INTRODUCTION
Insulin treatments are necessary for sugar control not only in type 1 diabetes mellitus (T1DM) patients, but also in type 2 diabetes mellitus (T2DM) patients. As for insulin injections, an intramuscular injection leads to a faster absorption than the desirable rate, while intradermal injection causes insulin leakage and pain, for which reasons insulin must be injected not into the muscles, dermis, and nerves, but into the subcutaneous tissue [
1]. However the subcutaneous tissue thickness of patients varies depending on the age, gender, body mass index (BMI), and parts of the body [
2,
3], and the injected subcutaneous area depends on the length of a needle [
4]. Therefore, before an insulin injection, the injection site, the subcutaneous fat thickness, the injection method, the length of the needle, and other psychological factors must be considered.
Yet, nurses constantly trained patients to inject insulin to diabetic patients with needles of the same length, regardless of the skin and subcutaneous adipose layer thicknesses [
4], and most patients inject insulin themselves with the syringes that they were trained with. Currently 8-mm needle syringes are used to inject insulin in clinical settings, and because these needles are long, people are trained to either inject insulin at 45-degree angle or after making skinfolds.
Gibney et al. [
3] reported that 15% of the content was injected into the muscles when injecting normal saline with 8-mm long needles. In such a way, if diabetic patients are injected with insulin with an 8-mm long needle, a fair amount of the insulin may be injected into the muscular layer. This is more likely in pregnant women who avoid intraperitoneal injections and tend to inject insulin into the upper arm, where creating skinfold is extremely difficult by themselves, and therefore it is much more likely for them to inject insulin into the muscles instead during self-injections. If insulin is injected to the highly vascularized muscles, the absorption rate becomes much quicker, leading to fluctuations in sugar control and hence bringing about predicaments such as difficulties in estimating the reaction to hypoglycemia [
5,
6], while intracutaneous injections engenders insulin leakage and subsequent skin damage [
6]. Therefore, in order to inject insulin into the subcutaneous adipose layer, some measure of injection techniques such as choice of injection site, injection angle, creating skinfolds, etc. are required, but such complexities reduce compliance to insulin injections, for which reason simplifying the injection skills is necessary. Extra care is demanded especially when training the annually increasing number of old diabetic patients [
7].
In this context, usage of short needles that can inject insulin into the subcutaneous adipose layer at right angles are recommended [
3,
8,
9], and recently needles of different lengths have been developed and used such as 4-mm needle syringes. However, obese patients are recommended to use longer needles in order to reach the desired depth [
10]. Collectively, measuring the skin and subcutaneous adipose layer thicknesses and identifying by which factors these thicknesses are affected, and therefore selecting the appropriate injection sites and needle length in diabetic patients in need of insulin injections is needed.
However, no studies have measured the skin and subcutaneous thicknesses of Korean diabetic patients yet, and therefore it is not yet possible to determine which needle length is appropriate. In addition, because insulin is repeatedly injected into a confined area, conditions that lead either to the shrinkage or enlargement of the subcutaneous tissue of the injection sites, such as lipodystrophy, occurs. Therefore, patients are educated to inject insulin at least 2 inches away from the navel, and use the insulin injection chart which they can refer to and circulate around each site with at least a 1- to 2-cm gap between injections [
1]. Unfortunately, although most diabetic patients claim to comply with the instructions and circulate in between each injection [
11], according to a preliminary investigation of this study, virtually none of the patients used the full injection sites available. Hence, a study that presents the skin and subcutaneous fat thicknesses of all the available injection sites on the abdomen and upper arm should be conducted to provide the patients with stronger evidence to motivate them to circulate around all injection sites.
Many studies regarding the skin and subcutaneous fat thicknesses [
3,
12] and insulin syringe needle length [
3,
5,
8,
13] have already been published not only from abroad, but endemic studies also exist regarding the skin thickness [
14,
15], subcutaneous fat thickness [
4,
16,
17,
18], and needle length [
2]. Even so, a major drawback remains that even if it is the same abdomen or upper arm, the subcutaneous fat thickness can vary depending on where it was measured [
17]. Despite this knowledge, other studies claim that a measurement from only one spot on the abdomen and upper arm represents the subcutaneous fat thickness throughout the respective body part. Not only is this insufficient to be used as an back-up evidence to encourage patients to circulate around the injection sites, but not even a single study exist investigating the appropriate insulin syringe needle length.
