Abstract
Bleeding from bilateral internal maxillary artery (IMA) injury may result in a life-threatening situation and greater urgency for resuscitation. Here we report a case of life-threatening bleeding of bilateral maxillary arteries in multiple facial bone fractures, which was treated by endovascular treatment. A 77-year-old woman sustained a fall from five meters height. She was transferred to our institution with stuporous consciousness, active oronasal bleeding, multiple facial laceration, facial deformity and both forearm swelling. Selective angiography of bilateral external carotid arteries (ECA) demonstrated contrast extravasation in the distal branches of the right IMA and in the proximal segment of the left IMA involving the left middle meningeal artery. Endovascular embolization with polyvinyl alcohol (PVA) particle successfully stopped bleeding from the bilateral IMA. At one-year clinical follow-up, she recovered without any neurological deficit except some clumsiness of her both hands due to bilateral radioulnar fractures. In patients with life-threatening bleeding from bilateral IMA, endovascular embolization with PVA particle may be considered as a good treatment option.
The incidence of maxillofacial injuries is about 10% in most major trauma centers.3) In patients with maxillofacial injuries, the life-threatening bleeding from the internal maxillary artery (IMA) injury is not frequent but urgent because this injury is associated with airway compromise, intracerebral hemorrhage, cervical spine injury, and massive oronasal bleeding.2,7) However, there are very few recommendations for its treatment. Here we report a case of life-threatening bleeding of bilateral IMAs in multiple facial bone fractures, which was successfully treated by endovascular treatment (EVT).
A 77-year-old woman sustained a fall from five meters height. She was transferred to our institution with stuporous consciousness, active oronasal bleeding, multiple facial laceration, facial deformity and both forearm swelling. Her initial Glasgow Coma Scale (GCS) was 8. Her blood pressure (BP) was 99/57 mmHg and heart rate was 78 beats per minute (bpm). Initial hemoglobin (Hb) was checked as 10.6 g/dL. The patient had been taking aspirin due to a past medical history of unstable angina. Initially, the patient was intubated endotracheally to prevent obstruction of the airway and nasal packing was performed with inflatable nasal balloon catheters. Brain and facial computed tomography (CT) showed multiple facial bone fractures and pneumocephalus without intracranial hemorrhage (Figure 1). Oronasal bleeding persisted during and after the CT scans. BP and Hb were down to 65/47 mm Hg and 6.1 g/dL, respectively. An 8,600-mL blood transfusion (16 units of packed red blood cells and 11 units of fresh frozen plasma) was given. BP was unstable at around 80 mmHg and Hb was checked as 6.6 g/dL. Thus, the patient underwent emergent conventional angiography. Selective angiography of right external carotid arteries (ECA) demonstrated contrast extravasation in the distal branches of the IMA (Figure 2A). Immediately, endovascular embolization was performed with polyvinyl alcohol (PVA) particles (range of particle size, 250-350 microns). After the embolization, the right ECA angiography demonstrated disappearance of the extravasation in the distal branches of the right IMA (Figure 2B). Selective angiography of left ECA showed contrast extravasation in the proximal segment of the left IMA involving the left middle meningeal artery (MMA) (Figure 2C). After embolization of the left IMA with PVA particles (range of particle size, 250-350 microns), the IMA segment involving the MMA was occluded and the extravasation was disappeared (Figure 2D). Additional 3,000 mL blood transfusion (5 units of packed red blood cells and 5 units of fresh frozen plasma) was given after the endovascular embolization.
On the morning on the next day after the embolization, BP was stabilized at about 120/80 mmHg and Hb was checked as 10.1 g/dL. After 2 weeks, plastic surgery for the facial bone fractures and orthopedic surgery for both radioulnar fractures were performed. Although the patient was inconvenient with clumsiness of her both hands due to bilateral radioulnar fractures, she recovered without any neurological deficit at one-year clinical follow-up.
In patients with maxillofacial fractures with massive oronasal bleeding, adequate airway protection should be considered first in order to protect the life-threatening problems such as aspiration and airway obstruction. In patients with life-threatening bleeding after panfacial fractures, there can be many causes other than oronasal bleeding responsible for the patient's condition. Pelvic bone fractures, splenic rupture, liver laceration, and mesentery tears may also cause massive bleeding and should be excluded.1)
The main vessel responsible for intractable bleeding after panfacial fracture is the IMA and the interosseous branch of the ECA, as well as its branches. In most mild to moderate bleeding, nasal packing or tamponade with balloon catheters are thought to be effective procedures.2,7) In cases of severe oronasal bleedings, however, tight oronasal packing is frequently ineffective because the bleeding may originate from the oral cavity, not the nasal cavity.9,11) In patients with multiple facial bone fractures, there is only soft tissue but no solid wall for the packing to stop massive bleeding in the oronasal cavity.7) When the injury is located at or proximal to the second part of the IMA, which is defined as lateral to the lateral pterygoid muscle, adequate bleeding control cannot be achieved by the packing.6)
Ligation of the ECA has been suggested as an alternative treatment, but it has failed to show consistent efficacy in stopping bleeding.2) It is difficult to identify the exact injured vessels among the complicated anatomic structures, and there are abundant collateral vessels responsible for bleeding recurrence. Immediate temporary reduction of the fracture bone is suggested as another choice for controlling bleeding.1,10) However, there are some disadvantages. It has some risks for the critical patient undergo general anesthesia and it is difficult to perform reduction of the fracture bone because of massive bleeding and severe tissue swelling.12)
Angiographic intervention is useful for diagnosing and locating the injured vessel and providing a therapeutic method for embolization of the bleeders. Endovascular embolization is considered the better choice for stopping intractable oronasal bleeding.2,7,12) Sakamoto et al.8) described the first series of treatment by angiographic embolization in patients with severe oronasal bleeding after blunt maxillofacial trauma. They performed carotid angiography in 13 patients, and 4 patients had extravasation of contrast media from the ECA. Successful bleeding control was achieved in 4 patients by endovascular embolization. They treated other 9 patients with nasal packing. Bleeding focus from the ICA was visualized by angiography in 8 of the 9 patients, but all these patients failed to stop bleeding. Komiyama et al.7) reported six patients with bilateral vessel injuries after trauma, five of which had received blood transfusions of more than 10,000 mL. Two of them died, two were in a vegetative state, on e had moderate disability; only one patient had a good recovery. In our case, the patient recovered without any neurological deficit after endovascular embolization, even though the patient had mild disability with her hands due to bilateral radioulnar fractures.
Compared with surgical treatment, endovascular embolization has the distinct advantages of distal access near the bleeding points, demonstration of bleeding points, control of multiple bleeding points, repeatability, no necessity for general anesthesia, and short procedure time.7) Avoidance of general anesthesia is particularly of benefit for multiple trauma patients with a compromised hemodynamic status. On the contrary, there are possible complications of endovascular embolization including soft tissue necrosis, blindness, facial nerve palsy, and migration of the embolus into the internal carotid or vertebral artery exist.2,4,5,7) Therefore, selective arterial embolization has been suggested, and it should be performed as close to the bleeding point as possible to prevent tissue necrosis.2,7) For the selective arterial embolization, PVA particle is effective than other embolization materials. A variety of particle sizes (40 to 1,180 microns) fit for various vessel sizes and the clinician can control the contrast/saline ratio to achieve the desired suspension and enhance fluoroscopic visualization.
Figures and Tables
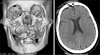 | FIGURE 1Brain (on the right side) and facial computed tomography (on the left side) showed multiple facial bone fractures and pneumocephalus without intracranial hemorrhage. |
 | FIGURE 2A: Selective angiography of right external carotid arteries (ECA) demonstrated contrast extravasation in the distal branches of the internal maxillary artery (IMA). B: After the embolization, the right ECA angiography demonstrated disappearance of the extravasation in the distal branches of the right IMA. C: Selective angiography of left ECA showed contrast extravasation in the proximal segment of the left IMA involving the left middle meningeal artery (MMA). D: After embolization of the left IMA with PVA particles (range of particle size, 250-350 microns), the IMA segment involving the MMA was occluded and the extravasation was disappeared. |
References
1. Ardekian L, Samet N, Shoshani Y, Taicher S. Life-threatening bleeding following maxillofacial trauma. J Craniomaxillofac Surg. 1993; 21:336–338.

