Abstract
Background
Our study group established "3H care" in 2002. The meaning of "3H care" attain and maintain adequate controls over hypertension, hyperlipidemia, and hyperglycemia in type 2 diabetic patients. This study evaluated the achievement of target goals after one year or more of "3H care" by specialists in our diabetic clinic.
Methods
This was a retrospective study of 200 type 2 diabetic patients who received "3H care" for one year or more in our diabetic clinic. We evaluated achievement of target goals for metabolic controls as suggested by the American Diabetes Association.
Results
Overall, 200 type 2 diabetes patients were enrolled, of whom 106 were males (53%) and 94 were females (47%). After one year of "3H care," the mean HbA1c was 7.2±1.5% and the percentage of patients achieving glycemic control (HbA1c <7%) was 51.8%. However only 32.2% of hypertensive patients achieved the recommended target. After one year of "3H care," the percentages of those who achieved the target value for dyslipidemia were 80.0% for total cholesterol, 66.3% for low density lipoprotein cholesterol, 57.9% for triglyceride, and 51.8% for high density lipoprotein cholesterol. The percentage that achieved all three targets level was only 4.4% after one year and 14.8% after two years.
Conclusion
The results of this study demonstrate that only a minor proportion of patients with type 2 diabetes achieved the recommended goals despite the implementation of "3H care." It is our suggestion that better treatment strategies and methods should be used to control hypertension, hyperlipidemia and hyperglycemia.
Cardiovascular disease is the leading cause of morbidity and mortality in diabetic patients, and among risk factors of cardiovascular disease, diabetes is considered to be comparable to cardiovascular disease [1-6]. One large-scale prospective study on diabetes, the UK Prospective Diabetes Study (UKPDS), reported that aggressive blood glucose control resulted in a decrease in microvascular complications, and though macrovascular complications were not significantly reduced and showed that the prevention of cardiovascular disease through blood glucose control alone was insufficient [7-9]. Additionally, in The Action to Control Cardiovascular Risk in Diabetes (ACCORD) and The Action in Diabetes and Vascular Disease (ADVANCE) studies, strict blood glucose control reduced the incidences of microvascular complications, particularly diabetic nephropathy. Although this reduction was significant, and reduces the risk of cardiovascular disease, we concluded that there were relatively fewer contributing risk factors of cardiovascular disease [10,11]. Steno-2 study results showed that the risk of microvascular complications and macrovascular complications can be reduced through integrated diabetes management [12]. When the results of the above study were summarized, the prevention of diabetic complications was shown to require integrated management that maintained cardiometabolic risk factors such as dyslipidemia and hypertension, in addition to fundamental blood glucose management.
Starting in 2002, our research group established the "3H care" concept in order to ideally manage hypertension, hyperlipidemia, and hyperglycemia in type 2 diabetic patients. Based on these concepts, the accompaniment of hypertension and dyslipidemia with the diagnosis of diabetes was confirmed. In addition, when hypertension and dyslipidemia existed in combination, combination that were treated equally hyperglycemia maintenance, patient education were perfomed, and necessary drugs were administered. During follow-up, the two associated conditions were managed to hyperglycemia identically. The importance of managing the aforementioned risk factors is already known, and it has been reported that the actual treatment of individual risk factors does not result in the satisfactory achievement of target goals [13-17]. Our research group performed "3H care" on type 2 diabetic patients for one year, and analyzed blood glucose, blood pressure, and the goal lipid levels at the end of the study period. Additionally, to analyze patients who were tracked for two years, a performance evaluation of 3H care was performed, from which it was determined that additional data to complement the maintenance method is required. It has been reported that the prevalence of metabolic syndrome is high in type 2 diabetic patients, and type 2 diabetes in combination with metabolic syndrome is known to increase mortality [18-20]. In this study, the prevalence of metabolic syndrome was investigated. This study was not based on specifically established guidelines or algorithms, and two endocrinology specialists performed treatment based on their own discretion and the clinical circumstances of each individual patient.
