Abstract
Objective
The morbidity and mortality are high for traumatic upper cervical spine instability with cervico-medullary compression. In a clinical retrospective study, the clinical and radiographic results of occipitocervical (OC) fusion using posterior atlantoaxial transpedicular screw fixation in 12 patients with traumatic upper cervical spine instability was reviewed.
Methods
Twelve patients with traumatic upper cervical spine instability (8 males and 4 females) were treated at our department over four years. Instability resulted from acute C1-C2 dislocation (4 cases), an acute unstable C2 fracture (1 case), acute C1-2-3 fracture dislocation (2 cases), acute C1 fracture (1 case), OC dislocation (2 cases) and old unstable C2 fracture (1 case). All 12 patients were internally fixed with occipital-/C1-C2 transpedicular screw fixation. The outcome (mean follow-up period, 16.5 months) was based on clinical and radiographic review using the Japanese Orthopedic Association (JOA) score.
Results
Four neurologically intact patients remained the same after surgery. Among eight patients with cervical myelopathy, clinical improvement was noted in six cases (75%). The JOA score of the 8 patients were 9.4 (range, 0-16) before surgery and 12.1 (range, 0-17) with a recovery rate of 38.3% at the time of the last follow up. One patient died 2 months after the surgery because of pneumonia and sepsis. Fusion was achieved in 10 patients (90.9%) by the last follow-up.
Instability after trauma to the upper cervical spine is a difficult diagnostic and therapeutic problem due to the complex anatomical structures and biomechanical characteristics of this legion. These injuries may cause an immediate fatality or delayed deterioration of neurological function.5,7) Many authors have reported excellent results after OC fixation using various internal fixation instruments, including the wire-rod system and the screw-plate system, which are currently widely used.20,24) The goals of internal fixation are to achieve anatomic alignment, to protect the neural elements, and to stabilize the spine while preserving the motion of normal elements as well as producing "functional decompression". The clinical course of 12 patients was reviewed to evaluate the outcome, complications and effectiveness of posterior atlantoaxial transpedicular screw fixation with traumatic upper cervical spine instability.
From 2005 to 2009, 12 patients underwent OC internal fixation surgery at our institution. Their medical records and imaging studies were retrospectively reviewed. They had been followed for a mean of 16.5 months (range, 3-36 months). Eight males and 4 females, with a mean age of 48.8 (range, 45-74 years) were included as patients. The causes of traumatic upper cervical spine instability were acute C1-C2 dislocation (4 cases), acute C1-2-3 fracture dislocation (2case), acute OC dislocation (2 cases), acute unstable C2 fracture (1 case), acute C1 fracture (1 case) and an old unstable C2 fracture (1 case). Each patient underwent preoperative radiological evaluation with X-ray, CT and MRI scanning of the OC region. Instability of the upper cervical spine was diagnosed if the atlantodental interval was shifted by more than 3 mm on dynamic X-rays and if pathological movement associated with neurological symptoms (subjective and objective). In patients with severe trauma, dynamic X-rays were not performed in order to avoid pain and to prevent neurological deterioration. Treatment was chosen after consideration of a number of different factors, including the general medical condition of the patient, the severity and location of the fracture, compression of the spinal cord, degree of instability and the neurological status. If cervical spine mal-alignment was present, attempts were initially made to reduce the dislocation using cervical traction except in case with OC dislocation. A cervical MRI was performed to evaluate spinal cord compression. The need for a laminectomy was evaluated based on the clinical findings of either cervical myelopathy or radiculopathy, and the presence of spinal cord compression on MRI. If posterior decompression of the spinal cord was necessary, posterior decompression was performed at the same surgery as the fusion procedure. C1-C2 transpedicular screw fixation methods were used for all 12 patients (Figure 1). Before surgery, all patients had 3D-reformatted CT scanning for preoperative planning. We measured the diameters of the C-1 pedicles, the trajectory angles of the C-1 pedicle screws, and the length of the tracts were determined. Anteroposterior and lateral radiographs were obtained immediately after surgery and monthly for at least 6 months, and a hard cervical collar was worn for at least 3 months postoperatively. All autologous iliac crest (10 patients) allografts were harvested, and the exposed bone on C1 and C2 was decorticated prior to graft placement. The graft was carefully fashioned to fit precisely to the prepared decorticated posterior surface of C1 and C2. Patients were then followed in the outpatient clinic. All patients underwent both anteroposterior/lateral/dynamic plain radiographs and cervical CT scanning to assess screw placement and the rate of fusion. Fusion was assessed principally by CT scans or by dynamic plain radiography, if patients could not have a CT scan during the follow up period. Solid fusion was defined as successful if two criteria were met: 1) the presence of a homogeneous fusion mass visualized between the graft and bone on CT scans; 2) there was no pathological movement between the fused motion segments in flexion and extension views on the cervical X-ray studies. The clinical conditions before and after the surgery was assessed using the Japanese Orthopedic Association (JOA) scoring system.19) The JOA score was assessed before the operation, at discharge, and at one and six months of follow up as well as at the last follow up visit. The total JOA score assessed motor and sensory functions of the four extremities and sphincter contraction, which was a total of seventeen points (Table 1). The neurological recovery rate was calculated as follows: (postoperative JOA score-preoperative JOA score)/(full score-preoperative JOA score) ×100. The neurological recovery rate was ranked as excellent (75-100%), good (51-74%), fair (25-50%), poor (0-24%), or worse (<0%). Comorbidity and complications were recorded to evaluate the risk of surgery.
Table 2 shows the clinical data one the 12 patients with traumatic upper cervical spine injuries that had fusion procedure after diagnosis by imaging. Preoperatively, all patients reported significant neck pain, stiffness or radiculopathy. Eight patients presented with myelopathy. The neck pain improved in all patients and no new instability developed at the level of fusion. At the last follow-up examination, 11 patients (91.6%) had a satisfactory fusion and were independent in their activities of daily living. All 4 neurologically intact patients remained intact after surgery. Among 8 patients with cervical myelopathy, 6 patients (75 %) had improvement of their JOA scores at the last follow-up. The JOA score of the 8 patients were a mean of 9.4 (range, 0-16) before surgery and 12.1 (range, 0-17) with a recovery rate of 38.3 % at the time of the last follow up. One of the patients, who had an OC dislocation with quadriplegia due to a motor vehicle accident, died 2 months after the surgery. After OC fusion, the patient had pneumonia and sepsis due to long term use of mechanical ventilator and decreased pulmonary function (Figure 2). The postoperative course of the other patients was uncomplicated. Wearing a hard cervical collar for at least 3 months, the patients were discharged 10 to 21 days after surgery. There was no further deterioration within 3 months after the operation.
