Abstract
Objective
In the elderly, chronic subdural hematoma (CSDH) has impairment of cognitive function such as memory and language. But these rather nonspecific symptoms may lead to misdiagnosis such as dementia and false treatment. The aim of this retrospective study was the identification of the leading clinical symptoms in patient with the diagnosis CSDH who had been treated surgically.
Methods
79 patients with symptomatic CSDH (47 male, 32 female; mean age 69.0±10.4) who were admitted to our neurosurgical department from 2005 to 2007, were included in the study. We reviewed the medical records including clinical status, radiologic finding, history of trauma and postoperative recurrence of subdural hematoma. The instrument used for assessing cognitive functions was the Korean Mini-Mental State Examination (K-MMSE).
Results
The preoperative symptoms were cognitive impairments in 43 patients (54.4%), followed by headache in 34 patients (43.0%), hemiparesis in 31 patients (39.2%) and dysarthria in 15 patients (20.3%). Simple burr hole trephination and hematoma evacuation were done in all patients. We found that all preoperative symptoms were improved.
Conclusion
CSDH is an important differential diagnosis for dementia and neurodegenerative diseases, and an important reversible cause of dementia in elderly. If dementia is suspected, we should check early neuroimaging evaluation that may allow for timely treatment of this condition to avoid a poor outcome.
With recent increases in the number of aging members of the population, the diagnosis and treatment of dementia have become an important social issue. Dementia is a clinical syndrome characterized by acquired loss of cognitive and emotional abilities, which is severe enough to interfere with daily functioning and quality of life.12) It occurs primarily in the elderly. The prevalence is approximately 1% in persons 60 years of age and doubles with every 5-year increase in age.5)
In geriatric psychiatry and neurology, patients often present rather nonspecific symptoms such as psychomotor regression, cognitive impairment and amnesia. Those signs mostly indicate a diagnosis of dementia or, when combined with tremor or motor deficits, are probably interpreted as the signs of beginning neurodegenerative diseases such as Parkinson disease and Alzheimer disease. Once such a diagnosis is considered, these patients are treated medically without neuroradiological imaging. In neurosurgical department, three operable causes for dementia are recognised: normal pressure hydrocephalus, frontobasal located meningiomas and chronic subdural hematoma (CSDH). Radiologic study is needed to detect these kinds of operable lesions.
CSDH represents one of the most frequent types of intracranial hematoma with a favorable prognosis when treated adequately. The reported annual incidence of CSDH is approximately 0.001-0.002%.23) A steady increase in the incidence has been observed in developing countries due to the rise in life expectancy, the incidence reaching 0.0074% in the over 70s age group. CSDH is mostly caused by a head trauma- a minor trauma in many cases-which may even not be recognised at the time of occurrence, and often dates back many weeks or even months before symptomatic presentation.
The aim of this retrospective study was to identify leading clinical symptoms in patient with the diagnosis CSDH who had been treated surgically and to analyze potential risk factors associated with cognitive impairment and clinical factors related to the recurrence of CSDH.
Retrospectively reviewed were the clinical and radiological records of 79 consecutive cases with CSDH which underwent surgical treatment at our hospital from January 2005 to December 2007. The lesions were diagnosed by computed tomography (CT) and magnetic resonance imaging (MRI) in every patient. Simple burr hole trephination and hematoma evacuation with closed drainage were done in all patients. Burr hole was usually made on parietal eminence or dependent portion of hematoma. Subdural drain catheter was inserted into cavity of CSDH with minimal intraoperative drainage of CSDH to avoid air accumulation in subdural space. Subdural drain catheter had kept for 1 to 7 days after operation (mean duration was 3.1 days). The medical records were reviewed for gender and age; the thickness and side of CSDH; pre- and postoperative clinical status including cognitive impairment (including confusion), headache, dysarthria, hemiparesis, psychosyndrome (aggressive or inadequate behaviour) and seizures. We measured the cognitive status using the Korean Mini-Mental State Examination (K-MMSE) on admission and discharge.8) Cognitive impairment was confirmed when the recorded K-MMSE score was less than 23 points.
Statistical analysis was performed with chi-square test and the t-test to assess the relationship between each factor and cognitive impairment, and recurrence of CSDH. For all analyses, a p-value of <0.05 was considered statistically significant.
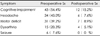
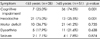
There were 47 men (59.5%) and 32 women (40.5%), Mean age (69.0±10.4). Preoperative clinical symptoms and neurological deficits consisted of cognitive impairment in 43 patients (54.4%) as the leading clinical symptom, headache in 34 patients (43.0%), motor deficits (monoparesis or hemiparesis) in 31 patients (39.2%) and dysarthria in 16 patients (20.3%)(Table 1). The incidence of preoperative cognitive impairment was 25.0% below 65 years and 74.5% above 65 years. There was statistical significance between age and preoperative cognitive impairment (p<0.05)(Table 2). We found that the older patients were, the more frequently cognitive impairment occured. We found that the correlation between CT finding (the thickness of hematoma and side of hematoma) and the preoperative cognitive impairment was not significant.
Postoperative result showed preoperative symptoms were improved respectively {cognitive impairment in 12 patients (15.2%), motor deficit in 7 patients (8.9%), headache in 6 patients (7.6%) and dysarthria in 4 patients (5.1%)}(Table 1).
