morris RW, Lawlor DA, Smith GD, Ben-Shlomo Y, Schreiner PJ, Fornage M, Siscovick DS, Cushman M, Kumari M, Wareham NJ, Verschuren WM, Redline S, Patel SR, Whittaker JC, Hamsten A, Delaney JA, Dale C, Gaunt TR, Wong A, Kuh D, Hardy R, Kathiresan S, Castillo BA, van der Harst P, Brunner EJ, Tybjaerg-Hansen A, Marmot MG, Krauss RM, Tsai M, Coresh J, Hoogeveen RC, Psaty BM, Lange LA, Hakonarson H, Dudbridge F, Humphries SE, Talmud PJ, Kivimaki M, Timpson NJ, Langenberg C, Asselbergs FW, Voevoda M, Bobak M, Pikhart H, Wilson JG, Reiner AP, Keating BJ, Hingorani AD, Sattar N. DIAGRAM Consortium. MAGIC Consortium. InterAct Consortium. HMG-coenzyme A reductase inhibition, type 2 diabetes, and bodyweight: evidence from genetic analysis and randomised trials. Lancet. 2015; 385:351–361.
32. Robinson JG, Farnier M, Krempf M, Bergeron J, Luc G, Averna M, Stroes ES, Langslet G, Raal FJ, El Shahawy M, Koren MJ, Lepor NE, Lorenzato C, Pordy R, Chaudhari U, Kastelein JJ. ODYSSEY LONG TERM Investigators. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015; 372:1489–1499.
33. Sabatine MS, Giugliano RP, Wiviott SD, Raal FJ, Blom DJ, Robinson J, Ballantyne CM, Somaratne R, Legg J, Wasserman SM, Scott R, Koren MJ, Stein EA. Open-Label Study of Long-Term Evaluation against LDL Cholesterol (OSLER) Investigators. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015; 372:1500–1509.
34. Cuchel M, Bruckert E, Ginsberg HN, Raal FJ, Santos RD, Hegele RA, Kuivenhoven JA, Nordestgaard BG, Descamps OS, Steinhagen-Thiessen E, Tybjaerg-Hansen A, Watts GF, Averna M, Boileau C, Boren J, Catapano AL, Defesche JC, Hovingh GK, Humphries SE, Kovanen PT, Masana L, Pajukanta P, Parhofer KG, Ray KK, Stalenhoef AF, Stroes E, Taskinen MR, Wiegman A, Wiklund O, Chapman MJ. European Atherosclerosis Society Consensus Panel on Familial Hypercholesterolaemia. Homozygous familial hypercholesterolaemia: new insights and guidance for clinicians to improve detection and clinical management. A position paper from the Consensus Panel on Familial Hypercholesterolaemia of the European Atherosclerosis Society. Eur Heart J. 2014; 35:2146–2157.
35. Nordestgaard BG, Chapman MJ, Humphries SE, Ginsberg HN, Masana L, Descamps OS, Wiklund O, Hegele RA, Raal FJ, Defesche JC, Wiegman A, Santos RD, Watts GF, Parhofer KG, Hovingh GK, Kovanen PT, Boileau C, Averna M, Boren J, Bruckert E, Catapano AL, Kuivenhoven JA, Pajukanta P, Ray K, Stalenhoef AF, Stroes E, Taskinen MR, Tybjaerg-Hansen A. European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013; 34:3478–3490a.
36. Umans-Eckenhausen MA, Sijbrands EJ, Kastelein JJ, Defesche JC. Low-density lipoprotein receptor gene mutations and cardiovascular risk in a large genetic cascade screening population. Circulation. 2002; 106:3031–3036.
37. Raal FJ, Pilcher GJ, Panz VR, van Deventer HE, Brice BC, Blom DJ, Marais AD. Reduction in mortality in subjects with homozygous familial hypercholesterolemia associated with advances in lipid-lowering therapy. Circulation. 2011; 124:2202–2207.
38. Versmissen J, Oosterveer DM, Yazdanpanah M, Defesche JC, Basart DC, Liem AH, Heeringa J, Witteman JC, Lansberg PJ, Kastelein JJ, Sijbrands EJ. Efficacy of statins in familial hypercholesterolaemia: a long term cohort study. BMJ. 2008; 337:a2423.
39. Besseling J, Kastelein JJ, Defesche JC, Hutten BA, Hovingh GK. Association between familial hypercholesterolemia and prevalence of type 2 diabetes mellitus. JAMA. 2015; 313:1029–1036.
40. Vohl MC, Gaudet D, Moorjani S, Tremblay G, Perron P, Gagne C, Lesiege D, Bergeron J, Lupien PJ, Despres JP. Comparison of the effect of two low-density lipoprotein receptor class mutations on coronary heart disease among French-Canadian patients heterozygous for familial hypercholesterolaemia. Eur J Clin Invest. 1997; 27:366–373.
41. Brown MS, Goldstein JL. Familial hypercholesterolemia: defective binding of lipoproteins to cultured fibroblasts associated with impaired regulation of 3-hydroxy-3-methylglutaryl coenzyme A reductase activity. Proc Natl Acad Sci U S A. 1974; 71:788–792.
42. Vuorio A, Strandberg TE, Schneider WJ, Kovanen PT. Statins and new-onset diabetes mellitus: a risk lacking in familial hypercholesterolaemia. J Intern Med. 2015; 08. 11. [Epub]. DOI: 10.1111/joim.12405.
43. Kusters DM, Avis HJ, de Groot E, Wijburg FA, Kastelein JJ, Wiegman A, Hutten BA. Ten-year follow-up after initiation of statin therapy in children with familial hypercholesterolemia. JAMA. 2014; 312:1055–1057.
44. Skoumas J, Liontou C, Chrysohoou C, Masoura C, Aznaouridis K, Pitsavos C, Stefanadis C. Statin therapy and risk of diabetes in patients with heterozygous familial hypercholesterolemia or familial combined hyperlipidemia. Atherosclerosis. 2014; 237:140–145.
45. Mora S, Kamstrup PR, Rifai N, Nordestgaard BG, Buring JE, Ridker PM. Lipoprotein(a) and risk of type 2 diabetes. Clin Chem. 2010; 56:1252–1260.
46. Habib SS, Aslam M. Lipids and lipoprotein(a) concentrations in Pakistani patients with type 2 diabetes mellitus. Diabetes Obes Metab. 2004; 6:338–343.
47. Todoric J, Handisurya A, Leitner K, Harreiter J, Hoermann G, Kautzky-Willer A. Lipoprotein(a) is not related to markers of insulin resistance in pregnancy. Cardiovasc Diabetol. 2013; 12:138.
48. Emerging Risk Factors Collaboration. Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, White IR, Marcovina SM, Collins R, Thompson SG, Danesh J. Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA. 2009; 302:412–423.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download