The main objective of this research is to inspect the skin, subcutaneous fat, and the total skin and subcutaneous fat thicknesses of the abdominal and upper arm of diabetic patients and elucidate the underlying factors affecting these thicknesses, so that we can determine the availability of using different length needles on the base of measured skin and subcutaneous fat thicknesses.
RESULTS
The clinical characteristics of subjects
The clinical characteristics of the subjects are shown in
Table 1. The mean age was 62.15±13.91 and 53.8% were male. Their average BMI was 24.09±3.43, with 58.4% of the subjects in the over-weight group. Fifty-one patients (32.7%) used insulin for sugar control, 62 (40.0%) had complications due to diabetes, and 74 (47.7%) had a family history of diabetes.
The skin and subcutaneous fat thicknesses
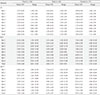
The skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the abdomen depending on injection sites are shown in
Table 2, with the thickness of the skin of 2.29±0.37 mm (range, 1.34 to 3.29 mm), thickness of subcutaneous fat of 10.15±6.54 mm (range, 0.75 to 36.34 mm), and the total skin and subcutaneous fat thickness of 12.44±6.56 mm (range, 2.24 to 38.24 mm).
The thickest point of the skin in the abdomen was 7 for males and 8 for females, whereas the thinnest point was 13 for both. The skin thickness range was 1.20 to 3.80 mm and 1.00 to 3.80 mm for males and females, respectively.
The thickest point of the subcutaneous fat and the total thickness of skin and subcutaneous fat in the abdomen was 12 for both males and females, while the thinnest point was 13 for both. The subcutaneous fat thickness range was 0.40 to 36.30 mm and 0.20 to 39.40 mm for males and females, respectively, and the total thickness of skin and subcutaneous fat range was 1.80 to 38.30 mm and 1.70 to 41.30 mm for males and females, respectively.
The skin and subcutaneous fat thicknesses
The skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the upper arm depending on injection sites are shown in
Table 3, with the average (range) skin thickness 2.00±0.34 mm (range, 1.11 to 2.90 mm), subcutaneous fat thickness of 5.50±2.68 mm (range, 0.85 to 12.69 mm), and the total skin and subcutaneous fat thickness of 7.50±2.68 mm (range, 2.30 to 14.85 mm).
The thickest location of the skin in the upper arm was 2 for males and 1 for females, while the thinnest point was 8 for both. The skin thickness range was 0.90 to 3.60 mm and 0.80 to 3.10 mm for males and females, respectively.
The thickest point of the subcutaneous fat and the total thickness of skin and subcutaneous fat in the upper arm was 1 for males and 2 for females, while the thinnest point was 8 for both. The subcutaneous fat thickness range was 0.10 to 18.70 mm and 0.75 to 17.50 mm for males and females, respectively, and the total thickness of skin and subcutaneous fat range was 1.40 to 21.20 mm and 2.00 to 19.80 mm for males and females, respectively.
The differences in the skin and subcutaneous fat thicknesses
The differences in the skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the abdomen and upper arm depending on normal characteristics are shown in
Table 4. Our analysis indicated that the abdominal and brachial skin, subcutaneous fat and the total of the two were thicker in females compared to male (
P<0.05), as well as the thickness increasing with higher BMI (
P<0.05), with statistical significance. However, age, use of insulin, family history of diabetes, or complications due to diabetes did not show any significant relevance.
Factors influencing skin and subcutaneous fat thicknesses of the abdomen and upper arm depending on injection sites
In order to determine the influential factors for the skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the abdomen and upper arm, multiple regression analysis was performed with the identified factors that are related to this such as gender, age, and BMI as independent variables, as shown in
Table 5.