Age and preoperative K-MMSE score had statistical significance as the factor affecting recovery of cognitive impairment after an operation. The study showed that mean age was 68.4 in the improved group and 78.6 in the unimproved group (p<0.05)(Table 3). Preoperative mean K-MMSE score was 16.4 in the improved group and 5.8 in the unimproved group (p<0.05)(Table 3). But we also found that the correlation between CT finding (the thickness of hematoma and side of hematoma) and recovery of cognitive impairment was not significant.
Finally, the recurrence of subdural hematoma didn't have any correlation with age, the thickness of hematomas and the side of hematoma (p>0.05)(Table 4).
CSDH generally occurs in elderly persons; the average age of onset is 63 years.6) The symptoms and signs of CSDH are variable and are not pathognomonic. The symptoms include change in the level of consciousness; psychomotor regression, headache and vomiting resulting from an increased intracranial pressure; decreased muscle power resulting from a decline in local movement; and dysarthria.18) The symptoms of increased intracranial pressure are common among young ages, but focal neurologic deficit and congnitive impairment are common among old ages.7) In this study, headache is common below 65 years, but cognitive impairment is common above 65 years.
A review of the patient's medical history and findings of the physical examination should lead to a diagnosis of CSDH; however, 40% of patients with this condition are likely to receive a misdiagnosis because many similar symptoms occur in other disease processes such as neurodegenerative diseases, stroke, dementia, and tumors.16) Although it is clear that neuropsychiatric symptoms are common in elderly patients with CSDH, the number of objective, datameasuring studies of CSDH presentation and outcome that have been performed from a neuropsychiatric perspective has been limited.17,26)
Dementia is an etiologically nonspecific condition that is permanent, progressive, or reversible. Dementia has profound effects on health outcomes and is associated with high use and costs of medical care.4) Therefore, the identification of potentially reversible causes of dementia is critical. More than 50 illnesses can cause dementia.20) Most frequent causes of reversible dementia are followed by metabolic and neurosurgical disorders.2,27) The prevalence of reversible dementia is reported to be lower than 1% in elderly patients.28,30) CSDH is generally seen in the elderly and is often accompanied by the type of dementia that can be reversed by simple surgery. In our study, we have demonstrated that approximately half patients with CSDH were suspected of having dementia on admission and the surgery improved above 70% of patients showing cognitive impairment. Therefore, CSDH should receive greater attention as a potential cause of reversible dementia.
On review of other studies, several risk factor used to predict postoperative clinical status after surgical treatment in CSDH patient suffering from dementia are patient age, preoperative activities of daily living (ADL) score, and preoperative clinical status. Ishikawa et al. reported patients younger than 74 years of age and/or have preoperative scores lower than 5 on the ADL, higher than 10 on the Mini-Mental Status Examination (MMSE), or higher than 9 on the hasegawa dementia scale-revised (HDS-R) will likely achieve good functional recovery.12) In current literature. Poor preoperative neurological status were used as predictor for an unfavourable outcome.10,19) However other authors reported no significant correlation between postoperative neurological outcome and preoperative clinical status.10,29,31) In our study, we have demonstrated the factors affecting postoperative cognitive status which were age and preoperaive K-MMSE.
Recurrence of CSDH after burr hole trephination has been reported in many literatures. The reported incidence of recurrence was ranged 9.2% to 26.5% and our study had a recurrence rate of 5.1%.1,22) Recently, the risk factors and pathphysiology of recurrent CSDH have been reported in the literatures.11,13,14) Risk factors for CSDH recurrence are divided into three categories. The first category is the factor related to the patient characteristics, such as old age, brain atrophy, coagulopathy, chronic alcoholism, dementia, use of anticoagulants and antiplatelet agents.3,24,31) The second category is the factor related to the CT finding of CSDH including large hematoma, bilateral CSDHs, multiple membranes in the hematoma cavity, mixed-density and highdensity hematoma.9,15,16,21,31) The third category is the factor related to the surgical procedure such as insufficient drainage of hematoma, presence of pneumocephalus, reexpansion rate of brain and early surgery when the hematoma has a poorly developed capsule.25) Our study showed that recurrence of subdural hematoma didn't have any correlation with age, the thickness of hematoma and the side of hematoma. This result may be caused by lack of the number of total patients or other risk factor.
We have found that cognitive impairment was the most common symptom in the elderly with CSDH and this tended to have a good outcome by surgery. The cognitive impairment and confusion signs mostly appear at the beginning of dementia. CSDH is an important differential diagnosis for dementia and neurodegenerative diseases, but also an important reversible cause of dementia in the elderly. If dementia is suspected in the elderly, we need to perform early neuroimaging evaluation that may allow for timely treatment of this condition to avoid a poor outcome.
Figures and Tables
References
1. Asano Y, Hasuo M, Takahashi I, Shimosawa S. Recurrent cases of chronic subdural hematoma-its clinical review and serial CT findings. No To Shinkei. 1992; 44:827–831.
3. El-Kadi H, Miele VJ, Kaufman HH. Prognosis of chronic subdural hematomas. Neurosurg Clin N Am. 2000; 11:553–567.

