Abstract
Objective
The purpose of the study was to retrospectively compare the early and late tracheostomy in terms of ventilator days, intensive care unit (ICU) days, pneumonia, and clinical outcomes in patients with a severe traumatic brain injury (TBI) who underwent a decompressive craniectomy.
Methods
Patients who had a TBI and a Glasgow Coma Scale (GCS) score ≤8, and were treated with a unilateral or bilateral decompressive craniectomy were enrolled. Between January 2006 and December 2008, 37 patients were enrolled in the retrospective study. Percutaneous tracheostomies were performed by trained residents. According to the timing of the tracheostomy, the subjects were classified as the early (≤7 days; n=20) or late group (>7 days; n=17).
Results
The average time of the tracheostomy was 3.2±1.4 days in the early group and 9.7±0.9 days in the late group. There was no statistically significant difference between the early and late groups with respect to total days of mechanical ventilation, ICU stay, Glasgow Outcome Score (GOS), and pneumonia incidence. The duration of antibiotic administration for the treatment of pneumonia was shorter in the early group (p=0.04). Klebsiella species were the most common pathogens in both groups.
Tracheostomies are one of the most common procedures performed in the intensive care unit (ICU).8,16) Several benefits of tracheostomies in patients with severe head trauma include protection from further direct laryngeal injury, facilitation of nursing care (airway suctioning and mouth hygiene), and increased patient comfort.5) In 1989, the American Consensus Conference on Artificial Airways issued a statement that tracheostomy is preferred if the need for an artificial airway is anticipated to be greater than 21 days.15) The recovery time for a stuporous patient with a traumatic brain injury (TBI) is variable and difficult to predict. The most important aspect of the management of patients with a severe TBI is prevention of secondary insults from hypoxia and hypotension. Indeed, the majority of these patients ultimately require a tracheostomy, not only for ventilator support, but also for airway management. Many studies have been conducted to evaluate the benefits of early tracheostomy; however, the initial diagnosis and treatment milieu have been very heterogenous among the enrolled patients.2,3) The different treatments affect the clinical outcomes of patients with severe TBI. Therefore, we focus on the uniform surgical intervention, craniectomy which is widely performed and useful for the treatment of TBI.
The purpose of this study was to compare early (≤7 days) and late (>7 days) tracheostomy in terms of ventilator days, ICU stay, pneumonia, and clinical outcomes for patients with a severe TBI who underwent a decompressive craniectomy.
Patients were eligible for enrollment if they had a TBI and a Glasgow Coma Scale (GCS) score ≤8, and were treated with a unilateral or bilateral decompressive craniectomy. The indication for decompressive craniectomy with dural expansion was the appearance of definite unilateral or bilateral brain swelling on the computed tomography (CT), i.e., a midline shift of >6 mm and/or obliteration of the cisternal structures on the CT scan. Patients with primary fatal brainstem failure, a GCS score of 3 or 4 with no spontaneous respirations and bilateral pupil dilatation, did not undergo surgical intervention.
Between January 2006 and December 2008, 37 patients were enrolled in the retrospective study. Initially, patients were intubated oro-tracheally and ventilated mechanically, if necessary. If patients remained stuporous, they eventually underwent tracheostomy. Bedside percutaneous tracheostomies were performed by trained residents in our hospital. According to the timing of the tracheostomy, subjects were classified as an early group (≤7 days; n=20) or a late group (>7 days; n=17). At baseline, data on the demographic and clinical characteristics were obtained. We compared days of mechanical ventilation, ICU stay, Glasgow Outcome Score (GOS), pneumonia incidence, the pathogens of pneumonia, and duration of antibiotics administration for the treatment of pneumonia. Pneumonia was classified as recent pulmonary infiltration on chest radiography associated with at least 2 of the following signs: purulent tracheobronchial secretion, a body temperature >38.3℃, and leukocytes in the circulation >25% above the basal count.12,14) Work-up for the diagnosis of pneumonia was started from the transportation to ICU. First- or third-generation cephalosporins were perioperatively administered for prophylaxis of surgical infections. The functional outcome was evaluated using GOS, according to the World Federation of Neurological Surgeons (1=normal activity; 5=death).
Data are expressed as either the mean±standard deviation (SD), median, or percentage. An unpaired t-test was used to compare continuous variables, and the Fisher exact test was used to compare proportions. Statistical significance was achieved with a p value≤0.05.
Table 1 shows the demographic data of the enrolled patients. There was no significant difference between the groups in terms of gender, age, GCS score on admission, accompanying brain injuries (epidural hematomas and brain contusions), and lung injuries. The average time of the tracheostomy was 3.2±1.4 days in the early group and 9.7±0.9 days in the late group.
