Abstract
Objective
The purpose of this study was to evaluate the risk factors for the development of progressive intracranial hemorrhage (PIH) after acute head injury.
Methods
175 (one hundred and seventy-five) head trauma patients who visited our hospital and had computerized tomography (CT) scan from January 2005 to December 2006 were investigated. Their medical records, radiological images and readings were analyzed retrospectively.
Results
Of the total 175 patients, 64 (64/175=36.6%) presented PIH. PIH was found in 54 patients (48.6%) of the 111 patient who obtained CT scans within 3 hours after trauma, whereas it was found in 10 (15.7%) of 64 patients who obtained CT more than 3 hours after head trauma. In 64 patients having PIH, the mean time interval between first and second CT scans was 13.8 hours. The risk factors for the development of PIH were cause of trauma, hemorrhagic lesion type, initial Glasow Coma Scale, first CT scan time after trauma.
Conclusion
If initial CT scan taken early after trauma shows hemorrhage, continuous supervision of mental status and changes in intracranial pressure, and early follow-up CT scan within 5 to 6 hours is necessary. In addition, because progression of hemorrhage may continue in a patient with hyperacute intracranial hemorrhage who are preparing for surgery, it is recommended to have a CT scan again right before the operation.
In the past, it took a long time for head-injured patients to arrive at the emergency center due to transporting system. It was not clear whether intracranial hemorrhage was present from the start or occurred later or in progress. In 1891, Bollinger reported the first delayed intracranial hemorrhage patient as "traumatische Spat-Apoplexie"(delayed apoplexy).7) According to the diagnostic criteria in 1891, delayed intracranial hemorrhage was defined as 1) clear history of head injury, 2) asymptomatic period of a few days or a few weeks (2-4 weeks), 3) acute onset of symptom, 4) no cerebrovascular diseases.7,12)
Incidence of delayed intracranial hemorrhage is reported as 23-47.5%1,2,14,18) Though, along with the development of diagnostic tools such as brain CT, it is defined as both the acute onset of symptom after a certain duration of asymptomatic period and progressive hemorrhage revealed after 24-48 hours posttraumatic.7,11) In other words, delayed intracranial hemorrhage means spontaneously developed recurrent hemorrhage in the injured tissue after a certain period that posttraumatic hemorrhage is controlled. With the development of emergency transport system, head-injured patients are usually transferred to the emergency room (ER) quickly and go through neurological examination and brain CT within 1 hour after trauma.10,17) It is common these patients experience aggravation of mental status and increase of intracranial hemorrhage.
Progressive intracranial hemorrhage (PIH) which is continuous hemorrhage after trauma should be distinguished from delayed intracranial hemorrhage.16) PIH was diagnosed for patients with the increase of hematoma found on the initial brain CT within 24 hours postinjury. Increase of hematoma includes hemorrhage with both acute and subacute onset. In the cases where the second CT was taken place, PIH was defined as more than 25% of increase in hemorrhage within 24 hours after the first CT scan.12) In this study, the patients with head injury were retrospectively analyzed based on medical history and radiologic data to determine the risk factors of PIH. This study is performed to predict PIH in advance and to suggest appropriate management.
Of 263 head injury patients, 175 who had CT scan more than twice in our hospital from 2005 to 2007 were subject of this study, who had found to have intracranial hemorrhage on initial CT scan. The management for intracranial hemorrhage is divided into two groups; emergent surgery and conservative management. Emergent surgery was performed if intracranial hemorrhage was detected on brain CT and mass efT ct was present. If the condition of a patient and the amount of hemorrhage did not rethere surgery based on clinical judgment, the patient'sient and the astatus was observed closely with ftivow-up CT and conservatively managed in the intensive care unit (ICU). Intracranial pressure monitoring was not included in treatment plan, so it was only done in a few patients.
Intracranial hemorrhage was categorized into epidural hemorrhage (EDH), subdural hemorrhage (SDH), intracerebral hemorrhage (ICH), subarachnoid hemorrhage (SAH) based on brain CT. ICH or SAH associated with brain contusion is classified as intraparenchymal contusion or hematoma (IPCH). PIH was defined as more than 25% of increase of hematoma on the second CT taken within 24 hours after the first CT which showed intracranial hemorrhage. The cases with surgery for intracranial hematoma were excluded in spite of the increase of hematoma postoperatively. The increase of hematoma was determined by a radiologist and a neurosurgeon.
Of 175 patients, the group of 64 with PIH and the group of 111 without PIH were compared. Based on the medical record and brain CT, general medical condition, trauma, and factors associated with evaluation and outcome were investigated. General condition is specified into sex, age, past medical history, coagulation status such as history of antiplatelet agent use and the number of platelet.
The trauma-related factors were the cause of trauma, the type of hematoma, the initial Glasgow Coma Scale (GCS) score, and the Glasgow Outcome Scale (GOS) at discharge, the time from trauma to the first brain CT, and the time interval between the first and the second CT.
A variate logistic analysis was used to determine the predictors of PIH. Predictors were defined as being significant if p value is lower than 0.05. Chi-square statistics were calculated for categorical comparisons. Values for the continuous parameters are given as the mean±SD.
