Abstract
Objective
Ventricular enlargement and hydrocephalus after traumatic brain injury (TBI) are relatively common findings. However, selecting patients for shunt surgery is difficult to determine and clinical outcomes after shunt surgery also varies. In this clinical study, we analyzed clinical features and outcomes of hydrocephalus patients who have undergone shunt surgery after traumatic brain injury.
Methods
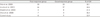
Total of 162 patients underwent shunt surgery between January, 2006 and December, 2010. Among these patients, we reviewed patients' medical records retrospectively and found neuroradiological findings of 17 patients with TBI. We divided patients into two groups: poor response to shunt surgery and good response to shunt surgery. Within each group, we analyzed clinical diagnosis, operation methods to traumatic brain injury, Glasgow coma scale (GCS), computed tomography (CT) scans, radionuclide cisternography and finally the interval between TBI and shunt surgery.
Results
Number of patients divided into each group were 8 and 9, respectively. GCS on traumatic onset of each group were 5.5 and 9.8. And the differences of each group were statistically significant (p=0.020). GCS before shunt surgery were 8.5 and 11.1 respectively. There were no significant differences in age, diagnosis, and interval between TBI and shunt surgery.
References
1. Ban SP, Son YJ, Yang HJ, Chung YS, Lee SH, Han DH. Analysis of complications following decompressive craniectomy for traumatic brain injury. J Korean Neurosurg Soc. 2010; 48:244–250.

2. Bauer DF, McGwin G Jr, Melton SM, George RL, Markert JM. Risk factors for conversion to permanent ventricular shunt in patients receiving therapeutic ventriculostomy for traumatic brain injury. Neurosurgery. 2011; 68:85–88.

3. Beauchamp KM, Kashuk J, Moore EE, Bolles G, Rabb C, Seinfeld J, et al. Cranioplasty after postinjury decompressive craniectomy: is timing of the essence? J Trauma. 2010; 69:270–274.

4. Choi I, Park HK, Chang JC, Cho SJ, Choi SK, Byun BJ. Clinical factors for the development of posttraumatic hydrocephalus after decompressive craniectomy. J Korean Neurosurg Soc. 2008; 43:227–231.

5. De Bonis P, Pompucci A, Mangiola A, Rigante L, Anile C. Post-traumatic hydrocephalus after decompressive craniectomy: an underestimated risk factor. J Neurotrauma. 2010; 27:1965–1970.

6. Honeybul S, Ho KM, Lind CR, Gillett GR. Decompressive craniectomy for diffuse cerebral swelling after trauma: long-term outcome and ethical considerations. J Trauma. 2011; 71:128–132.

7. Kaen A, Jimenez-Roldan L, Alday R, Gomez PA, Lagares A, Alén JF, et al. Interhemispheric hygroma after decompressive craniectomy: does it predict posttraumatic hydrocephalus? J Neurosurg. 2010; 113:1287–1293.

8. Licata C, Cristofori L, Gambin R, Vivenza C, Turazzi S. Post-traumatic hydrocephalus. J Neurosurg Sci. 2001; 45:141–149.
9. Marmarou A, Foda MA, Bandoh K, Yoshihara M, Yamamoto T, Tsuji O, et al. Posttraumatic ventriculomegaly: hydrocephalus or atrophy? A new approach for diagnosis using CSF dynamics. J Neurosurg. 1996; 85:1026–1035.

10. Mazzini L, Campini R, Angelino E, Rognone F, Pastore I, Oliveri G. Posttraumatic hydrocephalus: a clinical, neuroradiologic, and neuropsychologic assessment of long-term outcome. Arch Phys Med Rehabil. 2003; 84:1637–1641.
11. Rahme R, Weil AG, Sabbagh M, Moumdjian R, Bouthillier A, Bojanowski MW. Decompressive craniectomy is not an independent risk factor for communicating hydrocephalus in patients with increased intracranial pressure. Neurosurgery. 2010; 67:675–678. discussion 678.

12. Reddy GK, Bollam P, Shi R, Guthikonda B, Nanda A. Management of Adult Hydrocephalus With Ventriculoperitoneal Shunts: Long-term Single-Institution Experience. Neurosurgery. 2011; 69:774–781.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download