Abstract
Objective
The keyhole site depression is the major cosmetic problem after the frontotemporal craniotomy. Keyhole site bone defect and the temporalis muscle atrophy are the main causes of the keyhole site depression. The purpose of this study is to evaluate the efficacy of temporal mesh plate floating technique for keyhole site depression.
Methods
Total 109 patients who underwent frontotemporal craniotomy from January 2009 to December 2010 were enrolled in this study. The temporal mesh plate floating techniques were performed in 55 patients (Group A), and no other supporting materials were used in the remaining 54 patients (Group B). Each group was divided into single and repeated craniotomy groups for the reason that the repeated craniotomy might result in more severe keyhole site depression. The depth of keyhole site was measured from at least 3-month postoperative brain computed tomography, and the rate of depression was recorded in percentage by comparing to the contralateral side.
Results
The overall rate of keyhole site depression was 11.60% in group A with 9.70% in single craniotomy group and 22.75% in repeated craniotomy group, respectively. The overall rate was 44.57% in group B with 41.43% in single craniotomy group and 49.50% in repeated craniotomy group, respectively. The rate of depression was evidently more severe in group B than group A with statistical significance.
Figures and Tables
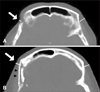 | FIGURE 2The depth of keyhole site was measured from at least 3-month postoperative brain computed tomography (CT), and the rate of depression was recorded in percentage by comparing to the contralateral side (yellow lines). A: Severe keyhole site depression (white arrow) is seen after Rt frontotemporal craniotomy without temporal mesh plate. B: Minimal keyhole site depression (white arrow) is seen after Rt frontotemporal craniotomy using temporal mesh plate. Note the floating configuration (black arrow head) of temporal mesh plate between the keyhole and temporalis muscle. |
 | FIGURE 3Photograph of temporal mesh plate (Synthes GmbH, Oberdorf, Switzerland). It is easily bent into 3-dimensional shape to fit underlying bony contour. |
 | FIGURE 4Intraoperative image (A) and postoperative three-dimensional computed tomography (B) show temporal mesh plate covering the bony defect at the keyhole site. The superior portion of the temporal mesh plate is fixed to the bone flap with self-tapping screws, and the inferior portion is designed to float with some gaps above the bone. |
References
1. Ammirati M, Spallone A, Ma J, Cheatham M, Becker D. An anatomicosurgical study of the temporal branch of the facial nerve. Neurosurgery. 1993; 33:1038–1043. discussion 1044.

2. Appell HJ, Glöser S, Duarte JA, Zellner A, Soares JM. Skeletal muscle damage during tourniquet-induced ischaemia. The initial step towards atrophy after orthopaedic surgery? Eur J Appl Physiol Occup Physiol. 1993; 67:342–347.
3. Badie B. Cosmetic reconstruction of temporal defect following pterional [corrected] craniotomy. Surg Neurol. 1996; 45:383–384.
4. Blaisdell FW, Steele M, Allen RE. Management of acute lower extremity arterial ischemia due to embolism and thrombosis. Surgery. 1978; 84:822–834.
5. Bowles AP Jr. Reconstruction of the temporalis muscle for pterional and cranio-orbital craniotomies. Surg Neurol. 1999; 52:524–529.

6. Brunori A, DiBenedetto A, Chiappetta F. Transosseous reconstruction of temporalis muscle for pterional craniotomy: technical note. Minim Invasive Neurosurg. 1997; 40:22–23.

7. Cheung LK, Samman N, Tideman H. The use of mouldable acrylic for restoration of the temporalis flap donor site. J Craniomaxillofac Surg. 1994; 22:335–341.

8. de Andrade Júnior FC, de Andrade FC, de Araujo Filho CM, Carcagnolo Filho J. Dysfunction of the temporalis muscle after pterional craniotomy for intracranial aneurysms. Comparative, prospective and randomized study of one flap versus two flaps dieresis. Arq Neuropsiquiatr. 1998; 56:200–205.
9. Falconer DT, Phillips JG. Reconstruction of the defect at the donor site of the temporalis muscle flap. Br J Oral Maxillofac Surg. 1991; 29:16–18.

10. Goh DH, Kim GJ, Park J. Medpor Craniotomy Gap Wedge Designed to Fill Small Bone Defects along Cranial Bone Flap. J Korean Neurosurg Soc. 2009; 46:195–198.