This study was performed for three years from September 1, 2004 to August 8, 2007 at a university hospital diabetes center. The patients who were registered as having type 2 diabetes and excluding those with chronic renal failure, malignant tumors, 1,892 participants visited the outpatient clinic and received medical care for one year. During the one year follow-up period with the applicable patients at least three outpatient visits were performed, during which blood pressure, HbA1c, lipid levels, and weight were measured. A total of 200 patients were analyzed (106 men, 94 women). All clinical data was from medical records and was used to conduct a retrospective study.
Subject gender, age, body mass index (BMI), duration of diabetes, cardiovascular disease history, diabetes treatment method, and the number of blood pressure control drugs used were analyzed, and the measured glycated hemoglobin (HbA1c), blood pressure, and lipid conditions were examined in the initial and most recent visits, based on these results each goal was investigated after one year. High blood pressure patients were defined as drug therapy recipients with a blood pressure ≥130/80 mm Hg, hyperlipidemia was defined as total cholesterol ≥200 mg/dL, low density lipoprotein cholesterol (LDL-C) was defined at levels ≥100 mg/dL, high density lipoprotein cholesterol (HDL-C) in men was defined as a level ≤40 mg/dL, and in women as a level ≤50 mg/dL in patients receiving drug treatment. Additionally, regardless of the number of visits to the outpatient clinic, in order to compare the indicators from the 135 (67.5%) patients who were followed for two years, the success percentage was investigated each year. Height and weight were measured directly by trained nurses after patients disrobed and removed their shoes, and BMI was calculated during the hospital visit by dividing the measured weight (kg) by the squared height (m2). After allowing the blood pressure to stabilize for ten minutes, a mercury sphygmomanometer was used on the seated patients to measure their systolic and diastolic blood pressure. The diabetes treatment methods were separated into four parts: diet, oral hypoglycemic agents, insulin monotreatment, insulin and oral hypoglycemic agents. Hyperglycemia management goals were HbA1c less than 7%, systolic blood pressure <130 mm Hg, and diastolic blood pressure <80 mm Hg. Total cholesterol less than 200 mg/dL, LDL-C less than 100 mg/dL, triglycerides less than 150 mg/dL, HDL-C greater than 40 mg/dL in men, and over 50 mg/dL in women were set. In this study total cholesterol and HDL-C were measured using the enzymatic colorimetry test method, triglycerides were measured using the glycerol elimination method, and LDL-C was measured using the homogenous enzymatic colorimetric test. Glycated hemoglobin was measured using high performance liquid chromatography (Tosoh, Tokyo, Japan); the normal range in our hospital was 3.9% to 6.1%. During the initial patent visit, insulin was measured in 62.5% (125) patients, and C-peptide was measured in 70.5% (141) patients. Those figures could not be investigated one or two years later. The patient management goals were established in accordance with the guidelines of the American Diabetes Association [21]. Since this study was a retrospective study of routine medical care circumstances, the differences in patient compliance to treatment were objectified and, could not be stated clearly.
All data was expressed as mean±standard deviation, and SPSS version 14.0 (SPSS Inc., Chicago, IL, USA) was used to perform all statistical analysis. The comparison among the blood glucose, blood pressure, and lipid control groups, were analyzed using t-tests and chi-square tests; treatment success comparisons were analyzed using ANOVA repeated measurements with a significance level was set at P<0.05.
The National Cholesterol Education Program (NCEP)-ATP III criteria [22] were used to diagnose metabolic syndrome, and instead of measuring waist circumference, the World Health Organization (WHO) [23] criteria for BMI were in addition to the standard Asian obesity criteria, BMI ≥25 kg/m2. Because this study is one among many studies on type 2 diabetes patients, when the NCEP-ATP III diagnostic criteria [22] for hyperglycemia were assumed to be satisfied, and when more than two of other NCEP-ATP III criteria were met, patients were diagnosed with metabolic syndrome.
