Abstract
Purpose
To assess the antibiotic susceptibility of Escherichia coli from community-acquired uncomplicated urinary tract infection (UTI).
Materials and Methods
Between August and December of 2015, confirmed cases of E. coli as a pathogen of community-acquired uncomplicated UTI were collected and assessed for antibiotic susceptibility in 10 designated hospitals. Additional fosfomycin susceptibility test was performed by a central laboratory using the disk diffusion method.
Results
A total of 347 E. coli isolates were collected from urine samples of community-acquired uncomplicated UTIs patients. The susceptibility rates of antibiotics were as follows: amikacin 100.0% (347), imipenem 100.0% (347), ciprofloxacin 57.1% (198), cefotaxime 74.9% (260), ampicillin 30.0% (104), trimethoprim/sulfamethoxazole 66.9% (232), and fosfomycin 98.0% (340). All fosfomycin-resistant E. coli isolates were extended-spectrum β-lactamase (ESBL)-producing. In 85 cases of ESBL-producing E. coli, the fosfomycin susceptibility rate was 91.8% (78/85).
Urinary tract infection (UTI) is a common disease among diverse age groups. Many clinicians are confronted with UTIs even in primary healthcare practices, as well as in tertiary medical centers. Its high prevalence rate and morbidity make frequent use of antimicrobials clinically [1]. Antibiotic resistance has been increasing recently, and its seriousness is a global problem. Empirical antimicrobials for the treatment of UTIs should be selected on the basis of epidemiological data, including the characteristics of causative bacteria and the result of susceptibility test in a regional community. Resistant bacteria are constantly evolving, and as such, continuous monitoring of the resistance pattern of uropathogens is important for the establishment of empirical therapy. Fosfomycin has been a recently re-emerging antibiotic, representing the epoxide class of antibiotics. It has been focused in treating infectious diseases from multidrug-resistant Enterobacteriaceae. In this study, the susceptibility pattern of antimicrobials to Escherichia coli from community-acquired uncomplicated UTIs was assessed focusing on fosfomycin.
To reflect the national status of antimicrobial susceptibility, a nationwide hospital recruitment was accomplished. For the responsible fulfillment of laboratory processes, institutions were selected preferentially among university hospitals that cooperated with the Korean Association of Urogenital Tract Infection and Inflammation (KAUTII). A total of 10 university hospitals covering a vast majority of the country were recruited. Between August and December of 2015, study materials were collected from these hospitals.
The materials of this study were E. coli identified in the usual outpatient clinical process. Mid-stream urine samples from adult female patients, who were diagnosed with community-acquired uncomplicated UTIs in the outpatient clinic, were collected for culture identification before taking any antimicrobials. If E. coli was confirmed as a pathogen, the strain was enrolled in this study. Any complicated UTI cases, including urolithiasis, male patients, indwelling catheter, uncontrolled diabetes mellitus, kidney transplantation, and urogenital anomaly, were excluded. The Institutional Review Board of St. Vincent's Hospital of The Catholic University of Korea approved the study protocol (VC15OIMI0059).
Consistent study guidelines for urine collection, culture, antibiotic susceptibility test, and delivery of bacterial colony were established all institutions that participated. Mid-stream urine of 10 ml was collected in sterile container and was streaked onto the blood and MacConkey agar. After culture at 37℃, all E. coli were characterized on the Vitek® 2 using GN and AST-GN30 cards (BioMérieux, Durham, NC, USA) for routine identification and susceptibility testing.
Presently, fosfomycin susceptibility test was not applicable to the automated system of each designated hospital. For an additional test, the E. coli plates were sealed with plastic film and delivered to the central lab in a cold storage system (Departments of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea) within 24 hours. The disk diffusion method was used for the susceptibility test of fosfomycin [2]. From the delivered E. coli plate, 1 colony was collected and put into the Muller-Hinton broth. Turbid was adjusted with MacFarland unit 0.5, and the liquid was evenly streaked 3 times with a cotton bud onto the Muller-Hinton agar. Before being dried out, fosfomycin disk was put down on the plate and was cultured overnight at 37℃. The zone diameter interpretation was as follows: Resistant: 12 mm or less, Intermediate: 13-15 mm, and Susceptible: 16 mm or more.
A total of 347 E. coli isolates were collected from the urine cultures. All enrolled patients had community-acquired uncomplicated UTIs that were composed of acute cystitis (84.1%, 292) and acute pyelonephritis (15.9%, 55). All patients were female, and the average age was 46.9 (21-72 years old). The most prevalent comorbidity was diabetes (3.5%, 12). The proportion of patients who had undergone antibiotic treatment for UTI in the past 6 months was 35.7% (124).
The susceptibility rates of antibiotics were as follows: amikacin 100.0% (347), imipenem 100.0% (347), ciprofloxacin 57.1% (198), cefotaxime 74.9% (260), ampicillin 30.0% (104), trimethoprim/sulfamethoxazole (TMP/SMX) 66.9% (232), and fosfomycin 98.0% (340). The rate of extended-spectrum β-lactamase (ESBL) manifestation was 24.5% (85). Table 1 shows the number of isolates and susceptibility.
Fosfomycin susceptibility was higher than most other antibiotics. Only 7 out of the 347 E. coli isolates were resistant to fosfomycin. All of the fosfomycin-resistant E. coli were ESBL-producing. In 85 cases of ESBL-producing E. coli, the fosfomycin susceptibility rate was 91.8% (78/85). Even in these cases, amikacin and imipenem still showed to be effective. Among patients who provided fosfomycin-resistant strains, 85.7% (6/7) cases had one or more experiences of UTI in the past 6 months.