The clinical outcomes are summarized in Table 2. There was no statistically significant difference between the early and late groups regarding with respect to total days of mechanical ventilation, ICU stay, GOS, and pneumonia. The interval between the initiation and discontinuation of antibiotic administration for the treatment of pneumonia was shorter in the early group (16.6±4.6 vs. 20.8±3.3 days; p=0.04). Eighteen of 37 patients (48.6%) developed pneumonia during the peri- and post-tracheostomy periods. On suspicion and diagnosis of pneumonia, a sputum culture was performed. The antibiotic choice was determined on consultation with pulmonary specialists. When the clinical parameters, such as vital signs, breath sounds, and radiologic findings were not improved, even after a change in antibiotics, the sputum cultures were repeated, and antibiotic alterations were considered. The discontinuation of antibiotic administration was indicated when the body temperature had normalized for at least 3 days, pneumonic infiltration resolved on chest X-ray, and the leukocyte count and erythrocyte sedimentation rate/C-reactive protein (ESR/CRP) levels were normalized.
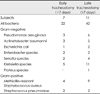
Table 3 shows the variety of bacteria which were associated with pneumonia. Twenty-two and 42 pathogens were isolated via sputum cultures in the early and late groups, respectively. Klebsiella species were the most common pathogens in both groups. The second and third most common pathogens were methicillin-resistant staphylococcus aureus and pseudomonas species.
The present study was conducted with retrospective reviews of clinical data, radiologic findings, and surgical records of a recent 3-year admission list of patients, and showed that early tracheostomy was associated with a shorter duration of antibiotic administration for the treatment of pneumonia in patients who underwent a decompressive craniectomy for a severe TBI.
Tracheostomies have been shown to be independently associated with a decreased risk for ventilator-associated pneumonia in non-trauma, immunocompetent patients.13) A meta-analysis of trauma patients demonstrated that early tracheostomies had no influence on mortality, pneumonia, or laryngotracheal pathology rates, and data from the review indicated that early tracheostomies should be strongly considered with severe brain injuries.6) Similarly, a prospective and randomized study showed that early tracheostomy did not reduce the number of days of mechanical ventilation, frequency of pneumonia or ICU length of stay in ventilator dependent trauma patients.3) According to single instituition reports, early tracheostomies decrease the total days of mechanical ventilation or mechanical ventilation time after development of pneumonia, and the length of ICU stay in patients with severe TBI.4) However, they did not describe the treatment modalities for TBI. We focus on patients underwent a homogenous surgical intervention, craniectomy in order to resolve inhomogenous population. TBI patients with a GCS score <8 is unlikely to be extubated. That is why we chose these conditions as inclusion criteria in our study.
Early tracheostomy allows for oral feedings, enhanced communication, early ambulation, and facilitates pulmonary toilet, which were associated with a shorter duration of antibiotic administration in our study. The patients were perioperatively administered first- or third-generation cephalosporins for prophylaxis of surgical infections. Most pneumonia pathogens are gram-negative or multidrug-resistant bacteria in our neurosurgical ICU. Therefore, the prophylactic use of cephalosporin did not reduce hospital-acquired pneumonias. A randomized study has demonstrated that antibiotic prophylaxis with ampicillin-sulbactam significantly reduced the occurrence of early-onset pneumonia in critically ill, comatose, mechanically-ventilated patients.1) Gram-positive bacteria, particularly staphylococcus aureus, were the predominant cause of pneumonia in the study. The efficacy of prophylatic antibiotic therapy for klebsiella species, pseudomonas species, and/or methicillin-resistant staphylococcus aureus is questionable in our setting.
There are a number of reasons to perform early tracheostomies in patients with severe TBIs. The most important reason may be to maintain the airway in stuporous patients. It is postulated that in severe TBI, the airway immune system becomes compromised, thereby increasing the potential for colonization and infection.7) Tracheostomy allows deeper suctioning of airway secretions. An early tracheostomy reduces the dead space ventilation and prevents laryngeal complications. Tracheostomy also decreases the work of breathing, airway resistance, and increases minute ventilation.10,11) Early tracheostomy did not affect the clinical outcomes, such as ventilator days, ICU days, and GOS in our study, but shortened the duration of pneumonia by facilitating respiratory toilet.
In patients with decreased intracranial compliance, a relatively minimally invasive procedure, such as percutaneous tracheostomy, may lead to a significant increase in intracranial pressure.9) During percutaneous tracheostomy, intracranial pressure should be closely monitored and preventive strategies should be instituted in an attempt to prevent secondary insults to an already severely injured brain. The early period (< 7 days after the injury) is vulnerable and critical to manage intracranial pressure. Therefore, early tracheostomy could be more harmful rather than late tracheostomy in terms of increased intracranial pressure.
There is a need for studies that address the practical guidelines for timing of tracheostomies according to the severity of the TBI and accompanying injuries.
An early tracheostomy decreased the duration of antibiotic use for the treatment of pneumonia in patients with severe TBI who underwent a decompressive craniectomy. An early tracheostomy did not reduce days of mechanical ventilation, length of ICU stay, the prevalence of pneumonia, and GOS.
Figures and Tables
References
1. Acquarolo A, Urli T, Perone G, Giannotti C, Candiani A, Latronico N. Antibiotic prophylaxis of early onset pneumonia in critically ill comatose patients. A randomized study. Intensive Care Med. 2005; 31:510–516.