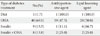
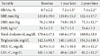
Among the 200 patients analyzed in this study, 106 were male, and 94 were female. The mean patient age was 56.0±11.3, and the mean BMI was 24.3±3.5 kg/m2. Among the participants, 43.0% were classified as obese, possessing a BMI greater than 25 kg/m2. Among the patients, 29.0% were first diagnosed with diabetes during this study, and 27.0% had been diagnosed with diabetes duration more than ten years prior. In addition 45.0% of patients had been diagnosed with hypertension, 40.0% of patients had been diagnosed with hyperlipidemia, and 20.5% of patients had been diagnosed with both. Initially 30.0% of the patients did not have hypertension or hyperlipidemia and 20.0% of patients had an HbA1c level greater than 10.0% at the first visit (Table 1). This study was conducted for one year by diabetes specialists on 200 patients who were receiving diabetes treatment. After two years, 135 patients had been retained for follow up.
Of the original 135 patients who had followed-up, 51.8% had reached their goal of maintaining an HbA1c level less than 7.0% after one year (Fig. 1), at which time, 25.5% of patients had the necessary glycated hemoglobin level needed to establish blood glucose control (greater than 8%). Among these patients, the percentage with glycated hemoglobin levels greater than 10% had increased to 7.5%. There were no differences in age and BMI based on analyzed results of patient characteristics under the target 7% HbA1c. Among the 106 male participants, 62 (58.4%) reached their treatment goal, and among the 94 female participants, 42 (44.6%) reached their treatment goal, demonstrating that male patients had a higher rate of success (P=0.035). Additionally, as glycated hemoglobin levels were lower initially, the treatment goal success rate increased (P<0.001). The average time since diagnosis of the patient group who reached their treatment goal was 4.6±7.1 years and the average time since diagnosis of the patient group who failed to reach their treatment goal was 8.0±8.9 years. The shorter was the time since diagnosis, the higher was the treatment success rate (P=0.003) (Table 2). In this study, diet, oral hypoglycemic agents, insulin monotherapy, and insulin and oral hypoglycemic agent combination therapy were divided into four groups, and the mean glycated hemoglobin levels of each group were compared. The mean level of the diet group was 6.0±0.4%, that of the oral hypoglycemic agent group was 6.8±2.2%, that of the insulin monotherapy group was 7.9±2.5%, and that of the insulin and oral hypoglycemic agent combination therapy group was 8.3±4.1%. When the treatment methods of the 58 (29.0%) type 2 diabetes patients who were diagnosed with diabetes for the first time were examined, the results for diet, oral hypoglycemic agents, insulin monotherapy, and insulin and oral hypoglycemic agent combination therapy, were 1.7%, 69.0%, 15.5%, and 13.8%, respectively (Table 3).
Among the participants in this study, 45% (n=90) had hypertension, and 32.2% of these patients had reached their treatment goals after one year, and 64% of the participants were taking one type of antihypertensive drugs, 32% were taking two types of antihypertensive drugs, and 4% were taking three or more antihypertensive drugs. The percentage of treatment success in patients who were taking only one type of antihypertensive drug was high. After one year, 32.2% of patients had reached their treatment goals. Among the 46 male participants, 11 (23.9%) reached their treatment goals, and among the 44 female participants, 18 (40.9%) reached their treatment goals. Females were more likely to achieve their treatment goals (P=0.025). In addition, success rates appeared to be independent of age, BMI, HbA1c levels, and lipid treatment goals (Table 4).
Initially, 40% (n=80) of the participants had dyslipidemia, and during the one year observation period, 7.5% (n=15) were newly diagnosed with dyslipidemia. The types of therapeutic drugs used to achieve lipid control were statin (n=67), fenofibrate (n=12), and statin and ezetimibe (n=1). Also, there were two cases in which treatment was changed from fenofibrate to statin during the observation period. In patients with dyslipidemia, the management goal success rate after one year was 80% for total cholesterol (<200 mg/dL), while those of LDL-C (<100 mg/dL), triglycerides (<150 mg/dL), and HDL-C (>40 mg/dL in males, >50 mg/dL) were 66.3%, 57.9%, and 51.8%, respectively. The percentage of patients who reached their serum lipid level goals after one year were 78.0%, 63.0%, 67.0%, and 50% in each group, respectively. When the characteristics of the patients who had reached their treatment goals were examined, as age increased, success rate increased, and treatment goals were relatively unaffected by gender, BMI, and hypertension. The average HbA1c of patients who had reached their target was 6.8±1.0%, and the mean HbA1c of patients who had failed to reach their goal was 7.2±1.4%. The average HbA1c of patients who had reached their goal was lower than those who had failed to reach their goal, indicating that the number of patients who had good blood glucose or hyperlipidemia control was not statistically significant (P=0.197) (Table 4).