We found that the skin thickness of the abdomen and upper arm was higher in male and those with high BMI, with the explanatory power of adjusted R2 of 18.5% and 27.4% in the abdomen and upper arm, respectively. As for the subcutaneous fat thickness and the total skin and subcutaneous fat thickness, the thickness was positively correlated with gender (female) and high BMI in the abdomen, whereas it was positively correlated with gender (female), younger age, and high BMI in the upper arm. The explanatory power of adjusted R2 was 54.4% and 63.2% for the subcutaneous fat thickness of the abdomen and upper arm, respectively, and 55.8% and 61.3% for the total skin and subcutaneous fat thickness of the abdomen and upper arm, respectively.
Our analysis showed that the regression models related to the skin and subcutaneous fat thicknesses and skin-subcutaneous thickness of the abdomen and upper arm were statistically significant (P<0.001). Furthermore, factors that influence these variables such as gender, age, and BMI did not have autocorrelation, with Dubin-Watson statistics of 1.791 to 2.058, and the variation inflation factor was 1.005 to 1.010 which is lower than 10 and therefore suggest no issues with the multicollinearity of these variables. Thus we may conclude that the results of regression analyses are reliable.
The needle length-dependent possibility for the injection of insulin to the abdomen and upper arm
The possibility of insulin injection to the abdomen and upper arm depending on the needle length was determined by analyzing the intradermal and intramuscular risks, as shown in
Table 6.
Investigations revealed that there were no cases of intradermal injection of insulin either to the abdomen or to the upper arm for all needle lengths. Differently, of the 156 patients, 3 (1.9%), 8 (5.1%), 20 (12.8%), and 45 (28.8%) cases were reported to have injected insulin into the muscles for the 4-, 5-, 6-, and 8-needles, respectively, where the frequency of intramuscular injection using 8-mm needles were more than 10-fold higher than when using 4-mm needles in the abdomen. Furthermore, 5 (3.2%), 32 (20.5%), 55 (35.3%), and 92 (58.9%) cases were reported for the same problem when using 4-, 5-, 6-, and 8-mm needles, respectively, in the upper arm, which denotes much higher risks than injecting into the abdomen. Nonetheless, these results plainly show that the risk of intramuscular injection increases with longer needles in both the abdomen and upper arm.
DISCUSSION
The pain and complexities of an injection for insulin treatment notably reduces its compliance. Therefore, in an attempt to reduce pain and simplify the injection technique, short 4- or 5-mm needles were developed and applied to practical use, but domestic patients and nurses still tend to use the 8-mm needles. During an injection, insulin is injected into the dermis if the needle is shorter than the skin thickness, while it is injected into the muscles if the needle is longer than the total skin and subcutaneous fat thickness, which subsequently leads to problems in sugar control. For these reasons, the thicknesses of the skin and subcutaneous fat are important variables to consider when choosing the needle length and injection method. Therefore the purpose of this study stands to have great importance, which was to check the skin and subcutaneous fat thicknesses in the injection site and hence confirm the suitability of the newly developed short needles with Korean patients. However, this study failed to recruit a sufficient number of under-weight patients. Moreover we neglected the possibility of the variation in the skin and subcutaneous fat thicknesses depending on the right or left-handedness of our subjects and randomized the patients, measuring the thicknesses either on the right or left arm without putting this possibility into consideration. Still, bearing these limitations in mind, we may discuss some important facts about the results of this research.
The average thickness of the skin in the was 2.29 mm (2.37 mm for males and 2.20 mm for females) and 2.00 mm (2.14 mm in males and 1.84 mm in females) in the abdomen and upper arm, respectively. Our results are consistent to the research by Gibney et al. [
3] who reported an average skin thickness of 2.20 mm, and although the age group is different, it was also similar to the study conducted by Lo Presti et al. [
13] who reported average skin thicknesses of 2.18 and 1.92 mm in the abdomen and upper arm of 14 to 17 years old teenagers, respectively. Despite these similarities, our results were strangely dissimilar to other studies conducted with Korean subjects, where Choi et al. [
15] reported that the thicknesses of the skin were 1.57 mm and 1.53 to 1.57 mm in the abdomen and upper arm, respectively, and Park et al. [
20] showed 1.31 mm (1.28 mm in males and 1.37 mm in females) in the abdomen, whose results are both thinner compared to ours. On the contrary, a study by Jung et al. [
14] that was conducted with subjects more than 60 years old showed that the skin thicknesses were 2.97 and 2.16 mm in the abdomen and upper arm, respectively, which are thicker than our results.
