Abstract
Tension pneumocephalus is an unusual delayed presentation of trauma. This case is presentation of a young man who suffered sudden deterioration of mental status from the rupture of the preexisting pneumocyst. He had a history of basal skull fracture, had a ventriculoperitoneal shunt placed due to posttraumatic hydrocephalus and had also undergone the repairing operation of basal skull defect at another hospital. The successful treatment of tension pneumocephalus and persistent pneumocyst at our hospital is described. The neurosurgeon must be aware the possibility of delayed pneumocyst formation and tension pneumocephalus in patients who experienced basal skull fracture quite a long time ago.
Tension pneumocephalus is a serious condition requiring prompt treatment.1) It is usually occurred after trauma and associated with basal skull fracture. Some cases were reported after neurosurgical manipulation.3,4,6,8,9) We describe a case of delayed tension pneumocephalus that presumably developed from rupture of the incompletely treated pneumocyst of the right anterior cranial fossa.
This 35-year-old man visited outpatient clinic of our hospital complaining headache, insomnia and memory disturbance. His medical record showed that he had a diffuse axonal injury by traffic accident 15 years ago and was treated at another hospital. A ventriculoperitoneal (VP) shunt was placed at that time due to hydrocephalus. The patient said that the second operation was performed due to a right frontal pneumocyst at the same hospital three years later. The initial study and follow up data were not obtainable and we were not certain whether the pneumocyst was completely treated or not. On the initial computed tomography (CT) scan at our hospital, a round pneumocyst was found on the right anterior cranial fossa (Figure 1). He refused further study and operation for removal of pneumocyst and repair of the defect. Conservative treatment including headache regimen was done and the patient was followed up for two years. He had no history of cerebrospinal fluid (CSF) leakage. On the day of emergent admission, the patient's mother reported that he had complained severe headache for two hours before deterioration. There was no known recent head trauma history and signs of CSF infection.
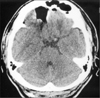
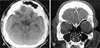
On the neurological examination, the patient was stuporous and hemiplegic on the left side. Axial CT scans revealed frontotemporal air collection with multiple cisternal air densities and compression of the parenchyma of brain bilaterally. The characteristic separation of the frontal lobe instead of peaking sign only was consistent with the diagnosis of tension pneumocephalus.7) The size of the previous air pocket seemed slightly decreased than the previous CT image (Figure 2).
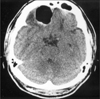
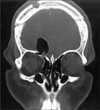
In consideration of the rapid deterioration, a twist drill trephination instead of a craniotomy with repair of the defect was performed on the right frontal bone and an externalized drain was connected to the closed drainage system. Two days later, the patient improved markedly. The CT scan checked on the fourth postoperative day showed complete resolution of the tension pneumocephalus, but the pneumocyst persisted without change of size compared to the CT checked on the day of his admission (Figure 3). Two weeks after his operation, a CT scan was rechecked. On the coronal section, pneumocyst was found to be connected to the fractured ethmoid sinus (Figure 4). The second operation was performed to repair the fractured sinus and dura. After right frontal craniotomy, the opening of ethmoid sinus was repaired with fascia lata graft and fibrin glue. A small dural laceration was sutured. The patient discharged ten days after second operation without neurological deficit and CSF leakage. A CT scan checked at four months after the second operation revealed complete disappearance of pneumocyst and good covering of fascial graft over the fractured ethmoid sinus (Figure 5).