Of the total 200 participants, 135 (67.5%) were followed-up for a two year period. Comparing the indicators of the 135 patients at the start of the treatment with those, one and two years after, the average HbA1c improved from 8.7±2.2% at the start of treatment to 7.2±1.5% after one year, and to 7.4±2.2% after two years (P<0.001) (Table 5). Compared to the changes in HbA1c, BMI, and systolic blood pressure showed no significant changes, diastolic blood pressure, total cholesterol, and LDL-C were reduced, and HDL-C increased significantly. However, triglyceride levels increased in the 135 patients who underwent two years of follow-up (Table 5). Two years after the "3H care," 57% of the 135 follow-up patients had reached their blood pressure goals, which was an improvement from that at the one year mark. The dyslipidemia success results showed that the cholesterol goal (<200 mg/dL) was achieved in 85.1% of patients and that for LDL-C (<100 mg/dL) was reached by 71.8%. The percentages of patients achieving triglyceride (<150 mg/dL) and HDL-C goals were 64.5% and 64%, respectively, and the two year follow-up showed a much higher achievement percentage than that at the one year follow up. The percentage of patients who had reached their goals for blood pressure and dyslipidemia were higher after two years than they were after one year, and patients who had reached their HbA1c goals were 51.8% after one year, and 43.7% after two years, showing a decreasing pattern. In addition, 4.4% (n=6) of patients had combination hyperglycemia, hypertension, and dyslipidemia after one year compared to 14.8% (n=20) after two years (Fig. 1).
Of the type 2 diabetes patients in this study, through 127 (63.5%) were diagnosed with metabolic syndrome according to the NCEP-ATP III (using BMI instead of waist circumference for diagnostic criteria). The prevalence of metabolic syndrome in males was 59.4% in male and 68.0% in females. When all patients were analyzed, the mean number of metabolic syndrome elements were 1.8±1.1, and only 12% of patients had only diabetes elements, while 25.5% had one element, 34.5% had two elements, 22.0% had three elements, and 6.0% had four elements. In patients with metabolic syndrome, the prevalence of each component of metabolic syndrome was: 49.5% for hypertension, 37.5% for hypertriglyceridemia, 56.0% for low HDL-C hyperlipidemia, 43.0% for Obese. Low HDL-C hyperlipidemia was the most common element of metabolic syndrome. Hypertension and hypertriglyceridemia were more prevalent in male patients, and low HDL-C hyperlipidemia had a higher prevalence in females. There was no difference in HbA1c level between the two groups based on the presence of metabolic syndrome. The prevalence of metabolic syndrome based on the duration of diabetes showed that prevalence increased with duration, although the association was not statistically significant. After one year, the HbA1c levels in the metabolic syndrome group and non-metabolic syndrome group were reduced from 8.6±1.8% to 7.4±1.4%, and from 8.6±2.7% to 7.1±1.8%, respectively. Blood pressure, triglyceride level, total cholesterol, and LDL-C were all reduced but HDL-C showed no change in the metabolic syndrome group. In the non-metabolic syndrome group, LDL-C was reduced or showed no significant change, and the triglyceride level increased (P<0.001).
Due to the increase in blood glucose levels and cardiometabolic risk factors in type 2 diabetes patients, the risk of developing microvascular and macrovascular complications tend to increase. To prevent complications from diabetes in addition to blood glucose control, the importance of the management of cardiometabolic risk factors such as dyslipidemia and hypertension has been emphasized. However, there are not many studies on how well it has actually been managed, and several studies have reported that actual medical care goal percentages could not be satisfied. In this study, 51.8% of patients reached their HbA1c goal of less than 7.0%, a lower number than was expected. When this study was compared with studies from other countries, the results reported by Harris et al. [24] showed that 44.6% of patients had reached the target of and HbA1c less than 7.0%. In the American National Health and Nutrition Examination Survey (NHANES) [25], 57.1% of patients had reached the target HbA1c of less than 7.0%. In a reports by Liebl et al. [26] involving data from eight countries based on the European Diabetes Policy Group Guidelines, 31% had an HbA1c less than 6.5% and in reports by Sone et al. [27] from Japan, 29.3% had an HbA1c less than 7.0%. In a South Korean study performed by Park et al. [17], 35.7% of patients reached their goal of an HbA1c less than 7.0%, and Lee et al. [28] reported a success rate of 49.2%. These results were similar to or lower than the results in the presenting study.