There are various methods to estimate the skin thickness, such as histopathologic analysis, computed tomography, ultrasound imaging, and so forth. However, there are several downsides for each method. When creating tissue sections for histopathologic analysis, the spaces between collagen proteins expand, making the section look thicker than it actually is. Furthermore, low-frequency ultrasound imaging does not provide a clear image that the investigators fail to definitely identify the boundary between epidermis and dermis and therefore lead to inaccurate estimation of the skin thickness, and computed tomography imaging has the tendency of compressing the skin, hence leading to underestimated skin thickness. Considering these possible biases, the skin thickness measured by Park et al. [
20] using computed tomography were thinner, and those measured by Jung et al. [
14] using low-frequency ultrasound were thicker than our results. Yet, those measured by Choi et al. using high-frequency ultrasound were thinner, while the results of Gibney et al. were similar to ours. Collectively, we believe that by using 10 MHz ultrasound and altering the frequency in the range of 7 to 12 MHz depending on the clarity of epidermal-dermal boundary, our results nicely reflect the actual thickness. In addition, the thicknesses measured by Jung et al. [
14] varied from 1.99 to 4.59 mm depending on where it was measured, despite measuring the same abdomen. Our study also showed a variance of skin thickness depending on the measurement location, from 1.99 to 2.47 mm for the abdomen and from 1.69 to 2.28 mm for the upper arm. Unlike other studies that presented their data based on a single measurement, we measured the skin thickness from 10 different points for the abdomen and 8 different points for the upper arm and calculated the average. Thus we are confident that our results are accurate and have significant impact.
Here the skin thicknesses of both the abdomen and upper arm differed depending on gender and BMI, and although the skin of males were thicker than females and their thickness also increased with increasing BMI value within a certain range, their explanatory power was 18.5% and 27.4% for the abdomen and upper arm, respectively, which is not a very high value. Gibney et al. [
3] reported injection site, gender, BMI, and ethnicity as influential variables, considering that this study was conducted with a single ethnic group, this study supports the results of the present work. In detail, female skin was thicker than those of males, which is consistent to many other previous studies [
3,
15,
20]. As for age, we recognized it to be a non-important factor for skin thickness, but the conclusion for this variable differed among many other research. Park et al. [
20] reported that skin becomes thicker until when at a certain point it starts to thin down, but Jung et al. [
14] reports a reversed result where they suggest that old age group has thicker skin compared to young and middle age groups. Nevertheless many other research have reported in favor of the opinion that age was irrelevant to skin thickness [
3,
15,
21], and Shuster et al. [
21] have suggested that the collagen and substrates in dermis are lost with progressing age, but the rearrangement of dermal collagen maintains the skin thickness. Together, it is necessary to rethink the hypothesis regarding the correlation of age and skin thickness, and repeated experiments to confirm this is required.
BMI was identified as a factor affecting skin thickness in this research, where skin thickens with increasing BMI. Although this agrees with the results of Gibney et al. [
3], it also somewhat disagrees with the results of Choi et al. [
15] that suggests there is no significant relationship between the weight, one of the important variables for the calculation of BMI, and skin thickness. As weight increases, the cells that constitute the dermis becomes larger, and because the thickness of dermis is included in the calculation for the skin thickness, we speculate that skin thickness to be positively correlated to BMI. Further study to elucidate the underlying mechanisms behind the relationship between these two variables is necessary.
