Abstract
Coexistence of emphysematous cystitis and prostatic abscess are rare occurrences. Here, we report a case of emphysematous cystitis and prostatic abscess in a 65-year-old man with a 5-year history of diabetes mellitus. This case was further complicated by the hematogenous spread of Klebsiella pneumoniae infection from the prostatic abscess to the liver and lung. Computed tomography (CT) imaging revealed a localized gas within the urinary bladder and swelling of the prostate, with fluid accumulation. Multiple low-density lesions were observed in liver segments S3, S4, and S7, suggestive of an inflammatory process. Chest CT scan revealed multiple cavitatory nodules of various sizes, with a ground glass appearance of both lung fields, which suggest septic emboli from severe uro-septicemia. The optimal antibiotic therapy was administered, and a holmium laser enucleation of the prostate operation was subsequently performed. On day 37 post-admission, the patient was discharged in a good condition, without any sequelae.
Emphysematous cystitis, a relatively rare infection of the bladder caused by gas-producing bacteria, often occurs in immunosuppressed patients [1]. Prostatic abscess presents in immunosuppressed patients, as well as in internal prosthetic patients and in those who underwent recent prostate biopsy. Although both diseases are common in patients with poorly controlled diabetes mellitus, it is rare for both to simultaneously occur. Herein, we describe a case of emphysematous cystitis concomitant with prostatic abscess, with hematogenous spread of infection to the lung and liver. Despite the short duration of infectious manifestation, pathogens may spread to distant organs via the blood stream with poorly controlled diabetes. We report our experience of this case.
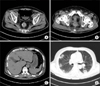
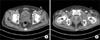
A 65-year-old man presented fever for the past three days with gross hematuria and lower abdominal pain to the nephrology outpatient clinic at our institution. He had been suffering from incomplete voiding and poor stream; however, he was not taking any medication. For the past 5 years, he had been taking medication for type 2 diabetes mellitus and chronic kidney disease, and had a previous cerebral infarction. On the initial examination, his body temperature was 38.5℃, pulse rate was 100 beats per minute, and blood pressure was 140/80 mmHg. His respiratory rate was 16 breaths per minute, and his oxygen saturation was recorded as 98% in ambient air. His abdomen was distended with mild suprapubic tenderness on palpation. According to a digital rectal examination, his prostate gland was mildly enlarged, soft, non-fluctuant, and moderately tender. The blood test results suggested acute kidney injury (creatinine, 3.32 mg/dl; urea, 64.7 mg/dl), infection (C-reactive protein, 24.2 mg/dl; serum white blood cell count, 23,710/mm3), and poorly controlled diabetes mellitus (glycated hemoglobin A1c, 12.5%). Routine urinalysis revealed numerous red- and white-blood cells on high power field examination of the urinary sediment, suggesting urinary tract infection. Plain X-ray images of the kidney, ureter, and bladder revealed gaseous shadows in the lower pelvic area. Plain chest X-ray images revealed a patchy opacification in both lung fields. A computed tomography (CT) scan of the abdomen and chest was subsequently performed. Abdominal CT scan revealed a distended urinary bladder with intraluminal and intramural gas and swelling of the prostate gland with fluid accumulation. This suggested emphysematous cystitis with a concomitant prostatic abscess. In addition, multiple low density lesions were observed in the liver segments S3, S4, and S7, which suggested inflammatory process. Chest CT scan revealed multiple cavitary nodules of various sizes and a ground-glass appearance of both lung fields. These findings were highly suggestive of septic emboli due to severe uro-septicemia (Fig. 1). The patient was admitted to a hospital for empiric antibiotic therapy, urinary bladder catheterization, and strict glycemic control with insulin therapy. Meropenem was used empirically for antimicrobial coverage of gram-negative rods, including extended-spectrum beta-lactamases (ESBL) positive organism and possible anaerobes. By the third day of admission, his blood and urine specimens presented more than 100,000 CFU/ml of Klebsiella pneumoniae, and sensitivity was positive for ceftazidime, cefotaxime, cefepime, ciprofloxacin, and negative for ESBL. By the tenth day of admission, his fever subsided, but K. pneumoniae was still cultured from blood specimens. On the twelfth day, his clinical condition was improved conspicuously, and his blood sugar levels were well controlled. On the fourteenth day, blood and urine cultures were sterile. Blood creatinine level decreased to 1.4 mg/dl (the patient's previous basal level). Twenty-three days after admission, the C-reactive protein level was decreased to 3.7 mg/dl and subsequent abdominal and chest CT scans showed regression of the intraluminal and intramural gas accumulation in the bladder, septic emboli, and inflammatory low density liver lesions. However, the size of the prostatic abscess cavity showed little improvement (Fig. 2). We decided to surgically drain the prostatic abscess. On day 30, holmium laser enucleation of the prostate (HoLEP) operation was performed. Both prostatic lobes were almost fully enucleated. The resected prostate volume was 15 g. The patient was afebrile postoperatively, and subsequent urinalysis revealed no pyuria. His Foley's urinary catheter was removed on the sixth day postoperatively, with no residual difficulty urinating and no abdominal discomfort. The patient was discharged 37 days after admission.
Theoretically, emphysematous cystitis due to urinary tract obstruction caused by a prostatic abscess is possible. However, to date and to the best of our knowledge, only a few cases have been reported in the literature. Although prostatic abscess and emphysematous cystitis are uncommon due to effective antibiotic therapy, these are potentially serious disorders that can, with delayed treatment, lead to death. The mortality rate of prostatic abscess is 3–30% [2]; whereas the prognosis of emphysematous cystitis is generally more favorable, with a mortality rate of about 7% [3]. Its incidence has increased in recent years due to the development and routine use of diagnostic imaging methods. The risk factors for both disorders are similar, including urinary retention (e.g., urinary tract obstruction, neurogenic bladder), underlying disease (e.g., diabetes mellitus, chronic kidney disease, liver cirrhosis, immunocompromised state), and previous urethral procedure (e.g., indwelling catheter, transurethral surgery) [4]. The clinical symptoms of emphysematous cystitis are dysuria, urinary frequency, fever, abdominal pain, and hematuria. In prostatic abscess, symptoms that differentiate the condition from prostatitis include perineal pain, tenesmus, and urinary retention. Palpation of the fluctuant prostate on digital rectal examination should lead to a suspicion of prostatic abscess. However, as clinical features of both disorders are often non-specific, the diagnosis is usually established using imaging techniques, including plain abdominal X-ray, ultrasound, and abdomino-pelvic CT scan. Transrectal ultrasound (TRUS) is especially useful if prostatic abscess is suspected. CT scan is the imaging modality of choice, as it clearly defines the extent and severity of the disease.
Emphysematous cystitis is caused by gas-forming microorganisms, mainly Escherichiacoli and K. pneumoniae. Other pathogens include enterococcus; fungi, such as Candida spp.; and anaerobes, such as Clostridium perfringens [5]. These pathogens are also the leading causes of prostatic abscess [6]. It is thought that bacterial fermentation of glucose and poor tissue perfusion result in the production of carbon dioxide and hydrogen gas bubbles [7], which dissect the necrotizing tissue in the intraluminal space [8].
K. pneumoniae is a rod-shaped, gram-negative bacterium with a prominent polysaccharide capsule. This capsule provides resistance against the host defense mechanisms [9]. A previous study demonstrated that capsular serotypes K1/K2 tend to be more resistant and have more virulence profiles [10]. In the present case, although we did not investigate the serotypes, bacterial serotype could be one of the factors for hematogenous spread of infection to the lungs and liver. The treatment of emphysematous cystitis consists of bladder drainage (infected urine and gas) and antibiotic therapy. Treatments for prostatic abscess include surgical drainage and suprapubic catheterization, since urethral instrumentation may aggravate sepsis. No management guidelines are currently available for the management of emphysematous cystitis concomitant with prostatic abscess in diabetic patients. We decided against cystostomy. Although minimally invasive treatment, such as TRUS-guided needle aspiration or drainage via transperineal or transurethral approach under local anesthesia, is preferred for a prostatic abscess, we performed the HoLEP procedure due to the possibility of a spontaneous rupture of the prostate abscess into the urethra, perineum, or rectum.
In conclusion, emphysematous cystitis and prostatic abscess seldom may coexist. The risk factors associated with each disorder are similar, as are the causative pathogens. Clinical features are often nonspecific, thus the diagnosis is usually confirmed radiographically. The basic treatment strategy combines adequate and appropriate antibiotic administration, timeous surgical drainage, and strict glycemic control in patients with diabetes mellitus. We hope that this case will provide some insight for the management of future cases of emphysematous cystitis concomitant with prostatic abscess.
Figures and Tables
Fig. 1
(A) Distended urinary bladder with intraluminal and intramural gas collection. (B) Swelling of the prostate gland, with fluid accumulation. (C) Ill-defined low-density lesions in sections S3, S4, and S7 of the liver. (D) Multiple cavitatory nodules of various sizes with a ground glass appearance of both lung fields.
References
1. Mokabberi R, Ravakhah K. Emphysematous urinary tract infections: diagnosis, treatment and survival (case review series). Am J Med Sci. 2007; 333:111–116.