Immediately after the operation, plain cervical X-ray images showed restoration of bone alignment in all patients. Postoperative imaging studies confirmed excellent instrument fixation and no abnormal lesion related to surgery in all patients. Post operative X-rays at 6 months did not reveal instrument loosening or breakage. During up to 12-months of follow up, the plain radiographs did not show any changes in the instrument position when compared to the immediate post operative radiographs. Dynamic plain radiographs in 2 patients and CT scans in eight patients were obtained to assess the fusion during the follow up period. Among the eight patients that had postoperative CT scans, solid fusion was found in 7 patients (87.5%). For the two patients that had dynamic plain radiographs to assess fusion, there was no pathological movement noted after surgery in either case. The true solid fusion rate diagnosed by postoperative CT was 87.5%. Failed fusion case occurred in a 68-year-old patient with traumatic C1-2-3 dislocation and osteoporosis (T-score: -3.2) who received an occiput to C4 fusion with screw fixation. According to the fusion criteria used, the overall rate of fusion was 90.9% in 10 patients with one case of non-union (9.1 %) at last follow up.
There was one case of vertebral artery (VA) injury during the operation, which occurred during the exposure of the C1 lateral mass. The posterior arch of C1 was dissected using a bipolar coagulator and the dissection proceeded too much of the lateral side. The bipolar coagulator tip injured the left VA. The bleeding was controlled intra-operatively using thrombin-soaked gel. On immediate angiographic evaluation, there was evidence of VA injury which was occluded by thrombus formation. Coil embolization of the left VA was performed (Figure 3). The patient was monitored very carefully after surgery, no specific treatment was required. The patient showed no symptoms related to the VA injury.
Treatment of trauma to the upper cervical spine is challenging for neurosurgeons, it is the primary indication for OC fusion. Patients may present with progressive myelopathy, pain, lower cranial nerve dysfunction, or deformities of the craniocervical region.3,20) The 5-year experience at a single center was reviewed for the clinical outcome, radiologic results and operative morbidity associated with the treatment of trauma to the upper cervical spine.
The effectiveness of the operative procedures reported was demonstrated by the fact that each patient was either stabilized or improved at the last follow up. Although there is no standardized grading system to clinically evaluate patients with cervical myelopathy, studies usually use a myelopathy grading system such as the JOA score and the Nurick Scale. In this series, 6 patients (75% of patients) had improvement on their JOA scores with regard to symptoms after the operation. These results are consistent with the 75% to 95% rates reported in the medical literature11) Significant neurological improvement (recovery rate >50%) was demonstrated in 50% of the patients. These results are consistent with other reports indicating a 30% to 40% improvement in myelopathy.3) Traumatic atlanto-occipital dislocation with survival is rare, as the neurological consequences are usually immediately fatal. In this series, one patient had an OC dislocation with resulting quadriplegia and died at 2 months after the surgery. The patient was bedridden for 2 months and died of pneumonia and sepsis.
Many investigators have discussed postoperative fusion rates in traumatic upper cervical spine injuries where OC or atlantoaxial fusion has been performed. The rate of fusion of traumatic upper cervical spine instability lesion has been remarkably successful. The rate of fusion range from 75% to 100%.10,21,30) The fusion rates with the screw based constructs are 90% to 100%.23) In this study, the our overall rate of fusion was 90%, consistent with the rates previous reported with this procedure. Non-union associated with pseudoarthrosis occurred in one patient with a traumatic C1-C2-C3 dislocation and osteoporosis (T-score: -3.2). The CT scan showed non-union at the bone fusion site probably as a consequence of poor bone quality (osteopenic bone) without neurological impairment. This result suggests that wiring may be superior to screws in patients with poor underlying bone (e.g., osteoporosis) which provides poor support for metal implants.31) However, further study is needed to confirm this. Although pseudarthrosis was observed, this patient was of advanced age (over 65 years old) but no neurological symptoms. Revision surgery was not performed in this patient. Fusion surgery will be considered if further instrumentation failure and/or neurological symptoms develop.
Potential intraoperative complications include excessive venous hemorrhage, neural tissue injury, VA injury, and dural lacerations. Most venous bleeding occurs during the exposure of the C1 lateral mass or C2 pars interarticularis which can be prevented by maintaining a subperiosteal plane of dissection. Hemostatic agents such as thrombin-soaked Gelfoam, or powdered Gelfoam can be used if necessary. One of the most troubling complications is damage to one or both vertebral arteries. Screw-based (plate or rod) constructs have been shown to be effective for treating atlantoaxial instability. However, despite the increased stability provided by the transarticular screw technique, there is the potential for VA damage and subsequent catastrophic neurological injury. A recent survey of neurosurgeons showed that the known rate of VA injury was 2.4% and of suspected injury 1.7% per patient treated.32) In addition, the frequency of VA anomalies in the atlantoaxial region has been reported as 2.3%.32) One of the most common anatomical variants that places a patient at greater risk of VA injury is a high-riding transverse C2 foramen.22) Bilateral transarticular screw fixation across C1-C2 may be contraindicated or impossible in up to 20% of patients because of structural variations such as anomalous course of the VA. When encountering these situations, unilateral transarticular screw fixation could be alternative method of C1-C2 arthrodesis for managing atlantoaxial instability.14) In other technique of atlantoaxial fixation, lateral mass screws are placed in the atlas which is connected via a rod or plate to the C2 pedicle or pars interarticularis screws.8,12,28) Many believe that the risk of VA injury is less with this technique compared to transarticular screw placement. Because an axial screw travels just medial to the transverse foramen using this technique, there is still the potential for VA injury. The potential for VA injury where the C1-C2 screw fixation technique is used can be minimized with careful screening using preoperative computed tomographic angiogram. If VA injury occurs, the bleeding is initially controlled by placing a screw in the drill hole. Prompt angiographic evaluation is performed postoperatively. If there is evidence of VA injury, and the injured artery is still partially patent, it should be occluded provided the contralateral vessel is normal (Figure 3). This avoids the later development of an arterial dissection, pseudoaneurysm or arteriovenous fistula.