The occurrence of pneumocephalus is relatively common in neurosurgical field but the air disappeared within several weeks. Tension pneumocephalus is rare in the neurosurgical practice and may produce mass effect, related neurological symptoms and signs and potentially life threatening sometimes. There are two generally accepted pathophysiological mechanisms for the formation of tension pneumocephalus after head trauma: a 'ball-valve' mechanism and an 'inverted soda-pop bottle' mechanism.1,4,5,7) Usually, tension pneumocephalus has been reported in association with traumatic brain injury and cranial trauma. It has been also occurred after the paranasal sinus operation, decompression of subdural hematoma, posterior fossa operation in the sitting position and the transsphenoidal surgery.3,4,7) Usually, tension pneumocephalus developed on the acute stage but there are a few of anecdotal reports of delayed occurrence. Some rarer causes and related conditions of pneumocephalus including tension pneumocephalus were reported: congenital defect of tegmen tympani, hyperpneumatization of cranium, VP shunt surgery, intravenous catheterization and rupture of an acquired nontraumatic middle fossa encephalocele.2,3,6,9,10)
The patient described in our article had pneumocyst which developed due to the basal skull fracture and spontaneous rupture of the pneumocyst might cause the delayed tension pneumocephalus 17 years after injury. The authors postulate that the patient tolerated the space occupying lesion well due to the encephalomalatic change of the frontal lobe and the patient's VP shunt might be involved in the rupture of the pneumocyst because of its contribution to the intracranial pressure.
Due to the lack of data, we are not sure of the type of the shunt and the presence of the antisiphon device. There has been controversy about the role of antisiphon device in relation to the development of tension pneumocephalus. Some authors asserted that modification of shunt system to a higher pressure valve or addition of antisiphon device may lead to successful treatment but others reported that regardless of the antisiphon use, they experienced development of the tension pneumocephalus.8) Previous reports have shown that tension pneumocephalus after shunt surgery occurred with several weeks or months.6,9) We assumed that the shunt might prevented CSF leakage and was the sine qua non for tension pneumocephalus, but the presence of shunt might not be the main cause of acute development of tension pneumocephalus in consideration of very long asymptomatic period. So, we postulated that a sterile and well functioning shunt management was unnecessary and mainly aimed at direct surgical closure of the fistulous site.
The treatments consist of the administration of high inspired concentrations of oxygen in case of nitrous oxide anesthesia, conservative treatment, needle aspiration, burr hole trephination with continuous external drainage, or craniotomy with defect repair.1,3) Recently endoscopic treatment has been used.3,4,6)
The neurosurgeon have to remind themselves the possibility of delayed pneumocyst formation and tension pneumocephalus in patients who experienced basal skull fracture quite a long time ago.
Figures and Tables
FIGURE 2
CT scans at emergent admission. Bilateral frontotemporal air collection and multiple air densities on the of the subdural space compressing brain parenchyma (A). The size of air pocket showing smaller than initial state (B).
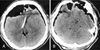
FIGURE 3
A CT scan of the postoperative day 4 (1st operation) showing remained pneumocyst without change of size.
References
1. Arbit E, Shah J, Bedford R, Carlon G. Tension pneumocephalus: treatment with controlled decompression via a closed water-seal drainage system. Case report. J Neurosurg. 1991; 74:139–142.
2. Cartwright MJ, Eisenberg MB. Tension pneumocephalus associated with rupture of a middle fossa encephalocele. Case report. J Neurosurg. 1992; 76:292–295.
3. Iplikcioglu AC, Bek S, Bikmaz K, Basocak K. Tension pneumocyst after transsphenoidal surgery for rathke's cleft cyst: case report. Neurosurgery. 2003; 52:960–962.

4. Cho HL, Han YM, Hong YK. Tension pneumocephalus after transsphenoidal surgery: report of two cases. J Korean Neurosurg Soc. 2004; 35:536–538.
5. Lunsford LD, Maroon JC, Sheptak PE, Albin MS. Subdural tension pneumocephalus. Report of two cases. J Neurosurg. 1979; 50:525–527.
6. McClay JE, Carreno O, Gupta A, Willner A. Treatment of Postcraniotomy Tension Pneumocephalus via Endoscopic Closure of the Nasofrontal Recess. Skull Base Surg. 1998; 8:221–224.

8. Sasani M, Ozer FA, Oktenoglu T, Tokatli I, Sarioglu AC. Delayed and isolated intraventricular tension pneumocephalus after shunting for normal pressure hydrocephalus. Neurol India. 2007; 55:81–82.

9. Satapathy GC, Dash HH. Tension pneumocephalus after neurosurgery in the supine position. Br J Anaesth. 2000; 84:115–117.

10. Thompson TP, Levy E, Kanal E, Lunsford LD. Iatrogenic pneumocephalus secondary to intravenous catheterization. Case report. J Neurosurg. 1999; 91:878–880.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download