11. Horimoto C, Toba T, Yamaga S, Tsujimura M. Subfascial temporalis dissection preserving the facial nerve in pterional craniotomy--technical note. Neurol Med Chir (Tokyo). 1992; 32:36–37.
12. Hwang SW, Abozed MM, Antoniou AJ, Malek AM, Heilman CB. Postoperative temporalis muscle atrophy and the use of electrocautery: a volumetric MRI comparison. Skull Base. 2010; 20:321–326.

13. Joffe JM, McDermott PJ, Linney AD, Mosse CA, Harris M. Computer-generated titanium cranioplasty: report of a new technique for repairing skull defects. Br J Neurosurg. 1992; 6:343–350.

14. Kadri PA, Al-Mefty O. The anatomical basis for surgical preservation of temporal muscle. J Neurosurg. 2004; 100:517–522.

15. Komorowska-Timek E, Gabriel A, Bennett DC, Miles D, Garberoglio C, Cheng C, et al. Artificial dermis as an alternative for coverage of complex scalp defects following excision of malignant tumors. Plast Reconstr Surg. 2005; 115:1010–1017.

16. Lacey M, Antonyshyn O, MacGregor JH. Temporal contour deformity after coronal flap elevation: an anatomical study. J Craniofac Surg. 1994; 5:223–227.
17. Lipa JE, Butler CE. Enhancing the outcome of free latissimus dorsi muscle flap reconstruction of scalp defects. Head Neck. 2004; 26:46–53.

18. Lipira A, Limbrick D, Haughey B, Custer P, Chicoine MR. Titanium mesh reconstruction to maintain scalp contour after temporalis musculofascial flap reconstruction of the floor of the middle cranial fossa: a technical note and report of two cases. Skull Base. 2009; 19:303–309.

19. Mathur KK, Tatum SA, Kellman RM. Carbonated apatite and hydroxyapatite in craniofacial reconstruction. Arch Facial Plast Surg. 2003; 5:379–383.

20. Matsumoto K, Akagi K, Abekura M, Ohkawa M, Tasaki O, Tomishima T. Cosmetic and functional reconstruction achieved using a split myofascial bone flap for pterional craniotomy. Technical note. J Neurosurg. 2001; 94:667–670.
21. Miyazawa T. Less invasive reconstruction of the temporalis muscle for pterional craniotomy: modified procedures. Surg Neurol. 1998; 50:347–351. discussion 351.

22. Oikawa S, Mizuno M, Muraoka S, Kobayashi S. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy. Technical note. J Neurosurg. 1996; 84:297–299.
23. Park J, Hamm IS. Cortical osteotomy technique for mobilizing the temporal muscle in pterional craniotomies. Technical note. J Neurosurg. 2005; 102:174–178.
24. Pennington DG, Stern HS, Lee KK. Free-flap reconstruction of large defects of the scalp and calvarium. Plast Reconstr Surg. 1989; 83:655–661.

25. Pieper DR, Al-Mefty O. Cranio-orbito-zygomatic approach. Operative Technique. Neurosurg. 1999; 2:2–9.
26. Poetker DM, Pytynia KB, Meyer GA, Wackym PA. Complication rate of transtemporal hydroxyapatite cement cranioplasties: a case series review of 76 cranioplasties. Otol Neurotol. 2004; 25:604–609.

27. Rapidis AD, Day TA. The use of temporal polyethylene implant after temporalis myofascial flap transposition: clinical and radiographic results from its use in 21 patients. J Oral Maxillofac Surg. 2006; 64:12–22.

29. Spetzler RF, Lee KS. Reconstruction of the temporalis muscle for the pterional craniotomy. Technical note. J Neurosurg. 1990; 73:636–637.
30. Wright S, Bekiroglu F, Whear NM, Grew NR. Use of Palacos R-40 with gentamicin to reconstruct temporal defects after maxillofacial reconstructions with temporalis flaps. Br J Oral Maxillofac Surg. 2006; 44:531–533.
31. Yaşargil MG, Reichman MV, Kubik S. Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg. 1987; 67:463–466.
32. Yoshioka N, Haraoka G, Muraoka M, Tominaga S. Single stage reconstruction of scalp and skull using free muscle flap and titanium mesh in patients with epidural infection. J Craniomaxillofac Surg. 1996; 24:118–121.

33. Zager EL, DelVecchio DA, Bartlett SP. Temporal muscle microfixation in pterional craniotomies. Technical note. J Neurosurg. 1993; 79:946–947.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download