Abstract
Objective
The mortality rate of patients with isolated head injuries is about 20-30%, whereas in multiple traumas with head injuries mortality rates can reach over 40%. The authors reviewed the multiple trauma patients with traumatic brain injury who died in emergency department and wanted to describe causes of deaths and to reconsider the role of neurosurgeons in association with trauma team.
Methods
Between July 1999 and May 2007, 48 patients who had multiple traumas were dead in the emergency department of our hospital before admission. Of them, 42 patients were selected in this study. Twenty eight were male and 14 were female. The medical and radiological records were reviewed retrospectively.
Results
The mode of accidents consisted of 18 pedestrian traffic accidents (TAs), 10 falls, 5 in car TAs, 4 motorcycle accidents, and 5 others. Initial mentality showed that alert or drowsy were 20 (47.6%), stupor 6 (14.3%), and semicoma or coma 16 (38.1%). Most frequent cause of deaths was hypovolemic shock and followed by hypoxia, severe brain swelling, and tension pneumothorax. The major causes of hypovolemia were pelvic bone fracture and abdominal bleeding. Among them, brain computed tomography (CT) and abdomen CT could be checked in 43% of patients and peripheral angiography in only 5 patients (12%).
According to the studies about the causes of trauma death, neurologic injury has been responsible for a high proportion of death, after blunt injury, presenting 27-60% of deaths.7,19) The mortality rate of patients with isolated head injuries has been reported about 11-30%, whereas in multiple traumas with head injuries mortality rates ran reach over 40%.8,9,18) The authors reviewed the multiple trauma patients with traumatic brain injury who died in the emergency department and wanted to describe causes of death and to reconsider the role of neurosurgeons in association with trauma team.
In our hospital, emergency medicine doctor or residents of surgical departments including general surgery, neurosurgery, cardiac surgery and orthopedic surgery evaluate seriously injured patients in the emergency department and an attending surgeon is called if any surgery or procedure is needed. Anesthesiologist, attending surgeon and interventional radiologist are available 24 hours per day, 7 days per week. Computed tomography (CT) room and angiography suit are located closely to the emergency department (ED) to decrease the time of evaluation.
Between July 1999 and May 2007, 48 patients who had multiple traumas were dead in the ED before admission. Of them, 42 patients were selected in this study. Six patients who presented deaths before arrival were excluded. The deaths which occurred during operation or intensive care unit were also excluded in this study. All medical records and radiological records were reviewed retrospectively. An analysis was done on the age, sex, trauma modes, neurosurgical diagnosis, combined injuries, initial mental status, initial blood pressure, times to arrival, radiologic studies, time to perform radiologic studies, time to start transfusion and causes of death for all patients.
Critical care errors were classified as management error and technical error. Management error was related error developed during initial resuscitation and subsequent survey proven to be wrong. Technical error included failure of delayed endotracheal intubation, central lines and peripheral angiographic procedures. If an error in management or technique contributed to death, the death was considered as preventable death. In addition, the authors wanted to evaluate 'talk and die' patients meaning those patients who had spoken recognizable words at some point after the head injury. For the 'talk and die' patients, we checked 'the lucid interval time' which means the time from arrival of emergency department to endotracheal intubation.
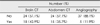
Twenty eight were male and 14 were female. The mean age was 45.5 years with a range of 4-90 years. It took average 20 minutes (10-60 minutes) to transfer from accidental spot to ED at this hospital. For the mode of accidents, pedestrian traffic accident (TA) consisted of the most including 18 (42.9%), 10 (23.8%) were in fall, 5 (11.9%) in car TA, 4 (9.5%) in motorcycle accident, and 5 in unclear causes (Table 1). Table 1 also shows major causes of death depending mode. In case of pedestrian TA, abdomen and pelvic injury were the major cause of death in 12 patients (66.7%), chest injury in 3 patients, and head injury in 3 patients. In case of fall, abdomen and pelvis injury consumed the most including 6 patients, 2 died by head injury, and 2 died by chest injury. In case of in car TA, 2 patients died by head injury, 1 by abdominal injury, and 2 by unclear causes, respectively. Initial mentality showed that alert or drowsy were 20 (47.6%), stupor 6 (14.3%), and semicoma or coma 16 (38.1%), which are listed in Table 2. Most frequent cause of death was hypovolemic shock and followed by hypoxia, severe brain swelling, and tension pneumothorax (Table 3). The major causes of hypovolemia were pelvic bone fracture and abdominal bleeding (Table 4). Brain CT could be performed on 18 patients (42.9%) and abdomen CT on 15 patients (35.7%)(Table 6). Arterial embolization was performed on only 5 patients (12%)(Table 5).
The 'talk and die' patients presented 5 (12%). The lucid interval time was identified between 2 and 183 minutes and the mean interval time was 82 minutes. Definite error was seen in 4 cases, 2 were in management error and 2 were related to endotracheal intubations. Not obvious errors, but there were events such as bradycardia, dyspnea, and seizure during CT scanning in three cases, respectively. It took average 369 minutes (16-420 minutes) from the arrival at ED to the occurrence of cardiac arrest.