When the characteristics of patients who had reached their target for glycemic control and patients who had not reached their target for glycemic control were compared, the target success rate in males in this study was high, unlike that reported by Lee et al. [28], while other studies have shown no differences between men and women, regarding increases in BMI or increasing effect of smoking on HbA1c [17,25-27]. Despite strict intensive care, HbA1c increased over time, in a previous study [8]. In the present study, the mean duration of diabetes in patients who successfully reached their treatment goals was 4.6±7.1 years, and the mean duration in patients who did not reached their treatment goal was 8.0±8.9 years. The shorter was the duration of diabetes, the higher was the treatment success rate (P=0.003) (Table 2).
When the level of glycemic control based on diabetes treatment was examined, the investigation of type 2 diabetes treatment in the European CODE-II study [26] reported that the mean glycated hemoglobin levels of the diet and exercise, administration of oral hypoglycemic agents, and insulin monotreatment and insulin and hypoglycemic agent groups were 6.7%, 7.5%, and 8.1%, respectively. In the present study, diet, oral hypoglycemic agents, insulin monotherapy, and insulin and oral hypoglycemic agent combination therapy were considered as four individual trait groups. When the mean glycated hemoglobin values of each was compared, the results showed that the diet group had a value of 6.0±0.4%, that of the oral hypoglycemic agents group was 6.8±2.2%, that of the insulin monotherapy group was 7.9±2.5%, and that of the insulin and oral hypoglycemic agents combination therapy group was 8.3±4.1%. Glycemic control becomes more difficult as diabetes progresses, and the necessity for additional drug actions can be seen. Of the total participants 45% (n=90) had hypertension, and similarly, 20% to 60% of patients had diabetes with hypertension. In the one year follow-up focused on target success among hypertension patients, 32.2% reached their target. In the reports of the tertiary hospital-based study of Lim et al. [13], 43.2% of patients who had taken antihypertensive drugs had a blood pressure below the target 130/85 mm Hg, a lower than expected result which prompted consideration of target lower in. In the present study 44.5% of all patients had under 130/80 mm Hg, which was similar to the 45.5% reported by the NHANES. When the two year follow-up results were examined, 57% of patients had achieved their two year "3H care." These results were compared with the one year follow-up results, to determine whether a higher success rate had been achieved, based on management efforts and demonstrated that the target blood pressure was more achievable.
In patients with dyslipidemia, after one year of management, the success rate for total cholesterol in patients was 80%, and those of LDL-C, triglycerides, HDL-C were 66.3%, 57.9%, and 51.8%, respectively. These results were higher than the 56.6% for total cholesterol and 35.7% for LDL-C reported by Lim et al. [13] in their study on dyslipidemia patients at a tertiary hospital. After one year, the plasma lipid levels in all patient groups were 78.0%, 63.0%, 67.0%, and 50.0%, respectively, which were higher than that reported by the NHANES [25]: 46.5% LDL-C, 46.6% triglycerides, and 58.0% HDL-C. The LDL-C success rate in our study was also greater than that of the NHANES, which was 51.0%. Due to the nature of the participants in the present study, the use of aggressive lipid-lowering drugs and appropriate monitoring devices from the diabetes clinic specialist is believed to have contributed to this success rate. Despite undergoing aggressive drug therapies for hyperglycemia, hypertension, and dyslipidemia during the two year experimental period, the final results are not significantly different from the reports after one year of treatment. Therefore, after a maximum of one year of close observation, the introduction of more aggressive therapy is thought to be necessary for patients who are unable to reach their targets. In addition, the success rate of hypertension, dyslipidemia, and high blood sugar treatments was only 4.4% (n=6) after one year, and 14.8% (n=20) after two years. In order to reduce mortality from microvascular and macrovascular complications, these three conditions must be simultaneously managed, and to achieve target levels, various treatment may be necessary. Additionally, 32.5% (n=65) of the original participants in this study did not finish the study, which was similar to the dropout rate from another studies [27]. Such high dropout rates make continuous integrated treatments impossible, and since this deteriorates the quality of diabetes management, encouraging patients to continue with their treatment is important.