2. Brawer MK, Stamey TA. Prostatic abscess owing to anaerobic bacteria. J Urol. 1987; 138:1254–1255.

3. Thomas AA, Lane BR, Thomas AZ, Remer EM, Campbell SC, Shoskes DA. Emphysematous cystitis: a review of 135 cases. BJU Int. 2007; 100:17–20.

4. Wen SC, Juan YS, Wang CJ, Chang K, Shih MC, Shen JT, et al. Emphysematous prostatic abscess: case series study and review. Int J Infect Dis. 2012; 16:e344–e349.

5. Juan YS, Chuang SM, Shen JT, Jang MY, Wu WJ, Wang CJ, et al. Unusual gas pattern in emphysematous cystitis: a case report. Kaohsiung J Med Sci. 2005; 21:44–47.

6. Weinberger M, Cytron S, Servadio C, Block C, Rosenfeld JB, Pitlik SD. Prostatic abscess in the antibiotic era. Rev Infect Dis. 1988; 10:239–249.

7. Sakamoto F, Taki H, Yamagata T, Tsukurimichi S, Ikeda M, Sugiura T, et al. Emphysematous cystitis with severe hemorrhagic anemia resulting from diabetes mellitus type 2. Intern Med. 2004; 43:315–318.

8. Chang CB, Chang CC. Emphysematous cystitis: a rare cause of gross hematuria. J Emerg Med. 2011; 40:506–508.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download