INTRODUCTION
The incidence of thyroid cancer has dramatically increased in the past 2 decades, owing to the explosive increase of papillary thyroid microcarcinoma (
1). Differentiated thyroid cancer has an excellent prognosis and the overall survival rate exceeds 90% to 95%, according to a surveillance, epidemiology, and end results (SEER) report (
2). The traditional risk factors for differentiated thyroid cancer include clinicopathological variables, such as age at diagnosis, tumor size, extrathyroidal extension (ETE), and distant metastasis (
3).
The American Joint Committee on Cancer (AJCC)/tumor, node, and metastasis (TNM) staging system is the most clinically useful and provides the highest proportion of variance explained (PVE) in survival analysis (a statistical measure of how well a staging system can predict the outcome of interest) (
4). The AJCC and Union for International Cancer Control (UICC) cyclically modify the TNM system to improve prognosis prediction and update risk factors according to newly acquired clinical data (
5). In 2016, the AJCC 8th edition for thyroid cancer was released and included major revision on TNM staging, resulting in significant stage migration. The aim of our study was to describe this stage migration of the 7th and 8th editions of the AJCC/TNM staging system using a cohort of differentiated thyroid cancer patients from a single institution.
METHODS
We reviewed 2,447 patients who underwent thyroidectomy between September 2008 and December 2011 at Seoul St. Mary's Hospital of The Catholic University of Korea. Of these, the complete medical records of 2,234 patients with differentiated thyroid cancer were retrospectively analyzed.
The extent of thyroid gland resection was determined in accord with the guidelines issued by the American Thyroid Association (ATA) guideline (
67). Patients with multiple lesions, bilateral lesions, thyroid capsular invasion during surgery, a history of head or neck radiotherapy, or a first-degree familial history of thyroid cancer, underwent total thyroidectomy (
67). Therapeutic central-compartment neck dissection was performed in patients with suspicious central node metastasis (
67). Prophylactic ipsilateral central-compartment neck dissection was performed in patients who were diagnosed with well-differentiated papillary thyroid carcinoma preoperatively. In patients with a metastatic lymph node in the lateral neck, selective lymph node dissection including level II, III, IV, V lymph node was performed (
67). All patients were administered levothyroxine for thyroid stimulating hormone suppression postoperatively. Radioactive iodine therapy was performed 6 to 8 weeks after total thyroidectomy, based on stage and risk factors, according to the ATA guidelines (
67). Serum thyroglobulin levels and neck ultrasonography were regularly checked during follow-up.
The TNM classification was established according to the 7th and 8th editions of the AJCC/UICC staging system. For reclassification, the histologic report and surgery report were reviewed (
89). ETE was reclassified as none, minimal thyroid capsule invasion, gross strap muscle invasion, subcutaneous soft tissue/trachea/nerve/esophagus/larynx invasion, or prevertebral fascia/major vessel invasion (
9). Minor extension through the thyroid capsule, which was only observed on histologic examination without grossly evident strap muscle invasion was defined as minimal thyroid capsule invasion. Clinical nodal status on preoperative imaging and clinical examination was reflected in the reclassification according to the 8th edition of the AJCC/UICC staging system (
Table 1) (
9).
Table 1
The 8th edition of AJCC/UICC staging system of differentiated thyroid cancer
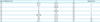
|
Age at diagnosis (yr) |
T |
N |
M |
Stage group |
|
<55 |
Any T |
Any N |
M0 |
I |
|
<55 |
Any T |
Any N |
M1 |
II |
|
≥55 |
T1 |
N0/NX |
M0 |
I |
|
≥55 |
T1 |
N1 |
M0 |
II |
|
≥55 |
T2 |
N0/NX |
M0 |
I |
|
≥55 |
T2 |
N1 |
M0 |
II |
|
≥55 |
T3a/T3b |
Any N |
M0 |
II |
|
≥55 |
T4a |
Any N |
M0 |
III |
|
≥55 |
T4b |
Any N |
M0 |
IVA |
|
≥55 |
Any T |
Any N |
M1 |
IVB |
Follow-up data was obtained from patient records. Vital status was followed through September 2008 to March 2017. Mortality data were also acquired from patient medical records from September 2008 to March 2017, as well as from the Korea Central Cancer Registry database and cancer mortality database from the Korea National Statistical Office until December 2014. Cause of death was based on death certificate reports. Recurrence was defined as structural evidence of disease which was confirmed by fine-needle aspiration cytology and/or functional or radiological evidence of distant metastasis (
10).