As advancing of transfer systems, early recognizing of serious injuries, skill of resuscitation, and cooperation of trauma teams, death and preventable death after injury has been reduced. Many authors have reported about the death after trauma, but the death of their reports implies usually hospital death including of the death in the ED, during operation and Intensive Care Unit (ICU) care. The report about the death rate of in the ED, however, is scant. The death in the ED, sometimes, means trauma cares process urgently to the death, making impossible to operate or manage ICU care. Reviewing of previous reports and our data, we can know that preventable death has often happened in the ED. Actually according to the published reports, the preventable death has been markedly reduced from 20-23% to 2.5%.3,6,19) Gruen et al.6) reported that 5.8% of all patients died in 9 years and 2.4% of them had recognized errors resulted in deaths. In their cases, 34% of errors had occurred in the ED; 20% initial assessment and resuscitation, 14% during the secondary survey and initial diagnostic test. In our study, definitely preventable death occurred in 4 (9.5%) of all patients. There were 2 technical errors related to endotracheal intubations. One occurred in the initial assessment and the other in the secondary survey. Other two errors were related to management. All cases were ascribed to lack of recognition about the management of hypovolemia.
Some authors have described 'talk and die' patients, which means that those patients who had spoken recognizable words at some points after head injury that is a verbal score of 3 and above on the Glasgow Coma Scale, then deteriorate and progressed to death.5,14-16) It's incidence has been reported from 2 to 7%. According to Goldschlager's report, the incidence of 'talk and die' patients was 2.6% and causes of death were mainly acute subdural hematoma (SDH) and brain contusion with swelling. In our study, there were 9 patients who could talk in the early course of ED care. But, pure 'talk and die' patients were 5 (11.9%). Of 5 patients, 4 patients had acute SDHs and one scant traumatic subarachnoid hemorrhage and intracerebral hematoma. The cause of death was hypovolemic shock in 4 patients and brain swelling in one patient in our study. The difference between our study and others might be ascribed to the facts as follows; 1) our study only included the death occurred in the ED, but others the death occurred during operation and ICU care. 2) Patients of our study had multiple traumas rather than isolated head trauma.
Central nervous system (CNS) injury has been a major cause of death after trauma, presenting 50-65%.3,4,19) However, in case of multiple traumas, non CNS injuries might be a major cause of death like as vessel injury, bowel injury or pelvic bleeding. In Siegel's report,18) one of the largest series of blunt head injuries published, extracranial injuries were found in about 60% of patients. The mortality rate with isolated brain injury was 11.1%, but when any extracranial injury was added, it was increased to 21.8%. The most frequent cause of the mortality was great vessel injuries (50%), followed by liver, bowel, lung, spleen, spine, femur fracture, and pelvic fractures.
In authors' study, the highest cause of death was not the CNS injury but, hypovolemic shock. The causes of hypovolemia were pelvic bleeding, abdominal bleeding, and hemothorax.
These findings are similar to other reports. According to the report, retrospective study of 1,000 deaths from injury in England, hemorrhage was a major cause of death in non CNS injury.3) The reason of increasing mortality in multiple traumas rather than isolated head injury was ascribed to secondary brain insult. Hypotension and hypoxemia have been known as major causes of secondary brain injury in severely injured patients. A recent study presented that only brief episode less than 10 minutes of hypotension was associated with an increased mortality and morbidity.20) Therefore, early detection and prevention of hypotension as well as treatment is very important in head injury patients with multiple traumas.
The bleeding from pelvic injury (26.2%) was more than abdominal injury (23.8%) in this study. For detection of abdominal bleeding, paracentasis, peritoneal lavage, ultrasonography, and mutislice computed tomography have been used. Pelvic fracture is often the cause of severe extraperitoneal hemorrhage. The injuries of presacral veins, or internal iliac artery or its branches often result in this extraperitoneal hemorrhage.17) The mortality associated with pelvic fracture is 7 to 15%.1,13) The arterial bleeding due to pelvic fracture can be treated using transcatheter arterial embolization (TAE).10)
Some authors have demonstrated that it is very effective to control bleeding as well as diagnosis with success rate of 87-100%.2,11,12) Despite high success rate of TAE, the time from arrival in the ED to arrival in the angiography suit is very important. Agolini et al.2) reported that if the patients were in the angiography suit within 3 hours, the mortality rate was 14%, however, after 3 hours increased to 75%.
Only 5 patients could undergo TAE in our study. Four of them had extraperioneal hemorrhage from both internal iliac arteries and one hemothorax. The mean time from arrival in the ED to arrival in the angiography suit was 192 minutes in 4 patients with pelvic fracture. The attributable to the causes of delay were the failure of early detection of hemorrhage, the lack of understanding of arterial embolization, delayed calling to intervention team and failure in coordination between the trauma teams.
The major cause of deaths of patients who had traumatic brain injury with multiple traumas in the ED was not brain injury but hypovolemic shock. So, adequate and timely management is very important for these patients. Early detection and treatment of bleeding causes by using multimodality consisting of brain CT, abdomen or chest CT, ultrasonography, and peripheral angiography, can decrease the mortality. In addition, it is absolutely important to cooperate between the trauma teams.
References
2. Agolini SF, Shah K, Jaffe J, Newcomb J, Rhodes M, Reed JF 3rd. Arterial embolization is a rapid and effective technique for controlling pelvic fracture hemorrhage. J Trauma. 1997; 43:395–399.