The highly specialized anatomy of the cervicovertebral junction (CVJ) region has contributed to the development of a variety of fusion techniques for stabilization. Fusion procedures at the CVJ region must be capable of withstanding the forces of compression, axial loading, flexion, extension and rotation. Rod and wire techniques are associated with lower rates of arthrodesis than rigid screw/rod systems, this is probably due to the biomechanical differences.4,18) Fusion rates of rod-and-wire techniques are reported to approach 80%.9,10) Rod and wire techniques often require postoperative halo immobilization and fusion of additional mobile segments for adequate strength, and are associated with complications from the passage of sublaminar or suboccipital wires, including dural lacerations and neurological injuries.15,26,27,29) The major advantages of the rod-and-wire techniques are greater ease of application and decreased risk to neurovascular structures. Continued development has led to the development of biomechanically superior segmental screw-based constructs for CVJ fusions.15,21) Screw-based constructs are technically demanding and require operative precision and expertise when placing screws in the cervical vertebrae.11,17) The transarticular screw fixation is effective and the fusion rates are reported to approach 100%.6,10,16) The transarticular screw traverses four cortical surfaces and fixes the two vertebrae anteriorly and posteriorly, which eliminates translational motion and rotatory motion. The construct is biomechanically superior to posterior graft-and-wire-augmented procedures, postsurgical orthosis are not needed after these procedure.9)
Despite its efficacy, the transarticular screw procedure has several drawbacks. When the C1 posterior arch is congenitally deficient, broken after trauma, or in need of decompression, the procedure may not be suitable. An anomalous course of the VA can place the patient at risk for inadvertent injury to the vessel during the placement of the screws. The pro cedure requires preliminary reduction of the atlantoaxial complex before screw placement. Incomplete reduction of C1-C2 lesions is a significant risk factor for VA injury during the placement of screw instrumentation.16) In the present study, atlantoaxial transpedicular screw fixation was used for OC fusion. Posterior atlantoaxial transpedicular screw fixation is used to treat reducible atlantoaxial subluxation. The procedure can provide immediate stability, and reduce the need for postoperative external orthoses. Although, complications of the approach seldom have been reported, one of troublesome complication associated with C1 lateral mass screw placement is the possibility of the development of C2 neuralgia after atlantoaxial transpedicular screw placement. There is no need to sacrifice the C2 ganglion bilaterally or to expose the C2 isthmus. Surgeons do not need to drill the inferior surface of the lateral aspect of the atlas' posterior arch. Thus, the operative time can be shortened, troublesome venous bleeding prevented, and blood loss during the procedure reduced. This technique is simple and easy to perform and can decrease the risk of vessel and/or neural damage. It can be an effective alternative procedure for the treatment of atlantoaxial subluxation. To reduce injury of neurovascular structures, 3D-reformatted CT scan are always obtained before surgery. Nowadays, 3D-reformatted CT scanning provides information on the anatomical features of C1-C2 and the path of the VA. Before surgery, a clear understanding of the anatomical landmarks essential in determining the entry points for the screw trajectory can be planned. The entry point of the screw is measured in millimeters from the mid portion of C1-C2. The screw trajectory is defined as the number of degrees from both the parasagittal plane and the dorsal or ventral position of the screw relative to the VA foramen. In addition, the height of the unilateral C1 pedicle is always measured and assessed. Improper screw placement might break through the inferior surface of the C1 pedicle into the C1 lateral mass. To prevent the problem of a potential breakthrough, a smaller-diameter screw can be used. In the cases reported here, no complications or loss of fixation occurred. The strength of the posterior transpedicular screw fixation is greater than lateral mass screw fixation, this is because the trajectory of the posterior arch and the pedicle into the C1 lateral mass. The trajectory of the C2 transpedicular screw is from the cortex of the C2 inferior process and pedicle into the C2 lateral mass.
The indications for fusion, in patients with traumatic upper cervical spine instability, an extensive posterior instrumentation fixation procedure that sacrifices the motion of the occiput and C1-C2 complex, are controversial.1,2,13,23-25,30) Failed fusions might be due to use of an inappropriate method of rigid internal fixation or of an inappropriate fusion level. The determination of the level of fusion is one of the most important factors for achieving a complete fusion. Reducibility should be determined in deciding on the level of fusion. Depending on the reducibility and status of the posterior elements, the instrumentation is extended upward to the occiput or is extended downward to the C3, C4 fusion (Figure 4). Incomplete reduction of C1-C2 lesions is a significant risk factor for VA injury during the placement of screw instrumentation.16) In reducible lesions of the upper cervical spine, stabilization is critical to maintain neural decompression. For irreducible lesions, decompression is mandatory at the site of encroachment, whether an anterior or posterior approach is used. If complete reduction of the C1-C2 subluxation is possible, a C1-C2 fusion so that occipital-C1 motion is usually performedoccipital-C1 motion is preserved. If the lesion is irreducible with C1-C2 subluxation and C1 or C2 posterior element defects (such as fracture and tumors), OC fusion is recommended. However, irreducible C1-C2 lesions may necessitate OC fusion for stability.
In conclusion, although a small study sample was evaluated, the clinical outcomes show that the OC antlantoaxial transpedicular screw fixation was a safe and effective for the treatment of CVJ instability. Posterior atlantoaxial transpedicular screw/plate fixation was used to treat reducible atlantoaxial subluxation. The advantages of this procedure include, immediate rigid internal fixation and, early mobilization with the need for minimal external support.
Figures and Tables
FIGURE 1
Illustrations of the C1-C2 3D-reformatted scan. Posterior and lateral views demonstrating the C1 and C2 entry points for the atlantoaxial transpedicular screw fixation technique (white circle: entry point, arrow: pathway of screw).

