Abstract
We report a patient who developed multiple focal cerebral infarctions after epidural hematoma evacuation. A 41-year-old man presented with altered mentality after sustaining a head trauma. Computer tomography (CT) scan showed large epidural hematoma at the left hemisphere. The patient underwent emergency evacuation of the hematoma and decompression surgery. Three days after the surgery, the patient showed right side hemiparesis. CT and MR diffusion weight images (MRDWI) revealed multiple infarctions at focal posterior cerebral artery (PCA) and middle cerebral artery (MCA) territories and subcortical parenchyma. Several months after the surgery, the patient showed improved mentality, but his cognition and hemiparesis were not improved as much. Before ischemic change occurs, it is vital to administer early, rapid and aggressive management are required to prevent posttraumatic cerebral infarction.
The cerebral infarction after head trauma (e.g. epidural hematoma, subdural hematoma, traumatic subarachnoid hematoma or contusion, etc.) occurs with a frequency ranging from 1.9% to 10.4%.6) Several mechanisms may account for this complication: direct vascular compression, cerebral vasospasm, vascular injury, embolism, and hypoperfusion.6,10-13) The common cause of post-traumatic cerebral infarction is vascular compression with focal mass effect in which the major intracranial vessels are frequently involved and small perforating vessels are also involved.1,13) Another cause of post-traumatic cerebral infarction is without mass effect such as vessel dissection or thrombosis.13) Recently, a few studies reported some cases and each mechanism was known to uncommon. We report a case of multiple type cerebral infarctions following intracranial hematoma after head injury with clinical, radiological features and the literatures are reviewed.
A 41-years-old man was found on a street and came to emergency center with altered mentality. He was chronic alcoholics and had a history of liver cirrhosis. He showed stuporous mentality and Glasgow Coma Scale score (GCS) of 5. Left pupil was dilated and fixed. He was resuscitated right then, and brain CT revealed epidural hematoma (EDH) with 4 cm depth at left fronto-temporo-parietal lesion (Figure 1). An urgent craniotomy and evacuation of the hematoma was done.
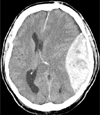
After the surgery, the patient improved mentality with GCS of 9. Postoperative CT revealed successful decompression, only focal hemorrhage combined small low density region was found at left occipital lobe (Figure 2). But the patient did not showed neurological dysfunction compatible to this lesion, and improved motor strength bilaterally than pre-operation. But after three days, decreased mentality (GCS of 8) and right side hemiparesis were developed. We evaluated MR diffusion weight images (MRDWI) scan first, it revealed new small multiple infarctions evolving left posterior cerebral artery (PCA) area which seemed to involve one of the terminal divisions, subcortical lesions and left basal ganglia (Figure 3). These lesions were not found in initial or post operative CT scan. A few days after followed CT scan showed multiple low density lesions which were corresponding with MRDWI. We diagnosed acute infarction. The patient underwent tracheostomy, and further ICU treatment focusing on hemodynamic therapy during a few weeks. After several months, he was able to perform many rehabilitative active with the help of the others, but the cognitive function and right hemiparesis did not show any significant improvement.
The major cause of infarction following head trauma is compression of the artery by mass effect such as hematoma. It is related to brain herniation and distortion, compressive effects of intracranial hematoma or severe cerebral edema, vasospasm, direct vascular injury (e.g. laceration or dissection), embolism, or injury to cortical vessels with skull fractures.2,5) Hippocampus, basal ganglia, cerebral cortex, and cerebellum are the most common sites of infarction.6) The patterns of infarct include the arterial territory, boundary zone (watershed infarction), and nonterritorial-nonboundary cerebral infarctions. Territorial infarction is defined cerebral vascular territory, involving entire or a part of it. Boundary cerebral infarction is well circumscribed hypodense lesions in boundary zones between the vascular territories. Nonterritorial-nonboundary infarction is single or multi focal lesions without a precise localization.2,5) Mirvis et al.,6) Server et al.13) and Marino et al.5) found that territorial cerebral infarctions were most common pattern, especially PCA territory infarction, than boundary zone infarction. And cortical infarctions were more common than subcortical infarction. In case of PCA, infarct occurs due to rapid increase of supratentorial pressure reading to herniation and this compromise of PCA due to compression against free edge of tentorium.8,14) In several studies, infarction in the PCA distribution of the occipital lobe was the most common.6,13) In case o is usually due to fixed M1 segment on the posterior margin of sphenoid lower wing.7) This can lead to subintimal in-jury and occur thrombosis or arterial dissection, occlusion of the vessels finally.3,14,15) MCA infarct can also occur from small perforating branches occlusions, secondary to displace-ment of midline cerebral structures due to a mass effect of the hematoma.8) In our case, follow up radiological images revealed boundary and multiple nonterritory-nonboundary cerebral infarctions, not vascular territory. So we did not evaluate further vascular studies such as cerebral angio-graphy.
The mass effects can lead infarction also where territory of small perforating vessels such as lenticulostriatae or thalamoperforating arteries.6) Server et al.13) report a case of the lateral lenticulostriatae infarction found in a supraclinoid artery dissection patient. In our case, after three days of surgery, multiple watershed infarction between the left MCA and PCA terminal branches in left temporal lobe, and acute left basal ganglia infarction were also found.
Focal infarction of the cortex or subcortical region can result from direct compression by overlying masses, such as EDH.13) These infarcts may result from direct pressure effect, decreasing arterial flow, and may be secondary to local venous drainage block.13) Such infarcts extend beyond arterial vascular territories and may be hemorrhagic.13) In our case, infarction of the cortex and subcortical region, overlying epidural hematomas produced significant mass effect on the underlying cortex, leading to subcortical infarction (Figure 3). Also, infarction with hemorrhagic change was found in the subcortical lesion of occipital lobe (Figure 2).
Another cause of posttraumatic infarction is vasospasm. Several studies suggest that intracranial vasospasm in association with traumatic subarachnoid hemorrhage can be a cause of infarction following trauma.15) And Kakarieka et al.4) demonstrated that the outcome of patients with traumatic subarachnoid hemorrhage was significantly worse than that of patients whose initial CT did not show subarachnoid hemorrhage.13) Our patient did not have initial subarachnoid hemorrhage, so we did not perform angiography or other vascular evaluations for vasospasm.
There are few well-established therapies for traumatic brain injury.5) Owing to the complexity of factors that influence outcome, clinical trials have been difficult to design and conduct. Several trials that have been performed in recent years failed to demonstrate a significant improvement in outcome, despite promising preclinical data.5,9)
Hemodynamic changes occur in severe brain injury: hypoperfusion, hyperemia and vasospasm. For better outcome for post traumatic ischemic patients, reduction of these changes is important hemodynamic treatment under the intensive monitoring. Some studies reveal that for a purpose of prevention, continuous anticoagulant therapy or inotropics infusion can decrease ischemic changes.6,8)
Not only medical therapy, but also early detection of ischemic change is important. Recent studies demonstrate that CT can be considered as an early diagnosis and outcome measurement.5)
Traumatic brain injury has high mortality, and accompanied posttraumatic cerebral infarction may increase a risk of mortality, hospitalization date and residual disability. To prevent multiple post traumatic infarction, early evaluation and rapid aggressive management are required before occurrence of ischemic changes.
Figures and Tables
FIGURE 2
Postoperative CT scan shows successful evacuation and focal low density around the left parieto-occipital sulcus.
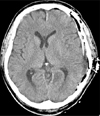
FIGURE 3
MRDWI reveals multiple nodular and patchy high signal increase lesions in medial part of left temporal lobe. This is PCA and MCA terminal branch territory. Subcortical lesion of left occipital lobe (A), cortical lesions and left basal ganglia infarction were also noted (B, C, D). MRDWI: MR diffusion weight images, PCA: posterior cerebral artery, MCA: middle cerebral artery.