All statistical analyses were performed using the SPSS ver. 15.0 software package (SPSS Inc., Chicago, IL, USA). P values of <0.05 were considered statistically significant.
RESULTS
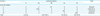
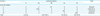
The clinical characteristics of a total of 2,234 cases are detailed in
Table 2. Mean patient age was 46.5 years (range, 11–81) and the male to female ratio was 1:4.6. We found that papillary cancer was the most common cancer type (98.1%), while follicular and Hurthle cell cancer/poorly differentiated cancer was found in 1.8% and 0.1% of the patients, respectively. Mean tumor size was 0.95 cm (range, 0.1–9.0 cm). In terms of surgical extent, total thyroidectomy was performed more frequently (81.9%), while radioactive iodine therapy was performed in 1,447 (79.1%) of 1,829 total thyroidectomy cases.
Table 2
Clinicopathologic characteristics of thyroid cancer cohort

|
Characteristic |
Thyroid cancer cohort (n=2,234) |
|
Age (yr) |
46.5±12.0 (11–81) |
|
Gender ratio (M:F) |
402:1,832 (1:4.6) |
|
Type of cancer |
|
|
Papillary |
2,192 (98.1) |
|
Follicular and Hurthle cell |
41 (1.8) |
|
Poorly differentiated |
1 (0.1) |
|
Mean tumor size (cm) |
0.95±0.74 (0.1–9.0) |
|
Extent of thyroidectomy |
|
|
Total thyroidectomy |
1,829 (81.9) |
|
Less than thyroidectomy |
405 (18.1) |
|
Radioactive iodine therapy*
|
|
|
No |
382 (20.9) |
|
Yes |
1,447 (79.1) |
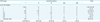
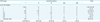
The key clinicopathological characteristics for re-categorization according to the 8th edition of the AJCC/UICC staging system are described in
Table 3. Of the 2,234 cases, 673 (30.1%) patients were between 45 and 55 years of age. We found that a tumor size under 2 cm occurred in 2,092 (93.6%) patients, 2 to 4 cm in 124 (5.6%) patients, and over 4 cm in 18 (0.8%) patients. When we analyzed ETE, we found that a total of 1,135 cases (50.8%) were intrathyroid lesions, 838 cases (37.6%) showed minimal histologic thyroid capsule invasion, 191 cases (8.5%) had gross strap muscle invasion, and 70 cases (3.1%) had trachea, nerve, esophagus, and larynx invasion.
Table 3
Key clinicopathologic characteristics for categorization in the AJCC/UICC classification in differentiated thyroid cancer

|
Characteristic |
Thyroid cancer cohort (n=2,234) |
|
Age (yr) |
|
|
<45 |
990 (44.3) |
|
45≤age<55 |
673 (30.1) |
|
≥55 |
571 (25.6) |
|
Tumor size (cm) |
|
|
≤2 |
2,092 (93.6) |
|
2<size≤4 |
124 (5.6) |
|
>4 |
18 (0.8) |
|
ETE |
|
|
No |
1,135 (50.8) |
|
Minimal |
838 (37.6) |
|
Strap muscle |
191 (8.5) |
|
Subcutaneous soft tissue, trachea, nerve, esophagus, larynx |
70 (3.1) |
|
Node metastasis |
|
|
Unknown |
191 (8.5) |
|
No |
1,106 (49.5) |
|
Central node metastasis |
735 (32.9) |
|
Lateral node metastasis |
202 (9.0) |
|
Distant metastasis |
|
|
No |
2,230 (99.9) |
|
Yes |
4 (0.1) |
When we examined nodal status, we found that 1,106 patients (49.5%) lacked nodal metastasis, 735 (32.9%) had central node metastasis, and 202 (9%) had lateral neck node metastasis. The nodal states of 191 patients (8.5%) were unknown due to omission of nodal dissection in follicular neoplasm and/or no node in histologic examination after nodal dissection. Four patients (0.1%) showed distant metastasis at diagnosis.