2. Bynoe RP, Kerwin AJ, Parker HH 3rd, Nottingham JM, Bell RM, Yost MJ, et al. Maxillofacial injuries and life-threatening hemorrhage: treatment with transcatheter arterial embolization. J Trauma. 2003; 55:74–79.
3. Chen CC, Jeng SF, Tsai HH, Liliang PC, Hsieh CH. Life-threatening bleeding of bilateral maxillary arteries in maxillofacial trauma: report of two cases. J Trauma. 2007; 63:933–937.

4. Elahi MM, Parnes LS, Fox AJ, Pelz DM, Lee DH. Therapeutic embolization in the treatment of intractable epistaxis. Arch Otolaryngol Head Neck Surg. 1995; 121:65–69.

5. Elden L, Montanera W, Terbrugge K, Willinsky R, Lasjaunias P, Charles D. Angiographic embolization for the treatment of epistaxis: a review of 108 cases. Otolaryngol Head Neck Surg. 1994; 111:44–50.

6. Hashim HA, Atiyeh BS, Kayle DI, Dandan I. Balloon compression of the intramaxillary sinus for intractable post-traumatic bleeding from the maxillary artery. Case report. Scand J Plast Reconstr Surg Hand Surg. 1999; 33:321–324.
7. Komiyama M, Nishikawa M, Kan M, Shigemoto T, Kaji A. Endovascular treatment of intractable oronasal bleeding associated with severe craniofacial injury. J Trauma. 1998; 44:330–334.

8. Sakamoto T, Yagi K, Hiraide A, Takasu A, Kinoshita Y, Iwai A, et al. Transcatheter embolization in the treatment of massive bleeding due to maxillofacial injury. J Trauma. 1988; 28:840–843.

9. Schaitkin B, Strauss M, Houck JR. Epistaxis: medical versus surgical therapy: a comparison of efficacy, complications, and economic considerations. Laryngoscope. 1987; 97:1392–1396.
10. Shimoyama T, Kaneko T, Horie N. Initial management of massive oral bleeding after midfacial fracture. J Trauma. 2003; 54:332–336. discussion 336.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download