Abstract
Lymphocele infection is a rare complication after radical prostatectomy and pelvic lymph node dissection (PLND). Here, we present a case of lymphocele infection that extended to the leg two months after robot-assisted laparoscopic radical prostatectomy and PLND. The patient was a 60-year-old man whose chief complaints were fever, chills, and right thigh pain. Computed tomography showed infected lymphocele with right thigh abscess. After percutaneous drainage and intravenous antibiotics, the infection and right thigh abscess were resolved.
A lymphocele is a collection of lymphatic fluid within the body that is not bordered by epithelial lining; this occurs as a consequence of surgical dissection of afferent lymphatic vessels. After radical prostatectomy and pelvic lymph node dissection (PLND), incidence of symptomatic lymphocele is rare; however, asymptomatic lymphocele occurs in up to 61% of cases [1]. Symptomatic lymphoceles present infection, deep vein thrombosis (DVT), pulmonary embolism, and/or leg edema, with infection being the most common concurrent presentation [2].
Here, we present a case of infected lymphocele that extended to the leg after robot-assisted radical prostatectomy (RARP) and PLND.
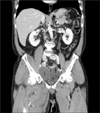
A 60-year-old man referred to our hospital presented fever, chills, myalgia, and right thigh pain. He underwent RARP and PLND at a different hospital two months prior to his referral. He experienced myalgia and right thigh pain for four days and took amoxicillin for two days. However, fever and right thigh pain persisted, causing him to visit our emergency department. His blood pressure was 130/80 mmHg, body temperature was 37.5℃, pulse rate was 110 beats/minute, and respiratory rate was 26 breaths/minute. Physical examination revealed right thigh swelling, heating sense, and tenderness. On laboratory examination, his white blood cell count was 19,700×103/µl (neutrophils, 89%), erythrocyte sedimentation rate was 69 mg/h, and C-reactive protein level was 217.4 mg/L. Urine analysis was unremarkable. Abdominopelvic computed tomography (CT) scan showed a cystic mass measuring 8.5×5.4 cm with a thick capsule in the right pelvic cavity, and another cystic mass measuring 8.3×4.6 cm with heterogeneous enhancement in the right thigh (Fig. 1). He underwent percutaneous drainage of the right infected lymphocele and was administered with intravenous antibiotics. Right thigh abscess decreased in size after percutaneous drainage (Fig. 2); pus culture revealed Staphylococcus aureus. Ten days after puncture, the lymphocele cavity had decreased in size and the pigtail catheter was removed.
In intermediate and high-risk prostate cancer, PLND is a prerequisite to determining accurate staging, predicting prognosis, and deciding on therapeutic treatment [34].
Lymphoceles occur due to a leakage from transected lymphatic vessels and remains to be the most common complication after PLND. The incidence of lymphocele formation is higher in extended PLND than in limited PLND [56]. Lymphoceles are mostly asymptomatic in up to 61% of cases [1] and most either resolve spontaneously or exist without causing any problems. Symptomatic lymphoceles are rare after PLND and present with infection, DVT, pulmonary embolism, and/or leg edema, among which, infection is the most common presentation [2].
In the present case, infection disseminated to the leg, likely as a result of efferent vessels from the deep inguinal lymph nodes passing through the femoral canal, entering the external iliac lymph nodes.
Treatment of infected lymphocele generally includes percutaneous drainage and/or sclerotherapy, open evacuation, or laparoscopic marsupialization [7].
S. aureus infection was found in this case. Hamada et al. [8] reported that gastrointestinal tract and skin flora are the main infectious agents in infected lymphoceles, following PLND for prostate cancer. Thus, they suggest a combination of intravenous ampicillin/sulbactam and vancomycin as the best initial empiric therapy for infected lymphocele.
To the best of my knowledge, this is the first report of infected lymphocele extending to the leg.
Based on this experience, it is recommended that for patients presenting leg pain paired with fever, chills, or any other related symptoms after radical prostatectomy and PLND, infected lymphocele should be considered. This should be confirmed via imaging studies (CT or sonography), and antibiotic treatment and/or percutaneous drainage should be followed.
Figures and Tables
References
1. Solberg A, Angelsen A, Bergan U, Haugen OA, Viset T, Klepp O. Frequency of lymphoceles after open and laparoscopic pelvic lymph node dissection in patients with prostate cancer. Scand J Urol Nephrol. 2003; 37:218–221.

2. Ploussard G, Briganti A, de la Taille A, Haese A, Heidenreich A, Menon M, et al. Pelvic lymph node dissection during robotassisted radical prostatectomy: efficacy, limitations, and complications-a systematic review of the literature. Eur Urol. 2014; 65:7–16.

3. Aus G, Abbou CC, Bolla M, Heidenreich A, Schmid HP, van Poppel H, et al. EAU guidelines on prostate cancer. Eur Urol. 2005; 48:546–551.

4. Stewart SB, Boorjian SA. Radical prostatectomy in high-risk and locally advanced prostate cancer: Mayo Clinic perspective. Urol Oncol. 2015; 33:235–244.

5. Briganti A, Chun FK, Salonia A, Suardi N, Gallina A, Da Pozzo LF, et al. Complications and other surgical outcomes associated with extended pelvic lymphadenectomy in men with localized prostate cancer. Eur Urol. 2006; 50:1006–1013.

6. Musch M, Klevecka V, Roggenbuck U, Kroepfl D. Complications of pelvic lymphadenectomy in 1,380 patients undergoing radical retropubic prostatectomy between 1993 and 2006. J Urol. 2008; 179:923–928. discussion 928-9.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download