The average subcutaneous fat thickness was 10.15 mm (7.75 mm for male and 13.07 for female) and 5.50 mm (4.06 mm for male and 7.19 mm for female) for the abdomen and upper arm, respectively, denoting that female had thicker subcutaneous fat layer and that abdomen was thicker than upper arm. Although this is fairly consistent with the research conducted on American diabetic patients by Gibney et al. [
3] who reported that the subcutaneous fat thickness was 13.92 mm (12.3 mm for male and 15.9 mm for female) and 10.77 mm (8.4 mm for male and 13.7 mm for female) for the abdomen and upper arm, respectively, as well as being consistent with another research conducted with Korean diabetic patients by Jeong et al. [
18] who reported thicknesses of 16.8 mm (16.3 mm for male and 17.3 mm for female) for the abdomen, the thicknesses measured in this study are generally thinner.
The study by Gibney et al. [
3] was conducted in a different country to the present study, for which reason we speculate that dietary patterns and ethnic factors may have some effects on the end result. On the other hand, the study by Jeong et al. [
18] that was conducted in the same country was performed with patients residing in the province, which is very different to the current study that was performed with diabetic patients residing in Seoul and visiting a higher class general hospital. Hence we carefully suspect that, although the population-social factors and the extent of diabetes control was not thoroughly investigated, the quality of life and diabetes control quality may have affected the patients' weight, causing a decrease in subcutaneous fat thickness. Altogether, we encourage further study evaluating the effect of population-social factors and the extent of diabetes control on BMI or perhaps even on the actual subcutaneous fat thickness, and utilize those results, together with the results of this study, in the education for diabetes.
Our results revealed gender and BMI (explanatory power 54.4%) for abdomen, and age, gender, and BMI (explanatory power 63.2%) for upper arm as the influential factors for subcutaneous fat thickness. Here, we showed that, within a certain range, the subcutaneous fat thickness increased by 0.63 and 0.52 mm in the abdomen and upper arm, respectively, per 1 kg/m
2 increase in BMI, which is consistent to the data from Gibney et al. [
3] who showed that the thickness increased by 0.4 mm per 1 kg/m
2 increase in BMI, as well as the data from Joo and Sohng [
4] who reported that the thickness increased by 0.71 and 0.62 mm in males and females, respectively, per 1 kg/m
2 increase in BMI. As expected, the immediate relevance of BMI and subcutaneous fat thickness was very high like the many other domestically conducted studies [
16,
17]. Since obesity is highly associated with various metabolic diseases, especially diabetes, the importance of maintaining standard body weight to control blood glucose level as a diabetic patient must be emphasized.
Subcutaneous fat thickness is also easily affected by gender, where females had thicker subcutaneous fat layer compared to males, and this is highly consistent throughout many other research [
3,
22]. The reason why females have thicker subcutaneous fat layers compared to males is because surplus fat is generally stored as visceral fat for males, while it is generally stored in the subcutaneous fat layer or the limbs for females [
9], consequently giving rise to thicker subcutaneous fat layer in females compared to males. This implies that gender and BMI are crucial factors to be considered when selecting the appropriate needle length for subcutaneous and intramuscular injections.
Insulin must be injected into subcutaneous fat. Thus, it is essential for short needles to fully penetrate the skin to avoid intradermal injections of insulin. All subjects of this study were confirmed to have skins less than 4 mm thick, and another study that was also conducted in Korea by Choi et al. [
15] had the thickest skin yet to be reported, ranging from 2.77 to 3.87 mm for the abdomen. Therefore, including the commercially available 4-mm needle, all insulin syringe needles with different lengths are free of any risk of intradermal injections.