The components of metabolic syndrome typically accompany type 2 diabetes, which is clinically important due to the increased risk of cardiovascular disease in patients with diabetes [18-20]. The prevalence of metabolic syndrome in the participants of this study was 63.5%, lower than the 82.6% found using the International Diabetes Federation (IDF) criteria in German type 2 diabetes patients [29] and that of the prevalence of metabolic syndrome in diabetes patients older than 50 years from the NHANES [25], and similar to the 65.9% prevalence of metabolic syndrome in Hong Kong diabetes patients [30]. In a study performed in 2006 by Kim et al. [31] on Korean metabolic syndrome patients, the prevalence of metabolic syndrome in type 2 diabetes patients was 77.9%, which was higher than what was reported by the present study. Tong et al. [30] reported that diabetes patients with metabolic syndrome are more at risk for cardiovascular disease than diabetes patients without metabolic syndrome. Therefore, identifying the presence of metabolic syndrome in type 2 diabetes patients is an important step in treatment.
There were several limitations in this study. This study was performed at one center and the study did not include a large variety or a large number of patients. In addition in the two year follow-up, 65 patients dropped out and their data could not be used. Therefore, in the future, a larger scale study will be required to establish the success rates and complications of metabolic syndrome in type 2 diabetes patients. In conclusion, this study showed the current situation of type 2 diabetes patients who are receiving treatment from endocrinologists at a single university hospital, and the results of the one year of "3H care" show that 48.2% of cases with hyperglycemia, 55.5% of cases with hypertension, and 32% to 50% of cases with dyslipidemia had not reached their targets. The results from two years of "3H care" yielded similar results. The results were slightly improved compared to those of several previous studies however, the improvement did not reach a satisfactory level. Also, more research and clinical effort will be requied to achieve the targets of hyperglycemia, hypertension, and dyslipidemia.
Figures and Tables
Fig. 1
Proportion of patients reaching the therapeutic goals at baseline and one and two years later. Baseline includes only patients who were followed-up until the end of the second year. BP, blood pressure; TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; TG, >triglyceride; HDL-C, high density lipoprotein cholesterol (HDL-C >40 mg/dL [male], HDL-C >50 mg/dL [female]). aP<0.001.

Table 4
Characteristics of study subjects according to their achievement of blood pressure and lipid control

References
1. Savage PJ. Cardiovascular complications of diabetes mellitus: what we know and what we need to know about their prevention. Ann Intern Med. 1996. 124(1 Pt 2):123–126.
2. Barrett-Connor EL, Cohn BA, Wingard DL, Edelstein SL. The Rancho Bernardo Study. Why is diabetes mellitus a stronger risk factor for fatal ischemic heart disease in women than in men? JAMA. 1991. 265:627–631.
3. Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998. 339:229–234.
4. Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979. 241:2035–2038.
5. Comaschi M, Coscelli C, Cucinotta D, Malini P, Manzato E, Nicolucci A. SFIDA Study Group--Italian Association of Diabetologists (AMD). Cardiovascular risk factors and metabolic control in type 2 diabetic subjects attending outpatient clinics in Italy: the SFIDA (survey of risk factors in Italian diabetic subjects by AMD) study. Nutr Metab Cardiovasc Dis. 2005. 15:204–211.
6. Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med. 1993. 329:304–309.
7. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000. 321:405–412.
8. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998. 352:837–853.
9. UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998. 352:854–865.
10. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008. 358:2560–2572.
11. Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008. 358:2545–2559.
12. Park SW, Kim DJ, Min KW, Baik SH, Choi KM, Park IB, Park JH, Son HS, Ahn CW, Oh JY, Lee J, Chung CH, Kim J, Kim H. Current status of diabetes management in Korea using national health insurance database. J Korean Diabetes Assoc. 2007. 31:362–367.