3. Anderson ID, Woodford M, de Dombal FT, Irving M. Retrospective study of 1000 deaths from injury in England and Wales. Br Med J (Clin Res Ed). 1988; 296:1305–1308.

4. Baker CC, Oppenheimer L, Stephens B, Lewis FR, Trunkey DD. Epidemiology of trauma deaths. Am J Surg. 1980; 140:144–150.

5. Goldschlager T, Rosenfeld JV, Winter CD. 'Talk and die' patients presenting to a major trauma centre over a 10 year period: a critical review. J Clin Neurosci. 2007; 14:618–623. discussion 624.

6. Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg. 2006; 244:371–380.
7. Hodgson NF, Stewart TC, Girotti MJ. Autopsies and death certification in deaths due to blunt trauma: what are we missing? Can J Surg. 2000; 43:130–136.
8. Lehmann U, Rickels E, Krettek C. [Multiple trauma with craniocerebral trauma. Early definitive surgical management of long bone fractures?]. Unfallchirurg. 2001; 104:196–209.
9. Lobato RD, Cordobes F, Rivas JJ, de la Fuente M, Montero A, Barcena A, et al. Outcome from severe head injury related to the type of intracranial lesion. A computerized tomography study. J Neurosurg. 1983; 59:762–774.
10. Miller BS, Harper WP, Gillies RM, Sonnabend DH, Walsh WR. Biomechanical analysis of five fixation techniques used in glenohumeral arthrodesis. ANZ J Surg. 2003; 73:1015–1017.

11. Panetta T, Sclafani SJ, Goldstein AS, Phillips TF, Shaftan GW. Percutaneous transcatheter embolization for massive bleeding from pelvic fractures. J Trauma. 1985; 25:1021–1029.
12. Piotin M, Herbreteau D, Guichard JP, Houdart E, Reizine D, Aymard A, et al. Percutaneous transcatheter embolization in multiply injured patients with pelvic ring disruption associated with severe haemorrhage and coagulopathy. Injury. 1995; 26:677–680.

13. Poole GV, Ward EF, Muakkassa FF, Hsu HS, Griswold JA, Rhodes RS. Pelvic fracture from major blunt trauma. Outcome is determined by associated injuries. Ann Surg. 1991; 213:532–538. discussion 538-539.

14. Ratanalert S, Chompikul J, Hirunpat S. Talked and deteriorated head injury patients: how many poor outcomes can be avoided? J Clin Neurosci. 2002; 9:640–643.

15. Reilly PL, Graham DI, Adams JH, Jennett B. Patients with head injury who talk and die. Lancet. 1975; 2:375–377.

16. Rockswold GL, Leonard PR, Nagib MG. Analysis of management in thirty-three closed head injury patients who "talked and deteriorated". Neurosurgery. 1987; 21:51–55.

17. Schmoker JD, Zhuang J, Shackford SR. Hemorrhagic hypotension after brain injury causes an early and sustained reduction in cerebral oxygen delivery despite normalization of systemic oxygen delivery. J Trauma. 1992; 32:714–720. discussion 721-712.

18. Siegel JH. The effect of associated injuries, blood loss, and oxygen debt on death and disability in blunt traumatic brain injury: the need for early physiologic predictors of severity. J Neurotrauma. 1995; 12:579–590.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download