4. Ernst RL, Hay JW. The US economic and social costs of Alzheimer's disease revisited. Am J Public Health. 1994; 84:1261–1264.

5. Evans DA, Funkenstein HH, Albert MS, Scherr PA, Cook NR, Chown MJ, et al. Prevalence of Alzheimer's disease in a community population of older persons. Higher than previously reported. JAMA. 1989; 262:2551–2256.

6. Foelholm R, Waltimo O. Epidemiology of chronic subdural haematoma. Acta Neurochir. 1975; 32:247–250.

7. Fogelholm R, Heiskanen O, Waltimo O. Chronic subdural hematoma in adults. Influence of patient's age on symptoms, signs, and thickness of hematoma. J Neurosurg. 1975; 42:43–46.
8. Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975; 12:189–198.
9. Frati A, Salvati M, Mainiero F, Ippoliti F, Rocchi G, Raco A, et al. Inflammation markers and risk factors for recurrence in 35 patients with a posttraumatic chronic subdural hematoma: a prospective study. J Neurosurg. 2004; 100:24–32.

10. Gelabert-González M, Iglesias-Pais M, Garcia-Allut A, Martinez-Rumbo R. Chronic subdural haematoma: surgical treatment and outcome in 1000 cases. Clin Neurol Neurosurg. 2005; 107:223–229.

11. Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003; 98:1217–1221.

