Abstract
Background
The present study was designed to develop criteria for screening patients with type 2 diabetes mellitus (T2DM) for asymptomatic coronary artery disease (CAD).
Methods
A total of 213 patients with T2DM without typical angina or chest pain were studied between 2002 and 2007. We also evaluated 53 patients with T2DM who had reported chest discomfort using an exercise treadmill test (ETT).
Results
Thirty-one of the 213 asymptomatic patients had positive ETT results. We performed coronary angiography on 23 of the 31 patients with a positive ETT and found that 11 of them had significant coronary stenosis. The main differences between the patients with significant stenosis and those with a negative ETT were age (63.1±9.4 vs. 53.7±10.1 years, P=0.008) and duration of diabetes (16.0±7.5 vs. 5.5±5.7 years, P<0.001). The positive predictive value (PPV) of the ETT was calculated to be 47.8%. The PPV of the ETT increased to 87.5% in elderly patients (≥60 years) with a long duration of diabetes (≥10 years). The latter value is similar to that of patients with T2DM who presented with chest discomfort or exertional dyspnea. The PPV of the ETT in symptomatic patients was 76.9%.
In patients with type 2 diabetes mellitus (T2DM), coronary artery disease (CAD) is generally detected at an advanced stage with extensive atherosclerosis and poor outcomes, whereas CAD is commonly missed in the asymptomatic stage [1]. Diabetic patients with asymptomatic CAD have a higher cardiac mortality risk than those with symptomatic CAD [2]. In the largest autopsy study of diabetic patients without antemortem evidence of CAD, approximately 50% of patients under 65 years of age and 75% of those 65 years of age and older had high-grade coronary atherosclerosis [3].
Performing routine screening for asymptomatic CAD in all patients with T2DM is debatable for several reasons [4-8]; therefore, it is important to adopt appropriate criteria for selecting high risk patients who would benefit most from routine CAD screening. The CAD screening results may influence a physician's lifestyle advice for the patient, treatment targets for glycemia, blood pressure, or cholesterol, or decisions regarding the appropriateness of aspirin or angiotensin-converting enzyme inhibitor therapy [9]. CAD screening might identify individuals who could benefit from anti-ischemia therapy (β-blocker) or from revascularization, and specifically those with left main or severe multivessel disease [4].
In the present study, which involved asymptomatic patients with T2DM, we used the diagnostic approach of performing a coronary angiogram following a demonstration of myocardial ischemia during an exercise treadmill test (ETT). The present study was designed to develop criteria for screening patients with T2DM for asymptomatic coronary artery disease.
A total of 213 outpatients who underwent ETT were enrolled from St. Mary's Hospital Diabetes Clinics (Seoul, Korea) between March 2002 and November 2007. The exclusion criteria were type 1 or secondary diabetes, previous cardiovascular disease, typical angina or chest pain, resting electrocardiogram (ECG) signs of myocardial ischemia, and severe systemic disease with a poor prognosis. The diagnosis of T2DM was based on American Diabetes Association (ADA) criteria [10]. Patients with blood pressure over 140/90 mm Hg or those taking antihypertensive agents were recorded as being hypertensive (HBP). Diabetic nephropathy was defined as the appearance of abnormal urinary albumin levels: microalbuminuria (30-299 mg albumin/24 hr) or macroalbuminuria (>300 mg albumin/24 hr). We also analyzed 53 patients with T2DM who underwent an ETT to evaluate their chest discomfort (typical or atypical) or exertional dyspnea during the same period.
The ETT was performed following Bruce protocol. The study patients ceased taking beta blockers and calcium channel blockers 72 hours before the exercise test [11]. A 12-lead ECG was used and continuously monitored during the test, and blood pressure was recorded at rest and every 2 minutes during exercise and recovery. The ETT was considered positive when a horizontal or downsloping ST-segment with a depression ≥1 mm occurred 0.08 seconds after the J point. The test was considered equivocal when a ST segment depression<1 mm was observed, or when a left bundle branch block or premature ventricular beats >6 beats/min were seen. The test was considered inconclusive if the patient failed to reach 85% of the predicted maximal heart rate for his or her age. All subjects with a positive screening test underwent cardiology consultation.
Coronary angiography was performed only when the ETT was positive. We defined asymptomatic CAD as objective evidence of ischemia occurring in an asymptomatic patient during the ETT. We also defined flow-limiting CAD as a stenosis of more than 70% on coronary angiography. Coronary artery stenosis greater than 70% compared to pre-stenotic measurements was considered significant for CAD.
All blood samples were taken in the morning following a minimum 8-hour fast. Glycated hemoglobin (A1C) levels were determined by high-performance liquid chromatography (HLC-723 G7; Tosoh Co., Tokyo, Japan). Total cholesterol, triglycerides, and high density lipoprotein cholesterol (HDL-C) were determined using commercial kits.