FIGURE 2
A 54-year-old woman presented with quadriplegia due to motor vehicle accident. A: Preoperative sagittal CT scan shows occipitocervical dislocation (Power's ratio: 0.96). B: Preoperative lateral cervical spine radiograph shows atlantoaxial dislocation and 10 mm of anterior translation of C1. C: Postoperative lateral radiograph shows occipitocervical fusion with C1-C2 transpedicular screw fixation. D: Axial (C1) and sagittal view shows placement of pedicle screws. The screws were in the proper position and did not traverse the vertebral artery foramen.

FIGURE 3
A 55-year-old male patient had an unstable Jefferson fracture. There was vertebral artery injury during the C1 arch dissection. A: Axial CT scan shows fracture of the anterior and posterior arch of C1. B: Immediate angiographic evaluation shows evidence of left vertebral artery injury that was occluded by thrombus. C: Angiogram after coil embolization shows the totally embolized artery with no flow. D: We underwent unilateral screw placement only to avoid bilateral vertebral artery injury.
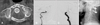
FIGURE 4
A 49-year-old male patient had a C2-C3 fracture dislocation with a quadriparesis due to a fall from the roof. A: Preoperative lateral cervical spine radiograph shows unstable C3 comminuted fracture with C2-C3 dislocation. B: Pre-operative axial and sagittal CT scan shows C2-C3 fracture dislocation with displacement of C2 posteriorly. C: Preoperative MRI scan shows enlargement of the upper spinal cord with intramedullary T2 high signal intensity, suggesting cord edema and contusion. D: C2-C3 fracture dislocation reduction was attempted with the Gardner-well tongs but failed. An extended fusion upward from C1 and downward to C4 was performed. The lateral radiograph showed C1 to C4 fusion and restoration of bone alignment postoperatively, the patient had a partial recovery with resolution of symptoms at the last follow up.