2. Ahmed N, Kuo YH. Early versus late tracheostomy in patients with severe traumatic head injury. Surg Infect (Larchmt). 2007; 8:343–347.

3. Barquist ES, Amortegui J, Hallal A, Giannotti G, Whinney R, Alzamel H, et al. Tracheostomy in ventilator dependent trauma patients: a prospective, randomized intention-to-treat study. J Trauma. 2006; 60:91–97.

4. Bouderka MA, Fakhir B, Bouaggad A, Hmamouchi B, Hamoudi D, Harti A. Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma. 2004; 57:251–254.
5. Clum SR, Rumbak MJ. Mobilizing the patient in the intensive care unit: the role of early tracheostomy. Crit Care Clin. 2007; 23:71–79.
6. Dunham CM, Ransom KJ. Assessment of early tracheostomy in trauma patients: a systemic review and meta-analysis. Am Surg. 2007; 72:276–281.
7. Ewig S, Torres A, El-Ebiary M, Fábregas N, Hernández C, González J, et al. Bacterial colonization patterns in mechanically ventilated patients with traumatic and medical head injury. Incidence, risk factors, and association with ventilator-associated pneumonia. Am J Respir Crit Care Med. 1999; 159:188–198.
8. Kim SH, Kim Y. A clinical study about the effect of tracheostomy in the brain damaged patients. J Korean Neurosurg Soc. 1985; 14:175–182.
9. Kocaeli H, Korfali E, Taşkapilioğlu O, Ozcan T. Analysis of intracranial pressure changes during early versus late percutaneous tracheostomy in a neuro-intensive care unit. Acta Neurochir (Wien). 2008; 105:1263–1267.

10. Lin MC, Huang CC, Yang CT, Tsai YH, Tsao TC. Pulmonary mechanics in patients with prolonged mechanical ventilation requiring tracheostomy. Anaesth Intensive Care. 1999; 27:581–585.

11. Moscovici da Cruz V, Demarzo SE, Sobrinho JB, Amato MB, Kowalski LP, Deheinzelin D. Effects of tracheotomy on respiratory mechanics in spontaneously breathing patients. Eur Respir J. 2002; 20:112–117.

12. Murphy TF, Sethi S. Bacterial infection in chronic obstructive pulmonary disease. Am Rev Respir Dis. 1992; 146:1067–1083.

13. Nseir S, Di Pompeo C, Jozefowicz E, Cavestri B, Brisson H, Nyunga M, et al. Relationship between tracheotomy and ventilatorassociated pneumonia: a case-control study. Eur Respir J. 2007; 30:314–320.
14. Pereira ED, Fernandes AL, da Silva Anção M, de Araúja Pereres C, Atallah AN, Faresin SM. Prospective assessment of the risk of postoperative pulmonary complications in patients submitted to upper abdominal surgery. Sao Paulo Med J. 1999; 117:151–160.

15. Plummer AL, Gracey DR. Consensus conference on artificial airways in pateints receiving mechanical ventilation. Chest. 1989; 96:178–180.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download