All data were analyzed using SPSS version 10.0 for Windows statistical software (SPSS Inc., Chicago, IL, USA). The data are presented as mean±standard deviation, unless otherwise stated.
Patient characteristics were compared by presence or absence of symptoms using independent sample Student's t-tests for continuous measures and χ2 tests for categorical measures. Comparisons of the clinical and biochemical characteristics among the groups were made using ANOVA and post hoc analysis (Tukey test). P values <0.05 were considered statistically significant.
The baseline clinical characteristics of all asymptomatic and symptomatic patients are summarized in Table 1. The mean duration of diabetes was significantly longer in symptomatic patients versus those without symptoms (10.3±8.9 years vs. 6.4±6.5 years, P=0.004). The symptomatic patients had higher A1C levels (7.2±1.1% vs. 6.7±1.1%, P=0.010) and a greater prevalence of HBP (58.5% vs. 46.4%, P=0.063) and nephropathy (42.5% vs. 22.5%, P=0.005).
Fig. 1 shows the flowchart for patients who underwent an ETT. Eighteen patients (8.5%) were unable to complete the ETT; nine due to leg discomfort, five due to fatigue, three due to dyspnea, and one due to dizziness. Nine of the 195 completed tests were not considered diagnostic because either the upsloping ST segment depression or the horizontal ST segment depression was less than 1 mm. The remaining 186 completed tests provided data suitable for diagnosis and were subdivided into those having a positive ETT (n=31, 16.6%) and those having a negative ETT (n=155, 83.3%). All subjects with a positive screening test underwent cardiology consultation. Among the 31 patients with a positive treadmill test, two had no defects on the thallium scan and six patients refused further evaluation. The remaining 23 patients underwent coronary angiography. Coronary angiography revealed coronary stenosis ≥70% in eleven patients: three patients had one diseased vessel, seven had two diseased vessels, and one had three diseased vessels. Of the remaining twelve patients, one presented with a 50-70% lumen reduction and eleven had either a lumen reduction of <50% or no lumen reduction. The positive predictive value (PPV) for the ETT was calculated to be 47.8% (37.5% for men and 71% for women) (Fig. 2).
We divided the 213 patients into three groups. One group had negative ETT results (Group A). The second group had a positive ETT, but negative coronary angiography (Group B). This second group, therefore, had only a positive functional test. The third group had a positive ETT and positive coronary angiography, indicative of flow-limiting coronary artery disease (Group C).
Table 2 shows a comparison of the differences in variables for the three groups by ANOVA. The main differences between the 11 patients who presented with coronary lesions (Group C) and the 155 patients with a negative ETT (Group A) were age (63.1±9.4 years vs. 53.7±10.1 years, P=0.008) and duration of diabetes (16.0±7.5 years vs. 5.5±5.7 years, P<0.001). Serum A1C levels and lipid profiles were not significantly different among the three groups.
We determined that the main factors influencing the results of the ETT and coronary angiography were age and duration of diabetes. We arbitrarily selected an age of 60 years and a 10-year duration of diabetes as cut-off points. We examined how the results might change if the elderly patients with a long duration of diabetes underwent only an ETT. Fig. 3 shows the flowchart for the 29 elderly study patients with a long duration of diabetes who underwent only the ETT. Of these 29 patients who underwent an ETT, 4 (13.7%) were unable to complete the ETT. In addition, 2 of the 25 completed tests were not considered diagnostic, and the remaining 23 tests were considered suitable for diagnosis. Of the 23 suitable tests, almost half of them (n=10, 43.4%) had a positive ETT. Eight of the ten patients who had a positive ETT underwent coronary angiography, and 7 of the 8 had coronary stenosis greater than 70%. In this segment of our study population, the PPV using the ETT was 87.5% (Fig. 2).
We analyzed 53 study patients who underwent the ETT to evaluate their (typical or atypical) chest discomfort or exertional dyspnea. Among them, 9 patients (16.9%) were unable to complete the ETT. Four of the 44 completed tests were not considered diagnostic and the remaining 40 patients' tests were considered suitable for diagnosis. Seventeen patients (42.5%) had a positive ETT. Thirteen of the seventeen patients underwent coronary angiography and ten of the thirteen patients (three patients with one diseased vessel, four with two diseased vessels, and three with three diseased vessels) had coronary stenosis greater than 70%. In this study population, the PPV using the ETT was calculated to be 76.9% (Fig. 2).
We found the main differences between the asymptomatic patients with significant coronary stenosis and those with negative ETT to be duration of diabetes and age. The PPV of the ETT for predicting angiographic coronary disease was 48%. This value was found to be higher when the patients were elderly (≥60 years) and had a long duration of diabetes (≥10 years), or were symptomatic. To improve cost-effectiveness, screening for asymptomatic CAD could be limited to elderly patients with a duration of diabetes of 10 years or more.