12. Ishikawa E, Yanaka K, Sugimoto K, Ayuzawa S, Nose T. Reversible dementia in patients with chronic subdural hematomas. J Neurosurg. 2002; 96:680–683.

13. Jeong CA, Kim TW, Park KH, Chi MP, Kim JO, Kim JC. Retrospective analysis of reoperated patients after chronic subdural hematoma surgery. J Korean Neurosurg Soc. 2005; 38:116–120.
14. Mori K, Maeda M. Surgical treatment of chronic subdural hematoma in 500 consecutive cases: clinical characteristics, surgical outcome, complications, and recurrence rate. Neurol Med Chir (Tokyo). 2001; 41:371–381.

15. Kim HY, Kwon SC, Kim TH, Shin HS, Hwang YS, Park SK. Analysis of management according to CT findings in chronic subdural hematoma. J Korean Neurosurg Soc. 2005; 37:96–100.
16. Kostanian V, Choi JC, Liker MA, Go JL, Zee CS. Computed tomographic characteristics of chronic subdural hematomas. Neurosurg Clin N Am. 2000; 11:479–489.

17. Machulda MM, Haut MW. Clinical features of chronic subdural hematoma: neuropsychiatric and neuropsychologic changes in patients with chronic subdural hematoma. Neurosurg Clin N Am. 2000; 11:473–477.
18. Iantosca MR, Simon RH. Chronic subdural hematoma in adult and elderly patients. Neurosurg Clin N Am. 2000; 11:447–454.

19. Markwalder TM, Steinsiepe KF, Rohner M, Reichenbach W, Markwalder H. The course of chronic subdural hematomas after burr-hole craniostomy and closed-system drainage. J Neurosurg. 1981; 55:390–396.

20. Mayeux R, Foster NL, Rossor M, Whitehouse PJ. The clinical evaluation of patients with dementia. In : Whitehouse PJ, editor. Dementia. Philadelphia: FA Davis;1993. p. 92–129.
21. Murakami H, Hirose Y, Sagoh M, Shimizu K, Kojima M, Gotoh K, et al. Why do chronic subdural hematomas continue to grow slowly and not coagulate? Role of thrombomodulin in the mechanism. J Neurosurg. 2002; 96:877–884.

22. Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001; 95:256–262.

23. Aoki N. Chronic subdural hematoma in infancy. Clinical analysis of 30 cases in the CT era. J Neurosurg. 1990; 73:201–205.
24. Oishi M, Toyama M, Tamatani S, Kitazawa T, Saito M. Clinical factors of recurrent chronic subdural hematoma. Neurol Med Chir (Tokyo). 2001; 41:382–386.

25. Okada Y, Akai T, Okamoto K, Iida T, Takata H, Iizuka H. A comparative study of the treatment of chronic subdural hematomaburr hole drainage versus burr hole irrigation. Surg Neurol. 2002; 57:405–409. discussion 410.

26. Oyama H, Ueda M, Inoue S, Ikeda A, Shibuya M, Katsumata T, et al. [Improvement of cognition after trepanation for the chronic subdural hematoma]. No To Shinkei. 1998; 50:249–252.
27. Tsutsumi K, Maeda K, Iijima A, Usui M, Okada Y, Kirino T. The relationship of preoperative magnetic resonance imaging findings and closed system drainage in the recurrence of chronic subdural hematoma. J Neurosurg. 1997; 87:870–875.

28. Walstra GJ, Teunisse S, van Gool WA, van Crevel H. Reversible dementia in elderly patients referred to a memory clinic. J Neurol. 1997; 244:17–22.

29. Weigel R, Schmiedek P, Krauss JK. Outcome of contemporary surgery for chronic subdural haematoma: evidence based review. J Neurol Neurosurg Psychiatry. 2003; 74:937–943.

30. Weytingh MD, Bossuyt PM, van Crevel H. Reversible dementia: more than 10% or less than 1%? A quantitative review. J Neurol. 1995; 242:466–471.
31. Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S. Independent predictors of recurrence of chronic subdural haematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg. 2003; 98:1217–1221.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download