For the establishment of valid guidelines for UTIs, microbiological characteristics, including clinical information about hospital and community acquired infection, should be provided. Particularly for primary health clinic, the guidelines should reflect the data on the community acquired UTI. According to a previous research regarding unresolved acute uncomplicated cystitis, the patient who failed to be treated of UTI at a primary clinic showed high antibiotics resistance rate in the empirical regimen. If the first line antimicrobial, like TMP/SMX or fluoroquinolone seems to be ineffective, a second line antimicrobial should be considered on the basis of local resistance study [3]. Improved surveillance of antibiotic resistance among uropathogens that causes uncomplicated UTIs may help clinicians to make informed decisions about the empirical and alternative treatment of uncomplicated UTIs [4].
Antibiotic resistance has been steadily increasing, and existing empirical treatments of uncomplicated UTI is becoming a problem. The treatment of emerging multidrug resistant (MDR) gram-negative organisms is also becoming a greater challenge. The slow rate of development of newer antimicrobials has led to the re-discovery of the ‘old’ and ‘forgotten’ antibiotics, like colistin and fosfomycin [56]. Fosfomycin was first isolated in 1969 from Streptomyces, which is now produced synthetically [6]. Fosfomycin inhibits the synthesis of peptidoglycan at a step earlier than beta-lactam or glycopeptide antibiotics and has a broad spectrum of activities against various Gram-positive and Gram-negative bacteria, including methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci. In the early period of its development, in vitro test of the drug was not able to support in vivo results, and it had been underutilized. Recently, however, fosfomycin received attention as an agent against MDR and has been actively researched [789]. It has been shown to have advantages in treating UTIs due to its high concentration in the urinary tract, exceeding 2,000 mg/L after the initial administration that remains for a prolonged period, over 24 hours [810]. Moreover, fosfomycin has been shown to be very well tolerated and with a low adverse effects, ranging between 1-10% of patients [8].
The clinical evidence of fosfomycin against resistant Gram-negative infections is limited but promising. There have been several clinical studies in Spain, France, and Italy since 1990 [11]. The susceptibility rate of fosfomycin in these countries was revealed to be around 97.4-99.4% [12131415]. Japan has been using fosfomycin for systemic infection, showing high efficacy against several infections; it has remained to be favorable against several bacterial species for more than 20 years [1116].
Recently, there have been several studies in South Korea on fosfomycin with respect to UTI treatment. Seo et al. [17] reported in 2014 reported that fosfomycin susceptibility on community-acquired UTI was 100% (346/346). With respect of ESBL control, Cho et al. [18] tested 277 isolates of ESBL-positive E. coli and Klebsiella pneumoniae from urine samples of patients with UTI, and showed that 243 out of the 277 (87.7%) isolates were susceptible to fosfomycin. In another study, a total of 347 non-duplicate ESBL-producing E. coli (165 isolates) and K. pneumoniae (182 isolates) were collected, and the susceptibility to fosfomycin was reported to be 92.9% in E. coli and 95.2% in K. pneumoniae (Table 2) [19].
This study has some limitations. Only tertiary referral hospitals participated in this study. Therefore, theoretically, our results may be inappropriate for full extrapolation to other patient population receiving care in non-tertiary facilities. As a referral hospital, it is possible that some of the enrolled patients with uncomplicated UTIs may have been referred from primary clinics after failed initial antimicrobial treatment. In such patients, the antimicrobial susceptibility was expected to be lower compared with those presenting UTIs without prior exposure to antimicrobial treatment [3].
Many reports including this study suggest the value of fosfomycin as a useful option for the treatment of community acquired uncomplicated UTIs. To establish the guideline for UTI management, the role of fosfomycin should be reviewed. Further research is necessary to verify the clinical efficacy of fosfomycin as a means to treat UTIs.
Figures and Tables
Table 1
Antibiotic susceptibility patterns of Escherichia coli from patients with community-acquired uncomplicated urinary tract infection (n=347)
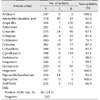
Table 2
Representative list of the studies on fosfomycin susceptibility with Escherichia coli
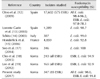
| Reference | Country | Isolates studied | Fosfomycin susceptibility (%) |
|---|---|---|---|
| Oteo et al. [12] (2009) | Spain | 17,602 (575 ESBL) | All E. coli: 98.4-96.2, ESBL E. coli: 97.8-78.3 |
| Lorente Garin et al. [13] (2005) | Spain | 1,289 | E. coli: 98.7 |
| Schito [14] (2003) | Italy | 387 | E. coli: 99.0 |
| Honderlick et al. [15] (2006) | France | 4,859 | E. coli: 92.8 |
| Seo et al. [17] (2014) | Korea | 346 | E. coli: 100 |
| Cho et al. [18] (2015) | Korea | 243 (all ESBL) | ESBL E. coli: 94.9 |
| Lee et al. [19] (2012) | Korea | 165 (all ESBL) | ESBL E. coli: 92.9 |
| Present study (2017) | Korea | 347 (85 ESBL) | All E. coli: 98.0, ESBL E. coli: 91.8 |
ACKNOWLEDGMENTS
This study is supported by the Korean Association of Urogenital Tract Infection and Inflammation (KAUTII). The authors appreciate the colleagues for the dedication in collecting the clinical isolates of bacteria.
References
1. Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med. 2012; 366:1028–1037.
2. Jorgensen JH, Ferraro MJ. Antimicrobial susceptibility testing: a review of general principles and contemporary practices. Clin Infect Dis. 2009; 49:1749–1755.