As previously reported, even when a satisfactory ETT test is completed, the PPV in detecting silent coronary stenosis is low, between 40 and 60% [8,12,13]. In our study, the PPV of the ETT increased to 88% in elderly patients with a long duration of diabetes. This value was similar to that of type 2 diabetes mellitus patients who presented with chest discomfort or exertional dyspnea: the PPV of the ETT in symptomatic patients was 76.9%
The ETT is often not feasible for diabetic patients because their exercise capability may be impaired by peripheral vascular or neuropathic disease [14]. In our study, 18 patients (8.5%) were unable to complete the ETT, mostly due to leg discomfort or dyspnea. A completely normal ETT has been reported to be a marker for a good prognosis in patients with diabetes [14]. Compared with such imaging procedures as coronary computed tomography (CT), echocardiography, and stress single photon emission computed tomography myocardial perfusion imaging, the treadmill exercise test can be performed at a much lower cost. The ETT is preferable to a pharmacological stress test because it depicts the heart's actual workload and better simulates everyday cardiac strain [15]. Furthermore, patients are not exposed to ionizing radiation and contrast. Therefore, initially performing an ETT in patients who are able to exercise is recommended. The more recently developed non-invasive, multi-slice CT angiography is recommended for exclusion of coronary heart disease, but has the associated disadvantages of high radiation exposure and cost [14]. An estimated 1 in 270 women who underwent CT coronary angiography at age 40 will develop cancer from that CT scan, compared with an estimated 1 in 8,100 women who had a routine head CT scan at the same age [16]. For these reasons, we chose the ETT as a screening tool for coronary artery disease in asymptomatic patients with T2DM. Further studies will guide us with respect to which modality is most appropriate.
The 1998 ADA Consensus Development Conference on the diagnosis of coronary artery disease in people with diabetes recommended performing stress screening for coronary artery disease in asymptomatic patients with ≥2 cardiovascular risk factors (smoking, arterial hypertension, hypercholesterolemia, family history of premature CAD, microalbuminuria) [17]. Unfortunately, recent studies have shown that the presence of traditional categorical risk factors did not help to identify asymptomatic patients with a higher prevalence of coronary artery disease [18]. In the absence of symptomatic CAD, clinical features that help to identify patients with an increased risk for myocardial infarction or cardiac death include evidence of other atherosclerotic vascular disease, microalbuminuria and chronic kidney disease, autonomic neuropathy, retinopathy, hyperglycemia, abnormal resting ECGs, age, sex, and both traditional and novel cardiac risk factors [5]. However, the routine screening of asymptomatic patients with T2DM and normal ECGs remains controversial [19]. In our study, patients with significant coronary stenosis tended to have higher A1C levels and to have a greater prevalence of HBP and nephropathy, however, the difference was not statistically significant (HbA1C, 7.0% vs. 6.6%; HBP, 63.6% vs. 45.8%; Nephropathy, 37.5% vs. 20%). The size of our study population may have been too small to draw conclusions about the other covariates studied.
We found the main differences between the asymptomatic patients with significant coronary stenosis and those with a negative ETT were the duration of diabetes and age. It is well known that age is a strong predictor of CAD [5], however, duration of diabetes is not included among CAD predictors in the ADA recommendations [5]. Debate on the relationship between duration of diabetes and CAD continues, and several recent studies have reported a positive correlation [8,20].
Our study has several limitations. First, it used a retrospective design, which is prone to selection bias. Second, data on other traditional cardiovascular risk factors, such as smoking, family history of premature CAD, autonomic neuropathy and retinopathy were not available. Third, clinical features such as chronic kidney disease, hyperglycemia, and hypertension did not differ between the groups. The small number of subjects in our study may also be a limitation.
In conclusion, we recommend screening for coronary artery disease in elderly patients (≥60 years) with a duration of diabetes ≥10 years. Further studies are needed to evaluate the effectiveness of routine screening for asymptomatic CAD in this patient subgroup.
Figures and Tables
Fig. 2
Positive predictive values (PPV) of an exercise treadmill test (ETT) for coronary artery stenosis. DM, diabetes mellitus.
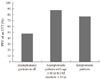
Fig. 3
Flowchart of elderly patients (≥60 years) with a long duration of diabetes (≥10 years). CAG, coronary angiography.

References
1. Alexander CM, Landsman PB, Teutsch SM. Diabetes mellitus, impaired fasting glucose, atherosclerotic risk factors, and prevalence of coronary heart disease. Am J Cardiol. 2000. 86:897–902.