The patient was a 68-year-old female who had an altered mentality when brought to the ER due to traffic accident as a pedestrian 40 minutes ago. She was stuporous with GCS score of 8. The initial CT scans obtained 30 minutes postinjury showed subdural hematoma and brain contusion on the left frontal lobe (Figure 1A, B). Her mentality aggravated in the ICU and had the second CT scan, 2 hours after the first scan. On the second CT, subdural hematoma in the left frontal lobe and intraventricular hemorrhage significantly increased (Figure 1C, D). She underwent emergency craniectomy and hematoma removal. However, her mental status did not improve due to brain edema and multiple hemorrhages, and GOS at discharge was 3.
46-year-old male was transported to emergency department after fall-down in drunken state. His mentality was drowsy, which was difficult to distinguish from drunken condition. A small amount of epidural hematoma with skull fracture in the right temporal area was demonstrated on the initial CT one hour postinjury (Figure 2A, B). The second CT scans were obtained 6 hours after the first CT since his mentality kept being drowsy. The amount of epidural hematoma was noticeably increased on CT (Figure 2C, D). The patient discharged without any neurological deficit after emergency hematoma removal.
54-year-old male was presented to the ER complaining of severe headache after a traffic accident 1 day ago. His mental status at the time of presentation was alert, and neurologically normal. SDH on the left frontal convexity area and EDH on the right temporal area were detected on brain CT taken 1 day after injury (Figure 3A, B). After conservative management, the hematoma was not increased on follow-up CT taken 2 days postinjury (Figure 3C, D).
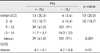
Out of 263 patients with intracranial hemorrhage after head trauma, 175 patients had CT scans more than twice. The incidence of PIH was 36.6% (64/175). The mean age of total 175 patients was 51.2 years while the mean age of patients with PIH was 48.6±21.5, and the mean age of patients without PIH was 52.6±19.9. The mean age is lower in the group with PIH, but it was not statistically significant (p=0.207)(Table 1). PIH was found in 40 males and 24 females, revealing higher incidence in males. However, considering that intracranial hemorrhage occurred more in males (118 males, 57 females), the gender and the occurrence of PIH are not associated with p-value of 0.291.
Comparing to no history of diseases, the presence of past medical history such as hypertension and diabetes showed no significance. The use of antiplatelet agents involved aspirin, warfarin and clopidol, and it was not significant with p-value of 0.421. The factors related to blood coagulation on blood laboratory at admission did not prove correlation with PIH. When the causes of injury were taken into consideration, PIH happened more with traffic accident and fall-down which are comparably severe trauma (Table 2).
Regarding the types of hematoma, the highest rate of PIH was occurred in patients with IPCH. Both the presence and the adjacency of fracture showed no relationship with PIH. The amount of hematoma was higher in patients with PIH, but it was not statistically significant. Initial GCS showed the significant relation with the incidence of PIH (Table 3), and when it is divided into severe (GCS 3-8), moderate (GCS 9-12), and mild (GCS 13-15), the lower the GCS score, the more likely it was that PIH was present (p<0.001). GOS was lower in patients with PIH showing poor prognosis (p<0.02).
The association between the incidence of PIH and the time from head injury to brain CT scans was analyzed. Among the 111 patient whose CT scans were taken within 3 hours after trauma, 54 patients (48.6%) presented PIH. But, PIH was found in 10 patients (15.7%) out of 64 patients who had CT scan more than 3 hours after head trauma. PIH occurred more when the time interval between trauma and CT scan was shorter (Table 4).
In this study, PIH is distinguished from delayed intracranial hemorrhage defined in previous studies.1,2,7,11,14,18) PIH was defined as the aggravation of mental status due to the rapid progression of intracranial hemorrhage found on the initial CT.1,3) The risk factors of PIH figured out on this study were the first brain CT scanning time detecting intracranial hemorrhage, the cause of trauma, the GCS score at admission, and the type of lesion. The higher incidence of PIH was statistically significant in the cases that had brain CT scan within 3 hours after trauma, and fall-down or traffic accident for the cause of injury, lower initial GCS, and presence of IPCH.
The incidence of PIH is reported as 23-48%, and it was 36.6% in this study.1,2,14,18) However, it is expected to be higher since there were cases which surgery had been performed right after the initial brain CT. It is also because the initial brain CT scan was delayed, so the large amount of intracranial hematoma was detected on the first brain CT scans. In addition, if brain CT had been performed more frequently in order, delayed intracranial hemorrhage would be included in PIH. PIH is reported higher in the old age, due to low contractility of blood vessels and free space in skull.8,13,14) The result from this study showed no statistical significance of the age. It is regarded as because of a small sample size. Regarding sex of patients, males tend to be more active and to work where heavier load is required so that they are more exposed to trauma. The absolute number of occurrence of PIH was significantly higher in males but it was not relative statistically considering the incidence of trauma.
