Abstract
Objective
In symptomatic patients with subdural hygroma, variety of treatment strategies, such as observation, repeated subdural tapping, external subdural drainage, and subduroperitoneal shunt (SPS) have been advocated. Until now, the ideal management for subdural hygromas in adults seems controversial, because of their differences between the effectiveness and the risk of complications. Thus, we evaluated the role of unvalved SPS for subdural hygromas in adults.
Methods
From January 2001 to December 2007, fifteen patients who had undergone unvalved SPS for symptomatic subdural hygromas in adults at our hospital were retrospectively reviewed. We analyzed the age, gender, initial diagnosis, causes, symptoms, neurological signs, and radiological findings such as thickness of subdural hygroma. Outcome was evaluated according to the post operative Glasgow Outcome Scale (GOS), radiologic findings and complications.
Results
The mean age of the patients is 61 years old (range from 29 to 86). We used the unvalved open-ended catheter to all patients. After SPS, all subdural hygromas disappeared on computed tomography scans within 14 days (mean 6.5 days) except 2 patients. Four patients had GOS 5. GOS 4 was present in three patients. GOS 3 was present in four patients. Three patients had GOS 2. One patient had GOS 1. Complications related to SPS occurred in 5 patients (33%)
Figures and Tables
FIGURE 1
Serial computed tomography (CT) images of patient number 12. A: Initial CT scan shows hydrocephalus due to cerebellar infarction. B: Bilateral subdural hygroma is noticed on CT image after suboccipital craniectomy. C: Post operative CT image of bilateral subduroperitoneal shunt reveals that subdural hygromas were resolved completely. Arrows indicate bilateral proximal shunt catheters.
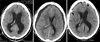
TABLE 1
Characteristics of 15 patients

no.: number, Dx: diagnosis, Sx: symptom, Tx: treatment, ICH: intracerebral hemorrhage, SDH: subdural hemorrhage, SAH: subarachnoid hemorrhage, IVH: intraventricular hemorrhage, Cbll: cerebellum, V-P shunt: ventriculoperitoneal shunt, EVD: external ventricular drainage, A-com: anterior communicating artery, P-com: posterior communicating artery, GBM: glioblastoma, RS: radiosurgery
References
1. Aoki N. Chronic subdural hematoma in infancy. Clinical analysis of 30 cases in the CT era. J Neurosurg. 1990; 73:201–205.
2. Caldarelli M, Di Rocco C, Romani R. Surgical treatment of chronic subdural hygromas in infants and children. Acta Neurochir (Wien). 2002; 144:581–588. discussion 588.

3. Cho JB, Cho KH, Kim SH, Shin YS, Lee W, Yoon SH. Surgical treatment of subdural hygromas in infants and children. J Korean Neurosurg Soc. 2005; 38:273–280.
4. Ersahin Y, Tabur E, Kocaman S, Mutluer S. Complications of subduroperitoneal shunting. Childs Nerv Syst. 2000; 16:433–436.
5. Erşahin Y. A new catheter for subduro-peritoneal shunting. Childs Nerv Syst. 2002; 18:518–521.
6. Hasegawa M, Yamashima T, Yamashita J, Suzuki M, Shimada S. Traumatic subdural hygroma: pathology and meningeal enhancement on magnetic resonance imaging. Neurosurgery. 1992; 31:580–585.
7. Kim BO, Kim SW, Lee SM. Effectiveness of early surgery in children with traumatic subdural hygroma. J Korean Neurosurg Soc. 2005; 37:432–435.
8. Korinth MC, Lippitz B, Mayfrank L, Gilsbach JM. Subdural-atrial and subdural-peritoneal shunting in infants with chronic subdural fluid collections. J Pediatr Surg. 2000; 35:1339–1343.

9. Lee KS, Bae WK, Bae HG, Yun IG. The fate of traumatic subdural hygroma in serial computed tomographic scans. J Korean Med Sci. 2000; 15:560–568.

10. Litofsky NS, Raffel C, McComb JG. Management of symptomatic chronic extra-axial fluid collections in pediatric patients. Neurosurgery. 1992; 31:445–450.

11. Meacham WF, McPherson WF. The diagnosis and treatment of subdural fluid collections in infants. Pediatr Clin North Am. 1970; 17:363–372.

12. Njiokiktjien CJ, Valk J, Ponssen H. Subdural hygroma: results of treatment by ventriculo-abdominal shunt. Childs Brain. 1980; 7:285–302.

13. Oka H, Motomochi M, Suzuki Y, Ando K. Subdural hygroma after head injury A review of 26 cases. Acta Neurochir (Wien). 1972; 26:265–273.
14. Schachenmayr W, Friede RL. The origin of subdural neomembranes. I. Fine structure of the dura-arachnoid interface in man. Am J Pathol. 1978; 92:53–68.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download