Assuming that insulin was injected at a right angle to the skin, the risk for intramuscular injections was evaluated for needles of different lengths, deeming a needle length longer than the total skin and subcutaneous fat thickness to be dangerous. As a result, the risks of intramuscular injections were 1.9%, 5.1%, 12.8%, and 28.8% for 4-, 5-, 6-, and 8-mm needles, respectively, for the abdomen, while they were 3.2%, 20.5%, 35.3%, and 58.9% for 4-, 5-, 6-, and 8-mm needles, respectively, for the upper arm, indicating that longer needles had higher risks of intramuscular injections. These results are also consistent to the study by Gibney et al. [
3] who also suggested that longer needles are tend to be at more risks of intramuscular injections, as well as the study by Lo Presti et al. [
13] which was conducted with teenagers. In particular, the total skin and subcutaneous fat thickness of different groups divided according to BMI were 5.80, 9.42, 13.07, 15.07, and 15.07 mm for the abdomen, and 4.61, 6.70, 7.20, 8.41, and 11.85 mm for the upper arm for under-weight, normal-weight, over-weight, obese, and extremely obese groups, respectively. Therefore, together with our analysis of maximum skin thickness, we can conclude that 4- and 5-mm needles for the abdomen and 4-mm needle for the upper arm are appropriate for injection at a right angle to the skin, free of intradermal or intramuscular injection risks, without having to inject at a 45-degree angle or making skinfolds. One drawback is that the subcutaneous fat thickness of the abdomen and upper arm varied depending on the injection site. In this study, the outer section of the abdomen had thinner subcutaneous fat than the middle section, whereas the upper part was thinner than the lower part of the upper arm. Of special note, for some patients in the under-weight group, even the 4-mm needle which is the shortest had a risk for intramuscular injections. Therefore, when treating the under-weight group, some injection skills may still be necessary such as injecting at a 45-degree angle or making skinfolds, despite using the shortest needle.
Pregnant patients diagnosed with gestational diabetes avoid injections to the abdomen and prefer to have insulin injections either to the upper arm or to the thigh in concern of their baby. In case of injecting insulin to the upper arm where the subcutaneous fat in relatively thin, special injection techniques such as injecting at a 45-degree angle or making skinfolds are necessary, but this is extremely difficult for the patients to perform by themselves. However, the results of this study indicated that the skin thickness of women in the upper arm was thinner than 4 mm while the total skin and subcutaneous fat thickness was thicker than 4 mm, pointing out that self-injections at a right angle to the skin is possible with short needles. Therefore we think that it is advisable to encourage pregnant patients with gestational diabetes to use short needled insulin syringes to make them more submissive to insulin treatment.
The number of old aged diabetic patients has been increasing recently [
7], along with the increase in the number of elderly living alone. The elderly also have issues with injecting at an angle or making skinfolds, so it is necessary to simplify the injection technique. In this regard, it is unnecessary to inject at an angle or make skinfolds when using short needles, so we hope that encouraging the usage of such short needles will make the elderly more compliant to insulin treatment.
In another aspect, Hauner et al. [
23] reported that 60% patients who do not change the injection site and 22% who do change the injection site but do so irregularly have lipodystrophy. Changing the injection site does not simply mean that the injection site must be changed, but the 'same time, same place' principle must be kept [
1]. According to a recent investigation, although the medical doctors instruct diabetic patients to take part in the education for diabetes, most patients do not follow [
24]. Even in the preliminary investigation of the present study, patients did not use the whole abdominal area to inject insulin, but mainly used the points 7, 8, 11, and 12 to inject insulin, and have explained that they did not use the whole abdominal area because it was inconvenient to inject on the outer area and also because they were in fear of injecting too deeply. We believe that our study which investigated the skin and subcutaneous fat thicknesses for each different injection sites on the abdomen and upper arm will be a strong supportive material in persuading patients to fully use the injection sites available and to do so in a consistently changing manner. Still, our study was conducted in only one hospital, and the number of patients less than 45 years old was 10.4%. For the generalization of our work, we propose further studies which repeat our study with expanded number of patients less than 45 years old as well as the number of hospitals. It would also be preferable to measure the skin and subcutaneous fat thicknesses of type 1 DM patients and children.
In conclusion, we presented our measurements of skin thickness and skin-subcutaneous thickness as a diagram so that it can be used as a basis for subcutaneous insulin injection. Furthermore, we investigated the risks of intradermal and intramuscular injections for needles of different lengths to evaluate the suitability and also the necessary or unnecessary techniques to be used with those needles. Our evaluations pinpoint the commercially available 4-mm long needles for usage by Korean diabetic patients. Overall this study will contribute immensely to the evidence-based decisions of appropriate needle length and injection sites for different diabetic patients.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download