References
1. Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine (Phila Pa 1976). 1999; 24:1425–1434.

2. Apostolides PJ, Dickman CA, Golfinos JG, Papadopoulos SM, Sonntag VK. Threaded steinmann pin fusion of the craniovertebral junction. Spine (Phila Pa 1976). 1996; 21:1630–1637.

3. Deutsch H, Haid RW Jr, Rodts GE Jr, Mummaneni PV. Occipitocervical fixation: long-term results. Spine (Phila Pa 1976). 2005; 30:530–535.

4. Dickman CA, Crawford NR, Paramore CG. Biomechanical characteristics of C1-2 cable fixations. J Neurosurg. 1996; 85:316–322.

5. Dickman CA, Papadopoulos SM, Sonntag VK, Spetzler RF, Rekate HL, Drabier J. Traumatic occipitoatlantal dislocations. J Spinal Disord. 1993; 6:300–313.

6. Dickman CA, Sonntag VK. Posterior C1-C2 transarticular screw fixation for atlantoaxial arthrodesis. Neurosurgery. 1998; 43:275–280. discussion 280-281.

7. Fairholm D, Lee ST, Lui TN. Fractured odontoid: the management of delayed neurological symptoms. Neurosurgery. 1996; 38:38–43.

8. Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: a report of 160 treated patients. Neurosurgery. 2002; 51:1351–1356. discussion 1356-1357.

9. Grob D, Crisco JJ 3rd, Panjabi MM, Wang P, Dvorak J. Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine (Phila Pa 1976). 1992; 17:480–490.