3. Kim HY, Lee SJ, Lee DS, Yoo JM, Choe HS. Microbiological characteristics of unresolved acute uncomplicated cystitis. Microb Drug Resist. 2016; 22:387–391.

4. Miller LG, Tang AW. Treatment of uncomplicated urinary tract infections in an era of increasing antimicrobial resistance. Mayo Clin Proc. 2004; 79:1048–1053. quiz 1053-4.

5. Dhariwal AK, Tullu MS. Colistin: re-emergence of the ‘forgotten’ antimicrobial agent. J Postgrad Med. 2013; 59:208–215.

6. Popovic M, Steinort D, Pillai S, Joukhadar C. Fosfomycin: an old, new friend? Eur J Clin Microbiol Infect Dis. 2010; 29:127–142.

7. Saiprasad PV, Krishnaprasad K. Exploring the hidden potential of fosfomycin for the fight against severe Gram-negative infections. Indian J Med Microbiol. 2016; 34:416–420.

9. Thaden JT, Pogue JM, Kaye KS. Role of newer and re-emerging older agents in the treatment of infections caused by carbapenem-resistant Enterobacteriaceae. Virulence. 2017; 8:403–416.

10. Naber KG, Thyroff-Friesinger U. Fosfomycin trometamol versus ofloxacin/co-trimoxazole as single dose therapy of acute uncomplicated urinary tract infection in females: a multicentre study. Infection. 1990; 18:Suppl 2. S70–S76.

11. Karageorgopoulos DE, Wang R, Yu XH, Falagas ME. Fosfomycin: evaluation of the published evidence on the emergence of antimicrobial resistance in Gram-negative pathogens. J Antimicrob Chemother. 2012; 67:255–268.

12. Oteo J, Orden B, Bautista V, Cuevas O, Arroyo M, Martinez-Ruiz R, et al. CTX-M-15-producing urinary Escherichia coli O25b-ST131-phylogroup B2 has acquired resistance to fosfomycin. J Antimicrob Chemother. 2009; 64:712–717.

13. Lorente Garin JA, Placer Santos J, Salvado Costa M, Segura Alvarez C, Gelabert-Mas A. Antibiotic resistance transformation in community-acquired urinary infections. Rev Clin Esp. 2005; 205:259–264.
14. Schito GC. Why fosfomycin trometamol as first line therapy for uncomplicated UTI? Int J Antimicrob Agents. 2003; 22:Suppl 2. 79–83.

15. Honderlick P, Cahen P, Gravisse J, Vignon D. Uncomplicated urinary tract infections, what about fosfomycin and nitrofurantoin in 2006? Pathol Biol (Paris). 2006; 54:462–466.
16. Hara T, Araake M, Watabe H. Antibacterial activities of fosfomycin against several fresh clinical isolates--comparison of the test methods for antibacterial activity. Jpn J Antibiot. 2002; 55:844–854.
17. Seo MR, Kim SJ, Kim Y, Kim J, Choi TY, Kang JO, et al. Susceptibility of Escherichia coli from community-acquired urinary tract infection to fosfomycin, nitrofurantoin, and temocillin in Korea. J Korean Med Sci. 2014; 29:1178–1181.

18. Cho YH, Jung SI, Chung HS, Yu HS, Hwang EC, Kim SO, et al. Antimicrobial susceptibilities of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in health care-associated urinary tract infection: focus on susceptibility to fosfomycin. Int Urol Nephrol. 2015; 47:1059–1066.

19. Lee SY, Park YJ, Yu JK, Jung S, Kim Y, Jeong SH, et al. Prevalence of acquired fosfomycin resistance among extended-spectrum β-lactamase-producing Escherichia coli and Klebsiella pneumoniae clinical isolates in Korea and IS26-composite transposon surrounding fosA3. J Antimicrob Chemother. 2012; 67:2843–2847.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download