2. Choi EK, Koo BK, Kim HS, Cho YM, Kang HJ, Cho YS, Chung WY, Chae IH, Choi DJ, Oh BH, Park YB, Choi YS. Prognostic significance of asymptomatic coronary artery disease in patients with diabetes and need for early revascularization therapy. Diabet Med. 2007. 24:1003–1011.
3. Goraya TY, Leibson CL, Palumbo PJ, Weston SA, Killian JM, Pfeifer EA, Jacobsen SJ, Frye RL, Roger VL. Coronary atherosclerosis in diabetes mellitus: a population-based autopsy study. J Am Coll Cardiol. 2002. 40:946–953.
4. Rutter MK, Nesto RW. The changing costs and benefits of screening for asymptomatic coronary heart disease in patients with diabetes. Nat Clin Pract Endocrinol Metab. 2007. 3:26–35.
5. Bax JJ, Young LH, Frye RL, Bonow RO, Steinberg HO, Barrett EJ. ADA. Screening for coronary artery disease in patients with diabetes. Diabetes Care. 2007. 30:2729–2736.
6. Bacci S, Villella M, Villella A, Langialonga T, Grilli M, Rauseo A, Mastroianno S, De Cosmo S, Fanelli R, Trischitta V. Screening for silent myocardial ischaemia in type 2 diabetic patients with additional atherogenic risk factors: applicability and accuracy of the exercise stress test. Eur J Endocrinol. 2002. 147:649–654.
7. Araz M, Celen Z, Akdemir I, Okan V. Frequency of silent myocardial ischemia in type 2 diabetic patients and the relation with poor glycemic control. Acta Diabetol. 2004. 41:38–43.
8. Janand-Delenne B, Savin B, Habib G, Bory M, Vague P, Lassmann-Vague V. Silent myocardial ischemia in patients with diabetes: who to screen. Diabetes Care. 1999. 22:1396–1400.
9. Buse JB, Ginsberg HN, Bakris GL, Clark NG, Costa F, Eckel R, Fonseca V, Gerstein HC, Grundy S, Nesto RW, Pignone MP, Plutzky J, Porte D, Redberg R, Stitzel KF, Stone NJ. American Heart Association. American Diabetes Association. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation. 2007. 115:114–126.
10. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2003. 26:Suppl 1. S5–S20.
11. Gibbons RJ, Balady GJ, Beasley JW, Bricker JT, Duvernoy WF, Froelicher VF, Mark DB, Marwick TH, McCallister BD, Thompson PD Jr, Winters WL, Yanowitz FG, Ritchie JL, Gibbons RJ, Cheitlin MD, Eagle KA, Gardner TJ, Garson A Jr, Lewis RP, O'Rourke RA, Ryan TJ. ACC/AHA Guidelines for Exercise Testing. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing). J Am Coll Cardiol. 1997. 30:260–311.
12. Penfornis A, Zimmermann C, Boumal D, Sabbah A, Meneveau N, Gaultier-Bourgeois S, Bassand JP, Bernard Y. Use of dobutamine stress echocardiography in detecting silent myocardial ischaemia in asymptomatic diabetic patients: a comparison with thallium scintigraphy and exercise testing. Diabet Med. 2001. 18:900–905.
13. Valensi P, Sachs RN, Lormeau B, Taupin JM, Ouzan J, Blasco A, Nitenberg A, Metz D, Paries J, Talvard O, Leutenegger M, Attali JR. Silent myocardial ischaemia and left ventricle hypertrophy in diabetic patients. Diabetes Metab. 1997. 23:409–416.
14. Djaberi R, Beishuizen ED, Pereira AM, Rabelink TJ, Smit JW, Tamsma JT, Huisman MV, Jukema JW. Non-invasive cardiac imaging techniques and vascular tools for the assessment of cardiovascular disease in type 2 diabetes mellitus. Diabetologia. 2008. 51:1581–1593.
15. Xanthos T, Ekmektzoglou KA, Papadimitriou L. Reviewing myocardial silent ischemia: specific patient subgroups. Int J Cardiol. 2008. 124:139–148.
16. Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de Gonzalez A, Miglioretti DL. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009. 169:2078–2086.
17. American Diabetes Association. Consensus Development Conference on the diagnosis of coronary heart disease in people with diabetes: 10-11 February 1998, Miami, Florida. Diabetes Care. 1998. 21:1551–1559.
18. Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A. Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus. J Am Coll Cardiol. 2006. 47:65–71.
19. American Diabetes Association. Standards of medical care in diabetes--2009. Diabetes Care. 2009. 32:Suppl 1. S13–S61.
20. Yoo WS, Kim HJ, Kim D, Lee MY, Chung HK. Early detection of asymptomatic coronary artery disease in patients with type 2 diabetes mellitus. Korean J Intern Med. 2009. 24:183–189.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download