Abstract
Objective
The aim of this study was to examine the significance of pupillary light reflex (PLR) during barbiturate coma therapy (BCT) against severe brain swelling.
Methods
Between January 2003 and October 2007, 28 patients (traumatic brain injury: 15) underwent BCT because of maintained severe brain swelling after operation. All the patients maintained 3-6th wave per minute activity on electro-encephalography, and PLR were checked every 2 hours during BCT. The patient's performance was checked using Glasgow outcome scale (GOS) at the average 19.6 days (1-60 days) after BCT.
Results
Twenty one patients had PLR at the start of BCT. Among 21 patients, 12 patient's PLR were vanished during BCT. Nine of 12 patients were dead (GOS=1), two had severe disability (GOS=2), and one stayed persistent vegetative state (GOS =3). But other nine patient's group, who showed prompt PLR continuously during BCT, got more improved GOS, compared with PLR vanished patient's group; 7 of 9 patients ranked more than GOS score 3.
Figures and Tables
FIGURE 1
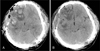
A 33-year-old male patient, glasgow coma scale (GOS) score 7, was admitted due to traumatic brain injury and operated. To control increased intracranial pressure, barbiturate coma therapy was done and his final glasgow outcome scale score was 5. A: Effacement of ambient cistern and midline shifting is remained after decompressive craniectomy. B: Effacement of ambient cistern and midline shifting is recovered after 48 hours of barbiturate coma therapy on brain computed tomography examination.
References
1. Brodersen P, Jorgensen EO. Cerebral blood flow and oxygen uptake, and cerebrospinal fluid biochemistry in severe coma. J Neurol Neurosurg Psychiatry. 1974; 37:384–391.

2. Cormio M, Gopinath SP, Valadka A, Robertson CS. Cerebral hemodynamic effects of pentobarbital coma in head-injured patients. J Neurotrauma. 1999; 16:927–936.

3. Langfitt T, Obrist W. Cerebral blood flow and metabolism after intracranial trauma. In : Krayenbuhl H, editor. Progress in Neurological surgery. Basel: S. Karger;1981. p. 14–48.
4. Lee MA, Deppe SA, Sipperly ME, Barrette RR, Thompson DR. The efficacy of barbiturate coma in the management of uncontrolled intracranial hypertension following neurosurgical trauma. J Neurotrauma. 1994; 11:325–331.

5. Lowenstein DH, Aminoff MJ, Simon RP. clinical experience with 14 patients. Neurology. 1988; 38:395–400.
6. Marshall LF, Smith R, Shapiro H. The outcome with aggressive treatment in severe head injuries. Part I. Significance of intracranial pressure monitoring. J Neurosurg. 1979; 50:20–25.
7. Mary JM, Richard AH, Pamela CC. Lippincott's Illustrated Review. Pharmacology. ed 2. Philadelphia: Lippincott Williams & Wilkins;2000. p. 94.
8. Messeter K, Nordstrom CH, Sundbarg G, Algotsson L, Ryding E. Cerebral hemodynamics in patients with acute severe head trauma. J Neurosurg. 1986; 64:231–237.

9. Michenfelder JD, Milde JH. Influence of anesthetics on metabolic, functional and pathological responses to regional cerebral ischemia. Stroke. 1975; 6:405–410.

10. Osorio I, Reed RC. Treatment of refractory generalized tonic-clonic status epilepticus with pentobarbital anesthesia after high-dose phenytoin. Epilepsia. 1989; 30:464–471.

11. Sato M, Niiyama K, Kuroda R, Ioku M. Influence of dopamine on cerebral blood flow, and metabolism for oxygen and glucose under barbiturate administration in cats. Acta Neurochir (Wien). 1991; 110:174–180.

12. Rea GL, Rockswold GL. Barbiturate therapy in controllied intracranial hypertension. Neurosurgery. 1983; 12:401–404.
13. Winer J, Rosenwasser R, Jimenez F. Electroencephalographic activity and serum and cerebrospinal fluid pentobarbital levels in determining the therapeutic endpoint during barbiturate coma. Neurosurgery. 1991; 29:739–742.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download