The higher incidence of PIH was expected in hypertensive patients as they use more antiplatelet agents.4-6,9) The result was inadequate since the history of medication was not clear or the record was insufficient. Platelet count dropped and prolonged coagulation time in severe multiple injury showed the association with PIH, but statistic significance was not observed. It is considered as a result of small number of cases with abnormalities on laboratory data. It was verified that PIH has a higher incidence rate in trauma such as traffic accident and fall-down that is likely to be associated with shearing injury.
Traffic accident was highest both in absolute number and in relative number. The type of lesion was also related to the occurrence of PIH. Trauma with IPCH would be more severe than the cases only with EDH and SDH and also injury involving brain parenchyma would cause more PIH. The presence and adjacency of fracture both showed no association with PIH. The amount (thickness) of hematoma was also found to be an inappropriate predictor of PIH. This is considered that the presence of fracture and the amount of hematoma are not proportionate to the degree of injury. The initial GCS at admission can be a predictor of PIH and the GCS score tends to be lower in cases with PIH than the one without PIH. It means that the initial GCS score refers to the condition of patients and the effect of trauma to patients.
The shorter the initial brain CT scanning time, the more PIH occurred. It demonstrates that intracranial hemorrhage within a few hours after injury is still in progress.3,16,19) It is suggested that intracranial hemorrhage on brain CT taken right after injury is not a result but a progress. Thus, the shorter the initial brain CT scanning time, it should be considered that it only shows the early stage of hemorrhage and the additional hemorrhage is possible. However, if it took a long time to take initial brain CT, it can be assumed that the rate of hemorrhage is decreased or hemostasis is in progress so that PIH was not likely to occur. The time interval between the first and the second brain CT tends to be shorter in the cases with PIH, but it was not statistically significant. The follow-up CT was taken at variable points in patients with small amount of intracranial hemorrhage and in stable patients who showed no change on observation. It had no significant value since the standard deviation was substantial.
On the contrary, it is reasonable that the td the t caal b oween the first and the follow-up brain CT was shorter in patients with PIH since they were generally unstable. As shown in the Table 4, the mean time interval between the first and follow-up CT for PIH (+) group was 13.8 hours, and it was almost taken within 6 hours (Figure 4).
Prediction of changes in intracranial pressure such as PIH in intracranial hemorrhage after trauma or brain edema is possible with a close examination of neurological status and ICP monitoring installed in skull.15) The relationship between the incidence of PIH and ICP change was not analyzed in this study. It was because that ICP monitoring was not available and the condition of patients was stable. It was often that PIH occurred when waiting to be admitted. In addition, ICP changes do not have to be considered when figuring out predictors of PIH.
The limitation of this study is that the borderline between PIH and delayed intracranial hemorrhage can be unclear. The brain CT had not been performed in order for the subjects in this study. PIH was only diagnosed for progression of hemorrhage within 24 hours so that the cases with slow progression rate and no follow-up CT taken within 24 hours were excluded and probably caused an error. The emergency treatment such as blood or component transfusion for multiple organ failure and mannitolization for lowering ICP can possibly be a factor related to PIH.
In our study, the incidence of PIH after acute head injury was high (36.6%). It happens more in the cases with low GCS at presentation, IPCH, and when brain CT was taken within 3 hours after injury. Especially, PIH was found in 48.6% of patient who obtained CT scan within 3 hours of injury.
Intracranial hemorrhage on initial brain CT scans taken right after the injury should not be regarded as a completed result, but a progressive state. Therefore, we recommend a repeated CT scan is required within at least 6 hours even when the condition of patients does not change. But in the cases with low GCS at presentation, IPCH, and when CT scan was taken within 3 hours of injury, a repeated CT scan should be performed within 2-3 hrs.
Figures and Tables
 | FIGURE 1Illustration of Case 1, progression of intracranial hemorrhage in 2 hours. A, B: Initial CT scans obtained 30 minutes postinjury, demonstrating multiple small contusion and small amount of subdural hematoma in the left frontotemporal area. C, D: Second CT scans obtained 2 hours postinjury, revealing hemorrhagic progression. |
 | FIGURE 2Illustration of Case 2, progression of EDH in 5 hours. A, B: Initial CT scans obtained 1 hour postinjury, demonstrating minimal EDH in right temporal lobe. C, D: Second CT scans obtained 6 hours postinjury, revealing large amount of EDH. EDH: epidural hemorrhage. |
 | FIGURE 3Case 3, non progreiion of subdural hemorrhage. A, B: Initial CT scans obtained about 1 day postinjury, demonstrating SDH in the left frontal convexity and multiple contusions. C, D: Second CT scans obtained about 2 days postinjury, revealing no increment of hematoma. SDH: subdural hemorrhage. |
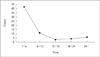 | FIGURE 4Time interval between first and second CT in 64 cases with progressive intracranial hemorrhage. |
References
1. Baratham G, Dennyson WG. Delayed traumatic intracerebral hemorrhage. J Neurol Neurosurg Psychiatry. 1972; 35:698–706.
2. Becker DP, Miller JD, Ward JD, Greenberg RP, Young HF, Sakalas R. The outcome from severe head injury with early diagnosis and intensive management. J Neurosurg. 1977; 47:491–502.