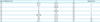
The stage migration that occurred following reclassification according to recommendations from the 7th to 8th editions of the AJCC/UICC staging system is described in
Tables 4,
5,
6. Using the 7th edition, we found 1,101 (49.3%) T1 patients, 30 (1.3%) T2 patients, 1,033 (46.2%) T3 patients, and 69 (3.1%) and 1 (0.9%) T4a and T4b patients, respectively. After reclassification according to the 8th edition, T3 patients were reassigned to different stages. Seven hundred and ninety-eight and 33 T3 patients were downgraded to T1 and T2, respectively. Seven patients were reassigned to T3a and 191 patients were reassigned to T3b. As a result, the numbers of T1 and T2 cases increased to 1,899 (85%) and 67 (3.0%), respectively (
Table 4).
Table 4
Comparison of the 7th and 8th editions of AJCC staging for T status in thyroid cancer cohort

|
T status |
AJCC 8th edition |
Total |
|
1 |
2 |
3a |
3b |
4a |
4b |
|
AJCC 7th edition |
|
|
|
|
|
|
|
|
1 |
1,101 |
0 |
0 |
0 |
0 |
0 |
1,101 (49.3) |
|
2 |
0 |
30 |
0 |
0 |
0 |
0 |
30 (1.3) |
|
3 |
798 |
37 |
7 |
191 |
0 |
0 |
1,033 (46.2) |
|
4a |
0 |
0 |
0 |
0 |
69 |
0 |
69 (3.1) |
|
4b |
0 |
0 |
0 |
0 |
0 |
1 |
1 (0.0) |
|
Total |
1,899 (85.0) |
67 (3.0) |
7 (0.3) |
191 (8.5) |
69 (3.1) |
1 (0.0) |
|
Table 5
Comparison of the 7th and 8th editions of AJCC staging for N status in thyroid cancer cohort
|
N status |
AJCC 8th edition |
Total |
|
X |
0a |
0b |
1a |
1b |
|
AJCC 7th edition |
|
|
|
|
|
|
|
X |
0 |
0 |
191 |
0 |
0 |
191 (8.6) |
|
0 |
0 |
1,106 |
0 |
0 |
0 |
1,106 (49.5) |
|
1a |
0 |
0 |
0 |
735 |
0 |
735 (32.9) |
|
1b |
0 |
0 |
0 |
0 |
202 |
202 (9.0) |
|
Total |
0 (0.0) |
1,297 (58.1) |
735 (32.9) |
202 (9.0) |
|
Table 6
Comparison of the 7th and 8th editions of AJCC staging for TNM stage in thyroid cancer cohort
|
TNM stage |
AJCC 8th edition |
Total |
|
I |
II |
III |
IVA |
IVB |
|
AJCC 7th edition |
|
|
|
|
|
|
|
I |
1,354 |
0 |
0 |
0 |
0 |
1,354 (60.6) |
|
II |
3 |
2 |
0 |
0 |
0 |
5 (0.2) |
|
III |
452 |
179 |
0 |
0 |
0 |
631 (28.2) |
|
IVA |
66 |
33 |
20 |
0 |
0 |
119 (5.3) |
|
IVB |
0 |
0 |
0 |
1 |
0 |
1 (0.0) |
|
IVC |
0 |
1 |
0 |
0 |
1 |
2 (0.1) |
|
Unknown (Nx) |
119 |
3 |
0 |
0 |
0 |
122 (5.5) |
|
Total |
1,994 (89.3) |
218 (9.8) |
20 (0.9) |
1 (0.0) |
1 (0.0) |
|
For nodal stage classifications, we found that 191 cases (8.6%) of unknown nodal stage according to the 7th edition were reclassified as N0b; therefore, N0 cases increased from 1,106 (49.5%) to 1,297 (58.1%) (
Table 5). The TNM staging showed notable changes owing to changes in the age cutoff point, definition of ETE, and changes from NX to N0b. As a result, we reclassified 640 patients into stage I. Three stage II patients became stage I, and 2 patients remained in stage II. Stage III and IVA patients were decreased notably upon reclassification: 452 stage III patients were reassigned to stage I and the remaining 179 patients were reassigned to stage II. All stage IVA patients were reclassified into stages I (66 cases), II (33 cases), or III (20 cases). One stage IVB patient was downgraded to stage IVA and 2 stage IVC patients were downgraded to stage II (1 case) or stage IVB (1 case). Of the 122 unknown stage tumors according to the 7th edition, 119 were reassigned to stage I and 3 were assigned to stage II. As a result, stage I and II cases increased remarkably from 1,354 (60.6%) to 1,994 (89.3%), and from 4 (0.2%) to 218 (9.8%), respectively. Concordantly, there was a corresponding decrease in stage III and IVA patients from 631 (28.3%) to 20 (0.9%), and from 119 (5.3%) to 1 (0.0%), respectively (
Table 6).