10. Grob D, Dvorak J, Panjabi MM, Antinnes JA. The role of plate and screw fixation in occipitocervical fusion in rheumatoid arthritis. Spine (Phila Pa 1976). 1994; 19:2545–2551.

11. Grob D, Jeanneret B, Aebi M, Markwalder TM. Atlanto-axial fusion with transarticular screw fixation. J Bone Joint Surg Br. 1991; 73:972–976.

12. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976). 2001; 26:2467–2471.

13. Huckell CB, Buchowski JM, Richardson WJ, Williams D, Kostuik JP. Functional outcome of plate fusions for disorders of the occipitocervical junction. Clin Orthop Relat Res. 1999; (359):136–145.

14. Hurlbert RJ, Crawford NR, Choi WG, Dickman CA. A biomechanical evaluation of occipitocervical instrumentation: screw compared with wire fixation. J Neurosurg. 1999; 90:84–90.

15. Hue YH, Chun HJ, Yi HJ, Oh SH, Oh SJ, Ko Y. Unilateral posterior atlantoaxial transarticular screw fixation in patients with atlantoaxial instability: comparison with bilateral method. J Korean Neurosurg Soc. 2009; 45:164–168.
16. Madawi AA, Casey AT, Solanki GA, Tuite G, Veres R, Crockard HA. Radiological and anatomical evaluation of the atlantoaxial transarticular screw fixation technique. J Neurosurg. 1997; 86:961–968.

17. Marcotte P, Dickman CA, Sonntag VK, Karahalios DG, Drabier J. Posterior atlantoaxial facet screw fixation. J Neurosurg. 1993; 79:234–237.

18. Mitchell TC, Sadasivan KK, Ogden AL, Mayeux RH, Mukherjee DP, Albright JA. Biomechanical study of atlantoaxial arthrodesis: transarticular screw fixation versus modified Brooks posterior wiring. J Orthop Trauma. 1999; 13:483–489.

19. Miyakoshi N, Shimada Y, Suzuki T, Hongo M, Kasukawa Y, Okada K, et al. Factors related to long-term outcome after decompressive surgery for ossification of the ligamentum flavum of the thoracic spine. J Neurosurg. 2003; 99:251–256.

20. Nockels RP, Shaffrey CI, Kanter AS, Azeem S, York JE. Occipitocervical fusion with rigid internal fixation: long-term follow-up data in 69 patients. J Neurosurg Spine. 2007; 7:117–123.

21. Oda I, Abumi K, Sell LC, Haggerty CJ, Cunningham BW, McAfee PC. Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine (Phila Pa 1976). 1999; 24:2377–2382.

22. Paramore CG, Dickman CA, Sonntag VK. The anatomical suitability of the C1-2 complex for transarticular screw fixation. J Neurosurg. 1996; 85:221–224.

23. Sasso RC, Jeanneret B, Fischer K, Magerl F. Occipitocervical fusion with posterior plate and screw instrumentation. A long-term follow-up study. Spine (Phila Pa 1976). 1994; 19:2364–2368.

24. Singh SK, Rickards L, Apfelbaum RI, Hurbert RJ, Maiman D, Fehlings MG. Occipitocervical reconstruction with the Ohio Medical Instruments Loop: results of a multicenter evaluation in 30 cases. J Neurosurg. 2003; 98:239–246.

25. Smith MD, Anderson P, Grady MS. Occipitocervical arthrodesis using contoured plate fixation. An early report on a versatile fixation technique. Spine (Phila Pa 1976). 1993; 18:1984–1990.
26. Sonntag VK, Dickman CA. Craniocervical stabilization. Clin Neurosurg. 1993; 40:243–272.
27. Stevenson KL, Wetzel M, Pollack IF. Delayed intracranial migration of cervical sublaminar and interspinous wires and subsequent cerebellar abscess. Case report. J Neurosurg. 2002; 97:113–117.
28. Stokes JK, Villavicencio AT, Liu PC, Bray RS, Johnson JP. Posterior atlantoaxial stabilization: new alternative to C1-2 transarticular screws. Neurosurg Focus. 2002; 12:E6.

29. Sudo H, Abumi K, Ito M, Kotani Y, Minami A. Spinal cord compression by multistrand cables after solid posterior atlantoaxial fusion. Report of three cases. J Neurosurg. 2002; 97:359–361.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download