13. Lim DJ, Kwon HS, Kim HS, Lee JH, Ko SH, Lee JM, Kim SR, Lee WC, Son HS, Cha BY, Lee KW, Son HY, Kang SK, Yoon KH. Clinical characteristics of the diabetic patients managed at the different medical institutions in Seoul and Gyeonggi province. Korean J Med. 2006. 71:173–181.
14. Rhee SY, Kim YS, Oh S, Choi WH, Park JE, Jeong WJ. Diabcare Asia 2001--Korea country report on outcome data and analysis. Korean J Intern Med. 2005. 20:48–54.
15. Kim SA, Park WS, Ohrr HC, Kang HY, Lee DH, Yi SW, Kwak YH, Song JS. Prevalence and management status of diabetes mellitus in Korea. Korean J Med. 2005. 68:10–17.
16. Lee YS. The current status of type 2 diabetes management at a university hospital. Korean Diabetes J. 2009. 33:241–250.
17. Park JH, Kim KW, Kang EJ, Kim TY, Lee SR, Bae SC, Kim MK, Choi SY, Park JH. Evaluation of glycemic control in type 2 diabetic patients have been treated in general hospital. J Korean Diabetes Assoc. 2004. 28:208–218.
18. Bonora E, Targher G, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, Saggiani F, Poli M, Perbellini S, Raffaelli A, Gemma L, Santi L, Bonadonna RC, Muggeo M. The Metabolic Syndrome is an independent predictor of cardiovascular disease in type 2 diabetic subjects. Prospective data from the Verona Diabetes Complications Study. Diabet Med. 2004. 21:52–58.
19. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005. 28:1769–1778.
20. Alexander CM, Landsman PB, Teutsch SM, Haffner SM. Third National Health and Nutrition Examination Survey (NHANES III). National Cholesterol Education Program (NCEP). NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes. 2003. 52:1210–1214.
21. American Diabetes Association. Standards of medical care in diabetes--2008. Diabetes Care. 2008. 31:Suppl 1. S12–S54.
22. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001. 285:2486–2497.
23. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998. 15:539–553.
24. Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999. 22:403–408.
25. Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS. Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Am J Med. 2009. 122:443–453.
26. Liebl A, Mata M, Eschwege E. ODE-2 Advisory Board. Evaluation of risk factors for development of complications in type II diabetes in Europe. Diabetologia. 2002. 45:S23–S28.
27. Sone H, Kawai K, Takagi H, Yamada N, Kobayashi M. Outcome of one-year of specialist care of patients with type 2 diabetes: a multi-center prospective survey (JDDM 2). Intern Med. 2006. 45:589–597.
28. Lee JE, Park HA, Kang JH, Lee SH, Cho YG, Song HR, Kim SW, Lee JS. State of diabetes care in Korean adults: according to the American Diabetes Association Recommendations. J Korean Acad Fam Med. 2008. 29:658–667.
29. Koehler C, Ott P, Benke I, Hanefeld M. DIG Study Group. Comparison of the prevalence of the metabolic syndrome by WHO, AHA/NHLBI, and IDF definitions in a German population with type 2 diabetes: the Diabetes in Germany (DIG) Study. Horm Metab Res. 2007. 39:632–635.
30. Tong PC, Kong AP, So WY, Yang X, Ho CS, Ma RC, Ozaki R, Chow CC, Lam CW, Chan JC, Cockram CS. The usefulness of the International Diabetes Federation and the National Cholesterol Education Program's Adult Treatment Panel III definitions of the metabolic syndrome in predicting coronary heart disease in subjects with type 2 diabetes. Diabetes Care. 2007. 30:1206–1211.
31. Kim TH, Kim DJ, Lim S, Jeong IK, Son HS, Chung CH, Koh G, Lee DH, Won KC, Park JH, Park TS, Ahn J, Kim J, Park KG, Ko SH, Ahn YB, Lee I. Prevalence of the metabolic syndrome in type 2 diabetic patients. Korean Diabetes J. 2009. 33:40–47.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download