References
1. Busch G. [Cerebral infarct following trauma.]. Rofo. 1985; 143:20–23.
2. Graham DI, Adams JH, Doyle D. Ischaemic brain damage in fatal non-missile head injuries. J Neurol Sci. 1978; 39:213–234.

3. Jacques S, Shelden CH, Rogers DT Jr, Trippi AC. Posttraumatic bilateral middle cerebral artery occlusion. Case report. J Neurosurg. 1975; 42:217–221.
4. Kakarieka A, Braakman R, Schakel EH. Clinical significance of the finding of subarachnoid blood on CT scan after head injury. Acta Neurochir (Wien). 1994; 129:1–5.

5. Marino R, Gasparotti R, Pinelli L, Manzoni D, Gritti P, Mardighian D, et al. Posttraumatic cerebral infarction in patients with moderate or severe head trauma. Neurology. 2006; 67:1165–1171.

6. Mirvis SE, Wolf AL, Numaguchi Y, Corradino G, Joslyn JN. Post-traumatic cerebral infarction diagnosed by CT: prevalence, origin, and outcome. AJNR Am J Neuroradiol. 1990; 11:355–360.

7. Mobbs RJ, Chandran KN. Traumatic middle cerebral artery occlusion: case report and review of pathogenesis. Neurol India. 2001; 49:158–161.
8. Moros-Peña M, Ruiz JA, Molina I, Abenia P, Melendo J, López-Pisón J. [Ischemic stroke of middle cerebral artery territory after the traumatic epidural hematoma.]. Rev Neurol. 1999; 28:978–981.
9. Narayan RK, Michel ME, Ansell B, Baethmann A, Biegon A, Bracken MB, et al. Clinical trials in head injury. J Neurotrauma. 2002; 19:503–557.

10. Pasqualin A, Vivenza C, Rosta L, Licata C, Cavazzani P, Da Pian R. Cerebral vasospasm after head injury. Neurosurgery. 1984; 15:855–858.

11. Rothfus WE, Goldberg AL, Tabas JH, Deeb ZL. Callosomarginal infarction secondary to transfalcial herniation. AJNR Am J Neuroradiol. 1987; 8:1073–1076.
12. Sato M, Tanaka S, Kohama A, Fujii C. Occipital lobe infarction caused by tentorial herniation. Neurosurgery. 1986; 18:300–305.

13. Server A, Dullerud R, Haakonsen M, Nakstad PH, Johnsen UL, Magnaes B. Post-traumatic cerebral infarction. Neuroimaging findings, etiology and outcome. Acta Radiol. 2001; 42:254–260.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download