Mean follow-up time was 70.8±19.1 months (range, 1–103 months). Among the 10 deaths during follow-up, only 1 case was a thyroid cancer-related death. Sixty-eight patients showed recurrent disease during follow-up and the mean disease-free time was 22.0 months (range, 4–78 months). Central neck recurrence, lateral neck recurrence, and contralateral lobe recurrence occurred in 19, 44, and 2 patients, respectively. Four patients had distant metastasis to the lung and 1 had both lung and bone metastasis during follow-up (
Table 7). Disease-free survival (DFS) was calculated using the Kaplan-Meier method and was compared using the log-rank test (
Fig. 1). According to the 7th edition, TNM stage significantly predicted recurrence-free survival (P<0.001,
Fig. 1A). In the subgroup analysis, stage I had better DFS than stages II and IVA (P=0.016 and P<0.001, respectively), and stage III had better DFS than stage IVA (P<0.001, data not shown). However, stage II showed an inverse relationship with stage III and cases of unknown stage, and had significantly worse DFS than stage III and unknown stage (P=0.002 and P<0.001, respectively, data not shown). The new TNM stages after reclassification according to the 8th edition failed to show a statistical difference in recurrence-free survival (P=0.462,
Fig. 1B).
Table 7
Sixty-eight recurrence disease during follow-up

|
Recurrence case |
Recurrence (n=68) |
|
Central neck recurrence |
19 |
|
Lateral neck recurrence |
44 |
|
Contralateral lobe recurrence |
2 |
|
Distant metastasis |
5*
|
Fig. 1
Cumulative recurrence curves according to the 7th (A) and 8th (B) editions of the AJCC/UICC staging system.
AJCC = American Joint Committee on Cancer; UICC = Union for International Cancer Control.

DISCUSSION
The AJCC/UICC TNM staging is the most widely used cancer staging system due to its accurate predictive power for prognosis and survival analysis (
89). The AJCC/UICC system undergoes revisions periodically to accommodate advances in cancer care and improve the prediction of cancer behavior and prognosis (
89). To decide on these changes, the AJCC/UICC has an expert panel that restructures, validates, and revises the staging system based on the clinical data (
89).
The major changes between the 7th and 8th editions include changes in age cutoff point at diagnosis, definition of ETE and N0, and changes in the stage categories according to new T, N, and M categories (
89).
Age at diagnosis is powerful independent predictor of prognosis and mortality in thyroid cancer (
311), and the mortality of thyroid cancer increases progressively with advancing age (
1213). Most staging systems, including Age, Grade, Extent, Size (AGES), Metastases, Age at presentation, Completeness of Resection, Invasion, Size (MACIS), Age, Metastases, Extent, Size (AMES), European Organization for Research and Treatment of Cancer (EORTC), and Memorial Sloan-Kettering Cancer Center (MSKCC), use age cutoffs between 40 and 50 years (
3). The AJCC recommends an age cutoff point of 45 years in the 2nd edition through the 7th edition. However, multiple studies have recommended moving the age cutoff from 45 to 55 years, or using multiple age categories to better reflect the relationship between age and prognosis (
141516). In the 8th edition of AJCC/UICC staging guidelines, the age cutoff point was moved from 45 to 55 years. Therefore, we found that most patients between 45 and 55 years of age without distant metastasis at diagnosis were re-categorized to stage I. Nixon et al. (
11) reported that the application of the new age cutoff of 55 years resulted in downstaging of 12% of differentiated thyroid cancer patients and prevented low-risk patients from being overstaged and overtreated. In this study, a total of 410 (18.4%) patients were downstaged according to the new age cutoff guidelines. The incidence of thyroid cancer in Korea showed a peak of age between 50 and 55 years; therefore, a significant number of patients will be reassigned to an earlier stage when the 8th edition is implemented in January 2018 (
17).