3. Brown CV, Weng J, Oh D, Salim A, Kasotakis G, Demetriades D, et al. Does routine serial computed tomography of the head influence management of traumatic brain injury? A prospective evaluation. J Trauma. 2004; 57:939–943.

4. Chang EF, Meeker M, Holland MC. Acute traumatic intraparenchymal hemorrhage: risk factors for progression in the early post-injury period. Neurosurgery. 2006; 58:647–656.

5. Clark JA, Finelli RE, Netsky MG. Disseminated intravascular coagulation following cranial trauma. Case report. J Neurosurg. 1980; 52:266–269.
6. Crone KR, Lee KS, Kelly DL Jr. Correlation of admission fibrin degradation products with outcome and respiratory failure in patients with severe head injury. Neurosurgery. 1987; 21:532–536.

7. Elsner H, Rigamonti D, Corradino G, Schlegel R Jr, Joslyn J. Delayed traumatic intracerebral hematomas: "Spät-Apoplexie". Report of two cases. J Neurosurg. 1990; 72:813–815.
8. Gudeman SK, Kishore PR, Miller JD, Girevendulis AK, Lipper MH, Becker DP. The genesis and significance of delayed traumatic intracerebral hematoma. Neurosurgery. 1979; 5:309–313.

9. Kaufman HH, Moake JL, Olson JD, Miner ME, duCret RP, Pruessner JL, et al. Delayed and recurrent intracranial hematomas related to disseminated intravascular clotting and fibrinolysis in head injury. Neurosurgery. 1980; 7:445–449.

10. Klauber MR, Marshall LF, Toole BM, Knowlton SL, Bowers SA. Cause of decline in head-injury mortality rate in San Diego County, California. J Neurosurg. 1985; 62:528–531.

11. Ninchoji T, Uemura K, Shimoyama I, Hinokuma K, Bun T, Nakajima S. Traumatic intracerebral haematomas of delayed onset. Acta Neurochir (Wien). 1984; 71:69–90.

12. Oertel M, Kelly DF, McArthur D, Boscardin WJ, Glenn TC, Lee JH, et al. predictors and consequences of the evolving injury. J Neurosurg. 2002; 96:109–116.
13. Rathlev NK, Medzon R, Lowery D, Pollack C, Bracken M, Barest G, et al. Intracranial pathology in elders with blunt head trauma. Acad Emerg Med. 2006; 13:302–307.

14. Rim BC, Kim ED, Min KS, Lee MS, Kim DH. A clinical analysis of delayed traumatic intracerebral hemorrhage. J Korean Neurosurg Soc. 1998; 27:1490–1499.
15. Servadei F, Nanni A, Nasi MT, Zappi D, Vergoni G, Giuliani G, et al. Evolving brain lesions in the first 12 hours after head injury: analysis of 37 comatose patients. Neurosurgery. 1995; 37:899–906.
16. Servadei F, Nasi MT, Giuliani G, Cremonini AM, Cenni P, Zappi D, et al. CT prognostic factors in acute subdural haematomas: the value of the 'worst' CT scan. Br J Neurosurg. 2000; 14:110–116.
17. Shackford SR, Mackersie RC, Hoyt DB, Baxt WG, Eastman AB, Hammill FN, et al. Impact of a trauma system on outcome of severely injured patients. Arch Surg. 1987; 122:523–527.

18. Stein SC, Spettell C, Young G, Ross SE. Delayed and progressive brain injury in closed-head trauma: radiological demonstration. Neurosurgery. 1993; 32:25–30.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download