The primary tumor category was determined based on tumor size and degree of ETE (
89). We found that the size category of the primary tumor was same in both 7th and 8th editions; however, in terms of ETE, the phrase “minimal ETE to the sternothyroid muscle or perithyroidal soft tissue” in the T3 category was changed to “gross ETE invading only strap muscles” (
9). Minor extension through the thyroid capsule, which was only observed on histologic examination, is not clinically appreciated in the 8th edition because it lacks a prognostic significance recommendation for persistent/recurrent disease and disease-specific and recurrence-free survival (
9181920). Grossly evident ETE included not only strap muscle invasion seen upon histologic examination, but also invasion identified by imaging or intraoperative findings (
9). In this study, a total of 835 (37.4%) T3 patients with minor ETE were downstaged to T1/T2 according to tumor size, and only 191 patients who showed gross ETE were reassigned to stage T3b upon application of the 8th edition guideline. The presence of ETE showed positive correlation with tumor size (
18). The incidence of small size thyroid cancer has increased in worldwide, therefore, the proportion of T1/T2 cancer might increase according to the new ETE definition (
21).
According to the 2015 ATA management guidelines for adult patients with differentiated thyroid cancer, prophylactic central-compartment neck dissection was not recommended in clinically node-negative small T1/T2 papillary thyroid cancer and most follicular cancer cases (
10). The cases for which regional lymph nodes could not be assessed by histologic examination for nodal stage classification were categorized as NX according to the 7th edition (
8). However, according to the 8th edition, patients who did not show radiologic or clinically evident of nodal metastasis were categorized as N0b, even though they lacked nodal dissection (
9). Metastasis to the superior mediastinal node (level VII) was categorized as N1b according to the 7th edition; however, it was reclassified as N1a according to the 8th edition (
9).
For patients over 55 years of age, the TNM staging according to the 8th edition of the AJCC/UICC system demonstrated that N1a and N1b had an equal impact on TNM stage (
9). Furthermore, nodal stage had little impact on TNM stage upgrading, especially for T3/T4 tumors according to the 8th edition. However, nodal stage had a powerful effect on TNM stage for T1–T3 tumors according to the 7th edition (
89). In T3/T4 patients over 55 years of age, tumor stage had a greater effect on TNM stage than nodal stage. This change may be due to the fact that it was not clear whether the anatomic location of the metastatic node correlated with survival (
9). According to the ATA guidelines, the size and number of metastatic nodes were emphasized in the modified initial risk stratification system (
10).
Nixon et al. (
11) reported that the 10-year disease-specific survival rates were 96% and 81% in stage III and IV patients according to the 7th edition of the AJCC/UICC staging system, respectively. This report revealed that many advanced stage patients were overstaged using the current staging system and this overstaging caused clinicians to choose more aggressive treatments without definite benefits (
11). To improve the prognosis prediction, downstaging was the most distinct characteristic that occurred upon reclassification using the 8th edition (
9). For example, in the 8th edition, stage II was expanded from T2 N0 to T1/T2 N1 tumors and T3 any N tumors in patients over 55 years of age (
9). Additionally, stage III was downscaled from T3 N0 and T1–T3 N1a to T4a any N. Finally, stage IVA was reduced from T1–T3 N1b and T4a any N to T4b any N. Therefore, a total of 758 patients (33.9%) were downstaged in this study.
This study had a limitation that failed to compare the prognostic predictability of the 7th and 8th editions of the AJCC/UICC staging system due to the small number of observed death and recurrent events. Therefore, a larger, multi-institutional, international study is needed to validate the 8th edition of the AJCC/UICC staging system.
In conclusion, application of the guidelines in the 8th edition of the AJCC/UICC staging system for differentiated thyroid cancer resulted in marked TNM staging migration in the direction of downstaging.







 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download